Our Previous Samples
NRS 493 Professional Capstone Practicum Essays GCUNRS 493 Topic 1 Individual Suc ...
NRS 493 Professional Capstone Practicum Essays GCU
NRS 493 Topic 1 Individual Success Plan (ISP)
REQUIRED PRACTICE HOURS: 100 Direct Clinical Experience (50 hours community/50 hours leadership) – 25 Indirect Clinical Experience Hours.
Application-based Learning Course AssignmentsList of Current Course ObjectivesNumber of Clock Hours Associated with Each AssignmentAssignment Date DueSelf-Assessment: GCU RN-to-BSN University Mission Critic Competencies and Programmatic Domains Competencies(see Appendix A)WEEK 1Agreement between Grand Canyon University and HillCrest Hospital Develop ISP and share ideas with mentor. Submit documentation for Course Mentor identification process Plan for a capstone research project105/16/2021MCI-MC5 Domains 1.1: 2.3:Course mentor11:59:594.1: 5.1Identification andDiscussionapproval processtopic duePre-conference Individual Successdates#1 5/12/21Plan11:59:59Capstone change#2 5/14/21project topics11:59:59Lopes Activity TrackerReflective JournalDiscussion topic 1&2WEEK 2Identify a topic problem, and opportunities to improve patient care, and outcomes, within a clinical practice setting. Determine evidence? based solutions Identify strategies for logistical Implementation of a105/23/202111:59:59 Discussion topic due dates#1 5/19/2111:59:59MCI-M5 Domains 1.1: 1.2: 1Capstone Topic Summary,1.4 :2.1:2.2: 2.3 3.1:3.2: 3.3 34.1: 4.3: 5.1: 5.2Selection, andApprovalLopes ActivityTrackerReflective JournalDiscussion topic 1&2solution. Use the PICOT process in analyzing a clinical problem or organization issue.#2 5/21/2111:59:59WEEK 31. Evaluate evidence-105/30/2021MC1-MC5: Domai.3ns 1.1:1.2:1.3: 1.4: 2.1: 2.2:2.3: 3.1:4.14.2: 4.3: 5.1:5MC1-MC5 Domains 1.1: 1.21.4: 1.5: 2.1: 2.2;2.3: 3.1: 4.14.2: 4.3: 5.1: 5.2
MC1-MC5 Domains 1.1: 1.2
1.5: 2.1: 2.2: 2.3: 3.1: 3.2: 3.
PICOT Statement Paper (Discussion with mentor)Lopes Activity Trackerbased research and other appropriate resources to inform the development of a change plan.2. Identify strategies for logistical11:59:59Discussion topic due dates#1 5/26/21Discussion topic 1&2Reflective journalimplementation of proposed solutions.3. Demonstrate the11:59:59#2 5/28/21Benchmark Capstone Change Project Objectivesability to evaluate levels of evidence into a concise format.4. Integrate evidence,11:59:59clinical judgment, inter-professionalperspectives, and patientpreferences in planning,implementing, andevaluating outcomes ofcare.WEEK 41. Evaluate evidence-106/06/2021Evidence-Based Practice Proposal Development Plan 2Literature Evaluation Tablebased research and other appropriate resources for the development of a change plan.2. Identify strategies for logistical11:59:59Discussion topic due dates#1 6/2/21Lopes Activity tracker Reflective journalimplementation of proposed solutions.3. Demonstrate the11:59:59#2 6/4/21Discussion topic 1&2Capstone Change Project Outcomesability to evaluate levels of evidence into a concise format.4. Integrate evidence, clinical judgment, inter-11:59:59professionalperspectives, andpatients’ preferences inplanning, implementing,and evaluatingoutcomes of care.WEEK 5Evidence-BasedIdentify the objectives, strategies, and best outcomes of the106/13/2111:59:59Practice Proposalevidence-based practice proposal. Mapped out steps to implement the strategies for change proposalFind resources to organize and implement the proposal.Establish an evaluation plan for change proposal effectiveness in ensuring adequate health promotion and disease prevention
Discussion4.2; 4.3: 5.1:5.2: 5.3:5.4:MC1-MC5 Domains 1.1: 1.21.4; 1.5: 2.1; 2.2: 2.3: 3.1: 3.3.3: 3.4: 4.1: 4.2: 4.3: 5.1:5.25.3: 5.4:
MC1-MC5 Domains-1.1, 1.2
1.4: 2.1: 2.2: 2.3, 2.4: 3.1: 3.
3.3: 3.4: 4.1: 4.2, 4.3: 4.4; 4.
5.1: 5.2: 5.3: 5.4: 5.5
Projecttopic dueDevelopment anddatesImplementation Plan 1 (Practice#1 6/9/21Hours Completion11:59:59Statement lopes activity tracker#2 6/11/2111:59:59Reflective journalDiscussion topic1&2Midterm Evaluationof studentMid-ConferenceWEEK 6Identify the objectives, strategies, and best outcomes of the evidence-based practice proposal. Find resources to organize and implement the proposal. Analyzing how current research supports the PICOT, as well as identifies what is known and what is not known in the evidence.106/20/202111:59:59discussion topic due dates#1 6/16/2111:59:59#2 6/18/21
11:59:59
Evidence-BasedPractice ProposalProjectDevelopment andImplementationPlan 2 (LiteratureReview withMentorCapstone ChangeProject resourcesReflective journalLopes activitytrackerDiscussion topic1&2WEEK 7Ability to identify ways106/27/2021Change Proposal Project Evaluation and Dissemination Planof evaluating a proposed solution. Assess variables and outcomes before and after project implementation using11:59:59Discussion topic due datesLopes activity trackerbasic statistics. Address plans of making#1 6/23/21Reflective journal Discussion topic 1&2evidence for change proposal known. Employ excellent communication and11:59:59#2 6/25/2111:59:59teamwork withinterdisciplinarymembers to deliver the best evidence-based patient care.WEEK 8 Change Proposal Project Evaluation and Dissemination Plan 2Practice Hours Completion Statement Reflective journal Lopes activity tracker Discussion topic 1&2Apply evidence-based research steps and processes required as the foundation to address clinically oriented problem or issue in future practice. Address plans of making evidence for change proposal known. Employ excellent communication and teamwork with interdisciplinary members to deliver the best evidence-based patient care.107/04/202111:59:59 Discussion topic due dates#1 6/30/2111:59:59#2 7/2/21
11:59:59
MC1-MC5 Domains -1.1, 1.21.3, 1.4, 2.1, 2.2, 2.3, 2.4, 3.13.2, 3.3, 3.4, 4.1, 4.2, 4.3, 4.44.5, 5.1, 5.2, 5.3, 5.4, 5.5WEEK 9Evidence-Based Practice Proposal Project 1(Capstone Project Change Proposal)Lopes activity tracker Reflective journalDiscussion topic 1&2Present a professional comprehensive change initiative. Apply new knowledge and skill to nursing practice watching the process of evidence- based research utilization by nursing staff. Analyze research studies for use as evidence-based practice in healthcare settings. Be an active interprofessional collaborator in leadership, skills and decision-making to provide in providing high-quality patient careKnow the organization and other barriers that can derail change proposals to affect10711/202111:59:59 Discussion topic due dates#1 7/7/2111:59:59#2 7/9/21
11:59:59
health care delivery and practice. Effectively communicate and exemplify good leadership traits in ensuring a successful implementation of the change initiative.WEEK 10Evidence-Based Practice Proposal Project 2Benchmark & Professional Capstone and Practicum Reflective Journal Individual Success PlanLopes activity trackerPost Conference
Present a professional comprehensive change initiative. Apply new knowledge and skill to nursing practice watching the process of evidence-based research utilization by nursing staff. Analyze research studies for use as evidence-based practice in healthcare settings. Be an active interprofessional collaborator in leadership, skills and decision-making to provide in providing high-quality patient careKnow the organization and other barriers that can derail change proposals to affect health care delivery and practice.Effectively communicate and exemplify good leadership traits in ensuring a successful implementation of the change initiative.
107/18/202111:59:59 Discussion topic due dates#1 7/14/2111:59:59#2 7/16/21
11:59:59
MC1-MC5 Domains -1.1, 1.21.3, 1.4, 2.1, 2.2, 2.3, 2.4, 3.13.2, 3.3, 3.4, 4.1, 4.2, 4.3, 4.44.5, 5.1, 5.2, 5.3, 5.4, 5.5Personal evaluation with mentor7/18/2111:59:59Scholarly Activity7/18/2111:59:59Comprehensive Log100.7/11MC2; MC5of Practice Immersion Hours1:59:59Domain 1.1; 1.2; 1.3; 1.4; 1.5By typing in his/her signature below, the student agrees to have read, understood, and be accountable for the instructions, assignments, and hours shown above and that all questions have been satisfactorily answered by the faculty.
Preceptors will sign upon initial receipt and at the end of the course to confirm that assignments have been complete with your guidance.
Student SignatureName:TLDate:5/14/2021Mentor Signature [Upon Initiation of Course]Name:CTDate:5/14/21Mentor Signature [Upon Completion of Course]Name:Week 10 mentor signs when date assignment completed is filled in.Date:APPENDIX A:
NRS 493 Professional Capstone Practicum Essays GCU: GCU RN-to-BSN Domains & Competencies
•University’s Mission Critical Competencies
How does this Individual Success Plan support the GCU Mission?
MC1: Effective Communication: Therapeutic communication is central to baccalaureate nursing practice. Students gain an understanding of their ethical responsibility and how verbal and written communication affects others intellectually and emotionally. Students begin to use nursing terminology and taxonomies within the practice of professional and therapeutic communication.
Courses require students to write scholarly papers, prepare presentations, develop persuasive arguments, and engage in discussion that is clear, assertive, and respectful.
MC2: Critical Thinking: Courses require students to use critical thinking skills by analyzing, synthesizing, and evaluating scientific evidence needed to improve patient outcomes and professional practice.
MC3: Christian Worldview: Students will apply a Christian worldview within a global society and examine ethical issues from the framework of a clearly articulated system of professional values. Students will engage in discussion of values-based decisions made from a Christian perspective.
MC4: Global Awareness, Perspectives, and Ethics: The concept of global citizenship is introduced to baccalaureate students in the foundational curriculum. Some courses will focus on the human experience across the world health continuum. The World Health Organization (WHO) definitions of health, health disparities, and determinants of health are foundational to nursing practice.
MC5: Leadership: Students will apply a Christian worldview within a global society and examine ethical issues from the framework of a clearly articulated system of professional values. Students will engage in discussion of values-based decisions made from a Christian perspective.

NRS 493 Professional Capstone Practicum Essays GCU Domains and Competencies
How does this Individual Success Plan support the Program Domains and Competencies?
NRS 493 Professional Capstone Practicum Essays GCU Domain 1: Professional Role
Graduates of Grand Canyon University’s RN-BSN program will be able to incorporate professional values to advance the nursing profession through leadership skills, political involvement, and life-long learning.
Competencies:
- : Exemplify professionalism in diverse health care
- : Manage patient care within the changing environment of the health care
- : Exercise professional nursing leadership and management roles in the promotion of patient safety and quality
- : Participate in health care policy development to influence nursing practice and health
- : Advocate for autonomy and social justice for individuals and diverse
NRS 493 Professional Capstone Practicum Essays GCU Domain 2: Theoretical Foundations of Nursing Practice
Graduates of Grand Canyon University’s RN-BSN program will have acquired a body of nursing knowledge built on a theoretical foundation of liberal arts, science, and nursing concepts that will guide professional practice.
Competencies:
- : Incorporate liberal arts and science studies into nursing
- : Comprehend nursing concepts and health
- : Understand and value the processes of critical thinking, ethical reasoning, and decision making.
NRS 493 Professional Capstone Practicum Essays GCU Domain 3: Nursing Practice
Graduates of Grand Canyon University’s RN-BSN program will be able to utilize the nursing process to provide safe quality care based on nursing best practices.
Competencies:
- : Utilize the nursing process to provide safe and effective care for patients across the health-illness continuum: promoting, maintaining, and restoring health; preventing disease; and facilitating a peaceful
- : Implement patient care decisions based on evidence-based
- : Provide individualized education to diverse patient populations in a variety of health care
- : Demonstrate professional standards of
NRS 493 Professional Capstone Practicum Essays GCU Domain 4: Communication/Informatics
Graduates of Grand Canyon University’s RN-BSN program will be able to manage information and technology to provide safe quality care in a variety of settings. In addition, graduates will be able to communicate therapeutically and professionally to produce positive working relationships with patients and health care team members.
Competencies:
- : Utilize patient care technology and information management
- : Communicate therapeutically with
- : Professionally communicate and collaborate with the interdisciplinary health care teams to provide safe and effective care.
NRS 493 Professional Capstone Practicum Essays GCU Domain 5: Holistic Patient Care
Graduates of Grand Canyon University’s RN-BSN program will be able to provide holistic individualized care that is sensitive to cultural and spiritual aspects of the human experience.
Competencies:
- : Understand the human experience across the health-illness
- : Assess for the spiritual needs and provide appropriate interventions for individuals, families, and groups.
- : Provide culturally sensitive
- : Preserve the integrity and human dignity in the care of all
Planning is the key to successful completion of this course and program-related objectives. The Individual Success Plan (ISP) assignment requires early collaboration with the course faculty and your course preceptor. Students must establish a plan for successful completion of
- The required 50 community direct clinical practice experience hours, 50 leadership direct clinical practice hours, and 25 indirect clinical experience hours.
- Completion of work associated with program competencies.
- Work associated with completion of the student’s capstone project change proposal.
Students will use the “Individual Success Plan” to develop an individual plan for completing practice hours and course objectives. As a part of this process, students will identify the number of hours set aside to meet course goals.
Student expectations and instructions for completing the ISP document are provided in the “NRS-493 Individual Success Plan” resource, located in the Study Materials and in the assignment instructions.
Students should apply concepts from prior courses to critically examine and improve their current practice. Students are expected to integrate scholarly readings to develop case reports that demonstrate increasingly complex and proficient practice.
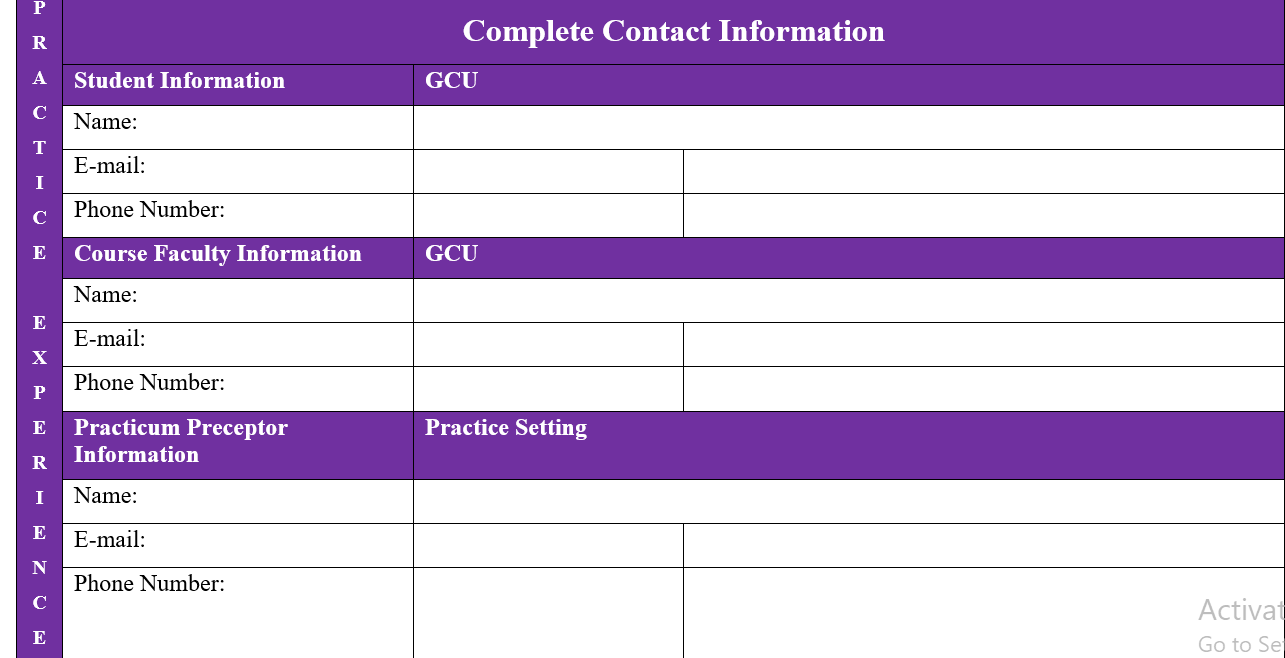
After the ISP has been developed by the student and approved by the course faculty, students will initiate a preconference with the faculty and preceptor to review the ISP.
You are not required to submit this assignment to LopesWrite.
NRS 493 Professional Capstone Practicum Essays GCU
NRS 493 Topic 1 Practice Experience Conference (Pre-Conference)
Students are required to initiate a preconference that will occur during the first week of class and must include the faculty member and the preceptor. Conferences may be conducted face-to-face or via synchronous technology such as Skype, Zoom, or GoToMeeting.
The student, preceptor, and faculty must be present at the conference. The student and preceptor will complete the “Practice Experience Conference Form (Preconference)” and the student will submit it to the instructor in LoudCloud after the conference has taken place.
You are not required to submit this assignment to LopesWrite.
NRS 493 Professional Capstone Practicum Essays GCU – NRS 493 Topic 1 DQ 1
Identify two GCU Library scholarly databases that will help you find the best research articles to support your capstone project change proposal. Discuss why these two databases are better than Google Scholar or a general Internet search.
NRS 493 Professional Capstone Practicum Essays GCU – NRS 493 Topic 1 DQ 2
The Institute of Medicine has stated a goal that 90% of practice be evidence-based by 2020. According to HealthyPeople.gov, the United States is currently at approximately 15%. Discuss two barriers that might hold nursing practice from achieving this goal and suggest ways in which identified barriers may be addressed.
NRS 493 Professional Capstone Practicum Essays GCU – Topic 2 DQ 1
During your practicum, determine what clinical problem or issue the organization is facing. Discuss two implications for nursing.
NRS 493 Professional Capstone Practicum Essays GCU – NRS 493 Topic 2 DQ 2
What is the main issue for your organization in addressing a solution to evidence-based nursing practice? Discuss what might be the first step in addressing and resolving this issue.
NRS 493 Professional Capstone Practicum Essays GCU – NRS 493 Topic 3 DQ 1
Submit a summary of six of your articles on the discussion board. Discuss one strength and one weakness for each of these six articles on why the article may or may not provide sufficient evidence for your practice change.
NRS 493 Topic 3 DQ 1 Example Approach
Kristler et al., (2018)
Strengths: The journal was informative on the demographic characteristics, methods used were survey and sampling, included data that I need for the focus of factors related to falls, with a time period. The data analysis is useful, and the limiters are identified.
Weakness: The target was more geared to CKD and the elderly results.
Ø CDC, (2021)
Strengths: The facts on falls and the statistical data are credited related to the CDC is the source. Falls in the U.S. is a comparison that is needed in the study. The education/ teaching tools are available to pull from for the project.
Weakness: There are many variables to search through to retrieve data, information, and are not complex to a specific age group for this journal.
Ø United Health Foundation, (2022)
Strengths: This website is detailed oriented toward the focus. The content is supportive of the data to Texas and falls age 65 and older. The references give this site credibility and therefore will be useful.
Weakness: The journal has information as a secondary source, and there are no comparisons as a peer-reviewed journal has methods and comparisons, limiters to search for that are user friendly.
Ø Ximenes et al., (2021)
Strengths: This journal is a systematic review, that includes interventions that are educational, peer-reviewed, and had methodological aspects of falls to offer assessments of the studies in hospitals, nursing homes, and specifically noted follow-up at home that utilized home visits. The focus of the research is home visits after hospitalization, and observance data comparisons. This provides the researcher with evidence-based information.
Weakness: The journal article showed the weaknesses, however, the focus only consisted of four risk factors. There were outliers of influence identified with all ages and therefore not specific to the target age.
Ø Bjerk, M., Brovold, T., Davis, J., & Bergland, A. (2019)
Strengths: The research literature review is clearly stated. The variables (dependent and independent) are identified clearly; as well as the statistical data for the analysis and descriptive results were identified. The research design is clearly stated. There is validity.
Weakness: Interviews were used and sometimes can be biased without a control group via observation. This is a secondary analysis of data and a randomized control trial identified as “elsewhere”. There were more women than men, and more education interventions are needed.
Ø Ozen, B., & Demir, G. (2020).
Strengths: The article is original, contains key elements such as statistics, methodology, and results. The risk factors were identified. The study was for sleepiness, however, there is data to support the researchers’ PICOT. The results were compared to previous studies.
Weakness: The research was geared to sleepiness in 65 and older adults. Educational interventions were not descriptive. There are no variables (this is a descriptive-relational study). There could be more studies that can continue the study searching more focus to specifics.
References
Bjerk, M., Brovold, T., Davis, J., & Bergland, A. (2019). Evaluating a falls prevention intervention in older home care recipients: a comparison of SF?6D and EQ?5D. Quality of life research. 28:3187–3195. https://doi.org/10.1007/s11136-019-02258-x
CDC. (2021). Facts about falls. Centers for Disease Control and Prevention. Retrieved February 22, 2022, from https://www.cdc.gov/falls/facts.html
Kistler, B., Khubchandani, J., Jakubowicz, G., Wilund, K., & Sosnoff, J. (2018). Falls and Fall-Related Injuries Among US Adults Aged 65 or Older With Chronic Kidney Disease. Preventing chronic disease, 15, E82. https://doi.org/10.5888/pcd15.170518
Ozen, B., & Demir, G. (2020). A determinant for falls and risk factors in the elderly: Daytime sleepiness. Volume 13 | Issue 1| Page 732. http://www.internationaljournalofcaringsciences.org/docs/81_ozen_original_13_1.pdf
United Health Foundation. (2022). Explore falls – ages 65+ in Texas: 2021 senior report. America’s Health Rankings. Retrieved February 22, 2022, from https://www.americashealthrankings.org/explore/senior/measure/falls_sr/state/TX
Ximenes, M., Brandao, M., de Araujo, T., Neto, N., Barros, L., Caetano, J. (2021). Effectiveness of educational interventions for fall prevention: a systematic review. Texto & Contexto – Enfermagem [internet]. 2021, v. 30:e20200558. Available from: <https://doi.org/10.1590/1980-265X-TCE-2020-0558>. Epub 30 Aug 2021. ISSN 1980-265X. https://doi.org/10.1590/1980-265X-TCE-2020-0558
NRS 493 Topic 3 DQ 1 Example Approach 2
Garcia et al (2019) found that burnout among nurses have a direct negative impact on the quality-of-care patients receive, particularly in terms of compromising their safety. The nurses get prone to medical errors because the focus, concentration and critical thinking skills gets impaired due to the psychological and physical exhaustion. The paper is strong on developing and defending the causal link on the variables under discussion. It is a review of published materials and not statistical research in itself.
Kelly et a l (2021) explains how when burnout inducing condition prevail in a hospital, clinic or nurses’ working environment not just the patients’ care but also the entire organization is affected. The paper does a great job in highlight the broader impact of nurse burnout and not just restricting it to the effects on patients. This is important because it drags the attention of management of medical establishments to take the issue of nurse burnout seriously because the operation of the organization can be crippled. The weakness is that the study surveyed nurses from three facilities only, opening up the study to question about whether it was representative enough.
Mua (2019) explains in details how investing in improving the work condition for nurses so that their burnout is dealt with has a direct impact on improving the experience of patients under their care. It finds that nurses who are motivated to work, has time to refresh and replenish and who have workload evenly distributed tend to give better quality service. The paper is effective in vouching for dealing with nurse burnout in a progressive and effective manner. It however does not highlight how patient behaviors also tend to frustrate nurses into burnout even if some of the conditions for the nurses are addressed.
Sasangohar et al. (2020) examines how the physical and psychological impacts of COVID-19 translated into stressing and overstretching ICU nurses, causing them to experience burnout. The article’s strength is that it lays bare how nurses experience burnout when they get overstretched by huge influx of patients into hospitals needing intensive care. This perspective is accurate. The weakness is that the paper uses pandemic times which has been an emergency to suggest conclusions which it purports to be generalized.
Shah et al (2021) discusses the how widespread the problem of nurse burnout is among nurses in the United States and what factors contribute to it. It found that the up to 31.5% nurses who report to have left their job cite burnout as the principal reason. Hospitals and clinics with 20 hour a week working schedule setting were associated with greater odds of burnout. The strength of this article is that it clearly links the factors to the outcome which forms the basis for its conclusion. The weakness is that it only sampled 50,000 nurses to represent 3.9 million people, a sample I think is too small to be representative.
Kelly et al. (2021) use evidence-based studies to build a case of how nurses can deal with burnout and shield themselves from it. The detailed suggestion highlight how nurses can reduce their pre-exposure to physical and emotional exhaustion that drains the work drive. The weakness is that articles reviewed to generate the suggestions seem so limited to give credible conclusions that can be relied upon.
References
Garcia, C. D. L., Abreu, L. C. D., Ramos, J. L. S., Castro, C. F. D. D., Smiderle, F. R. N., Santos, J. A. D., & Bezerra, I. M. P. (2019). Influence of burnout on patient safety: systematic review and meta-analysis. Medicina, 55(9), 553.
Kelly, L. A., Gee, P. M., & Butler, R. J. (2021). Impact of nurse burnout on organizational and position turnover. Nursing outlook, 69(1), 96-102.
Kelly, L. A., Weston, M. J., & Gee, P. M. (2021). A Nurse Leader’s Guide to Reducing Burnout: Strategies to Improve Well-Being. Nurse Leader, 19(5), 467-473.
Mua, A. (2019). Compounding Effects of Reducing Nurse Burnout and How It Can Produce an Increase in Patient Safety and Satisfaction.
Sasangohar, F., Jones, S. L., Masud, F. N., Vahidy, F. S., & Kash, B. A. (2020). Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesthesia and analgesia.
Shah, M. K., Gandrakota, N., Cimiotti, J. P., Ghose, N., Moore, M., & Ali, M. K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA network open, 4(2), e2036469-e2036469.
NRS 493 Professional Capstone Practicum Essays GCU – NRS 493 Topic 3 DQ 2
Name two different methods for evaluating evidence. Compare and contrast these two methods.
NRS 493 Professional Capstone Practicum Essays GCU – Topic 4 DQ 1
Why is understanding the health care system at the local level important to consider when planning an EBP implementation? Conduct research and solicit anecdotal evidence from your course preceptor that you will take into consideration for your own change project.
NRS 493 Professional Capstone Practicum Essays GCU -NRS 493 Topic 4 DQ 2
Compare and contrast two change theories, and determine which theory makes the most sense for implementing your specific EBP intervention. Why? Has your preceptor used either theory, and to what result?
NRS 493 Professional Capstone Practicum Essays GCU – NRS 493 Topic 5 DQ 1
Stakeholder support is necessary for a successful project implementation. Consider your internal stakeholders, such as the facility, unit, or health care setting where the change proposal is being considered, and your external stakeholders, like an individual or group outside the health care setting. Why is their support necessary to the success of your change proposal, and how you will go about securing that support?
NRS 493 Professional Capstone Practicum Essays GCU – NRS 493 Topic 5 DQ 2
Technology is integral to successful implementation in many projects, through either support or integration or both. Name at least one technology that could improve the implementation process and the outcomes of your capstone project change proposal. Do you plan to use this technology? If not, what are the barriers that prevent its use?
NRS 493 Professional Capstone Practicum Essays GCU – Topic 6 DQ 1
After discussion with your
READ MORE >>
NRS 493 RS4 Literature Evaluation TableLiterature Evaluation TableCriteriaArticl ...
NRS 493 RS4 Literature Evaluation Table
Literature Evaluation Table
CriteriaArticle 1Article 2Article 3Article 4Author, Journal (Peer-Reviewed), andPermalink or Working Link to Access Article
Zheng, F., Liu, S., Liu, Y., & Deng, L. (2019). Effects of an outpatient diabetes self-management education on patients with type 2 diabetes in China: a randomized controlled trial. Journal of diabetes research, 2019. https://doi.org/10.1155/2019/1073131
Nassar, C. M., Montero, A., & Magee, M. F. (2019). Inpatient diabetes education in the real world: an overview of guidelines and delivery models. Current diabetes reports, 19(10), 1-8. https://doi.org/10.1007/s11892-019-1222-6
Lee, S. K., Shin, D. H., Kim, Y. H., & Lee, K. S. (2019). Effect of diabetes education through pattern management on self-care and self-efficacy in patients with type 2 diabetes. International journal of environmental research and public health, 16(18), 3323. https://doi.org/10.3390/ijerph16183323
Chatterjee, S., Davies, M. J., Heller, S., Speight, J., Snoek, F. J., & Khunti, K. (2018). Diabetes structured self-management education programs: a narrative review and current innovations. The Lancet Diabetes & Endocrinology, 6(2), 130-142. https://doi.org/10.1016/S2213-8587(17)30239-5Article Title and Year Published
Effects of an outpatient diabetes self-management education on patients with type 2 diabetes in China, 2019Inpatient diabetes education in the real world: an overview of guidelines and delivery models, 2019Effect of diabetes education through pattern management on self-care and self-efficacy in patients with type 2 diabetes, 2019Diabetes structured self-management education programs, 2018Research Questions (Qualitative)/Hypothesis (Quantitative)
Is a simple outpatient diabetes self-management education program effective?Do hospitals face challenges in delivering inpatient diabetes education with the increase in readmission and hospitalizations?How does applying customized diabetes management programs through pattern management affect individual self-care behaviors and self-efficacy in patients with type two diabetes mellitus?What improvements have been seen in self-management diabetes education programs during the last two decades?Purposes/Aim of StudyAssessing the effectiveness of a simple outpatient diabetes self-management education program
Providing an overview of the current state of inpatient diabetes education using the existing guidelines and education models.
Investigating the effect of applying customized diabetes education programs on patients’ self-care behaviors and self-efficacy.Assessing the improvement in self-management diabetes education programs.Design (Type of Quantitative, or Type of Qualitative)Single-blinded randomized control studySummary overview of the existing diabetes education models.Nonequivalent control group pretest-protest designNarrative review.Setting/Sample
60 patients in an outpatients department Xiangya Hospital, Central South UniversityDiabetes-Specialty care models and diabetes-non-specialty care models were reviewedType 2 diabetes patients of age 18-70 who visited the hospital between March 2017 and September 2017Existing self-management diabetes education programsMethods: Intervention/Instruments
Two-group experimental design was used. Diabetes Education models Summary reviewpretest-posttest design to test the effects of PM-based diabetes education utilizing CGMS results of patients with diabetesSystematic reviews of diabetes self-management education programs done between 2012 and 2017Analysis
SDSDA, PAID, FBG, postprandrial2 h
blood glucose, and HbA1c tests were all performed to evaluate
the effects of interventions for both groups before and
After three months.
The existing inpatient diabetes education models were discussed in line with their reported outcomesThe effects on self-efficacy and self-care behavior were analyzed using ANOVA. Collected data was analyzed using SPSS version 22Analysis of the evidence-based reports of the articles reviewed.Key FindingsFor the control group, Scores of the diabetes self-care activities significantly improved in the intervention group after the interventionInpatient diabetes education should provide survival skills for self-management upon discharge until more outpatient education is provided.Positive changes in self-care behavior were observed. Self-care behaviors improved after diabetes education programsThere is an increase in self-empowerment in self–management diabetes education models. There is an integration of psychosocial models in diabetes education.Recommendations
Diabetes self-management education can improve psychological conditions and glycemic control in T2DM.Both diabetes specialty care models and diabetes non-specialty care models can be used successfully for inpatient diabetes education.Customized diabetes education programs specific to each patient’s characteristics should be developed.Psychosocial issues and communication should be considered in self-management education.Explanation of How the Article Supports EBP/Capstone Project
The article provides evidence of the impact of education on patients with type 2 diabetes. The article shows that well-structured education is the basis of patient responsibility and increases patient self-management.The article provides an overview of inpatient patient education. It shows the superiority of structured education to other forms of patient education. It also alternatives for patient education.The article introduces the importance of education in increasing self-efficacy and self-management. It supports that patient education is the best intervention to improve self-efficacy and self-management because diabetes care is highly dependent on patients’ interventions.The study shows that structured education programs utilizing nursing terminologies are the best interventions to deliver quality education. The standardized terminologies are vital in covering patients’ differences
CriteriaArticle 5Article 6Article 7Article 8Author, Journal (Peer-Reviewed), and
Permalink or Working Link to Access Article
Ghisi, G. L. D. M., Seixas, M. B., Pereira, D. S., Cisneros, L. L., Ezequiel, D. G. A., Aultman, C., Sandison, N., Oh, P., & da Silva, L. P. (2021). Patient education program for Brazilians living with diabetes and prediabetes: findings from a development study. BMC public health, 21(1), 1-16. https://doi.org/10.1186/s12889-021-11300-y
Xu, G., Liu, B., Sun, Y., Du, Y., Snetselaar, L. G., Hu, F. B., & Bao, W. (2018). Prevalence of diagnosed type 1 and type 2 diabetes among U.S. adults in 2016 and 2017: a population-based study. Bmj, 362. https://doi.org/10.1136/bmj.k1497
Rahaman, H. S., Jyotsna, V. P., Sreenivas, V., Krishnan, A., & Tandon, N. (2018). Effectiveness of a patient education module on diabetic foot care in outpatient setting: An open-label randomized controlled study. Indian Journal of Endocrinology and Metabolism, 22(1), 74. https://dx.doi.org/10.4103/ijem.IJEM_148_17Galaviz, K. I., Weber, M. B., Straus, A., Haw, J. S., Narayan, K. V., & Ali, M. K. (2018). Global diabetes prevention interventions: a systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose. Diabetes Care, 41(7), 1526-1534. https://doi.org/10.2337/dc17-2222
Article Title and Year Published
Patient education program for Brazilians living with diabetes and prediabetes: findings from a development study, 2021Prevalence of diagnosed type 1 and type 2 diabetes among U.S. adults in 2016 and 2017: a population-based study, 2018Effectiveness of a patient education module on diabetic foot care in outpatient setting: An open-label randomized controlled study.Global diabetes prevention interventions: a systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose, 2018Research Questions (Qualitative)/Hypothesis (Quantitative)
Can there be a diabetes education program that is specifically applicable to Brazilians living with diabetes?How prevalent is diabetes type 1 and 2 among us adults?How effective is the foot care education module that the team had developed?Can LSM strategies implemented under real-world conditions lower diabetes risk and promote weight loss?Purposes/Aim of StudyDevelop a diabetes patient education program applicable to the Brazilian population living with diabetes.Estimating the prevalence of diagnosed total diabetes type 1 and 2 in the U.S. general population and the proportion among U.S. adults.Assessing the effectiveness of a foot care education module the authors had developed.The purpose of this study was to synthesize global evidence on the impact of LSM strategies on diabetes incidence and risk factors in one parsimonious model.Design (Type of Quantitative, or Type of Qualitative)
Narrative of existing diabetes education programsNationwide, population-based, cross-sectional surveyRandomized controlled studyEpidemiological study designSetting/Sample
Both inpatient and outpatient Brazilians living with diabetes. Diabetes patient educatorsNational health interview survey 2016 and 2017. U.S. adults aged 20 and above165 Adult patients diagnosed with Diabetes type 1 or 2 attending endocrinology from July 2015 to December 2016PubMed, Embase, Cochrane Library, and ClinicalTrials.gov were searched for studies published between January 1990 and April 2015.Methods: Intervention/Instruments
Review of the development process of diabetes patient education programs.Data was collected through NHIS and standardized questionnaires.Block randomization was used to divide the patients into a control group and an intervention groupMeta-analysis was used to obtain evidence of the effectsAnalysis
Best practices in diabetes education programs in Brazil and South America were analyzed using systematic reviews.Data was statistically analyzed using survey weights.Randomized control trials were used to analyze the effect of healthcare education on foot care knowledge and behavior in diabetes patients.random-effects meta-analysis techniques were applied to obtain a pooled pre/post mean difference for weight and glucose outcomes among intervention participantsKey Findings
Development phases of a diabetes education program were explained. A program applicable to Brazilian patients was developed.The study provided benchmark estimates on the national prevalence of diagnosed type 1 diabetes (0.5%) and type 2 diabetes (8.5%) among U.S. adults. Among U.S. adults with diagnosed diabetes, type 1 and type 2 diabetes accounted for 5.6% and 91.2%, respectively.The module was effective. Persistent change in foot care behavior requires the patient to have reinforcement regularly.The study found that participants receiving an intervention had a 29% lower risk of developing diabetes, lost 1.5 kg more body weight, and reduced FBG by 0.09 mmol/L more than participants not receiving one.Recommendations
The program’s effectiveness must be tested in the future as meeting individual needs requires sustained efforts.
The study recommends further investigations into the disparities in the prevalenceThe study recommends further improvement on the diabetes patient education moduleEven though LSM strategies can succeed in diabetes prevention, the study recommends further studies in low-income countries.Explanation of How the Article Supports EBP/CapstoneThe article shows the applicability and importance of education in diabetes care. The article provides evidence of increased self-management and better patient education after diabetes education, hence proving the project’s viability.The article provides data on the real-world prevalence of diabetes. It portrays it as a priority clinical problem. In addition, it recommends specific interventions such as mass awareness and patient education to reduce the diabetes healthcare burden.The article reviews the costs of diabetes. It also reviews its interventions and preventability. The article recommends rigorous public sensitization and patient education to prevent diabetes and its complicationsThe article reviews the global diabetes prevention interventions. Diabetes education features as an essential intervention in the prevention and prognosis of diabetes.
READ MORE >>
NRS 493 Scholarly Virtual Tools Activities DiscussionScholarly activities for Ca ...
NRS 493 Scholarly Virtual Tools Activities Discussion
Scholarly activities for Capstone project, due to COVID all things are virtual so whatever you write keep that in mind that any meetings you may write about would of have to of been virtual. Just make up an activity that could of been done it would have to be something in Valley Hospital in Las Vegas NV since that is the location the capstone is based on and the activity has to be part of the capstone. On the questions about who just put the persons title and position but no names are needed. Thanks.
Scholarly Activities
This document describes the scholarly activity elements that should be included in a five paragraph summary. You may use this resource to help guide the preparation of the Scholarly Activities assignment, due in Topic 10.Overview
This section consists of a single paragraph that succinctly describes the scholarly activity that you attended/participated in, the target market for the activity, and the benefit of the activity to you.Problem
This section consists of either a short narrative or a list of bullet points that concisely identifies the problems the scholarly activity is designed to solve.Educate:- What is the current state of the activity topic? Explain why this is a problem, and for whom is it a problem?
Inspire:
- What could a nurse achieve by participating in the scholarly activity? Use declarative sentences with simple words to communicate each point. Less is more.
Solution
This section consists of either a short paragraph or a list of bullet points that concisely describes the solution to a proposed practice problem that the scholarly activity addressed and how it addresses the problem outlined in the previous section.
Opportunity
This section consists of short paragraphs that define the opportunity that the scholarly activity is designed to capture. It is important to cover the objectives and goals that were met. How will attending/participating in this scholarly activity help you grow as a nurse?
Program Competencies Addressed
This section consists of a list of program competencies that were addressed in this scholarly activity. Please use the list from the ISP.
NRS 493 Grand Canyon University Scholarly Virtual Tools Activities Discussion
Scholarly Activities
Throughout the RN-to-BSN program, students are required to participate in scholarly activities outside of clinical practice or professional practice. Examples of scholarly activities include attending conferences, seminars, journal club, grand rounds, morbidity and mortality meetings, interdisciplinary committees, quality improvement committees, and any other opportunities available at your site, within your community, or nationally.You are required to post at least one documented scholarly activity by the end of this course. In addition to this submission, you are required to be involved and contribute to interdisciplinary initiatives on a regular basis. Submit, by way of this assignment, a summary report of the scholarly activity, including who, what, where, when, and any relevant take-home points.Include the appropriate program competencies associated with the scholarly activity as well as future professional goals related to this activity. You may use the “Scholarly Activity Summary” resource to help guide this assignment.While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center. APA style is not required, but solid academic writing is expected.You are not required to submit this assignment to LopesWrite. Topics The capstone project change proposal will be presented to an interprofessional group of leaders. A final summary of the reflective journal entries will allow students to self-reflect on the process of developing an evidence-based change proposal. Students will apply concepts related to self-awareness, synthesis, and integration of new knowledge and skills in their nursing practice.NRS 493 Grand Canyon University Scholarly Virtual Tools Activities Discussion Objectives:
- Present the capstone project change proposal to an interprofessional group of leaders.
- Demonstrate interprofessional collaboration in the dissemination of the capstone project change proposal.
- Demonstrate achievement of the course objectives in the written completion of the Individual Success Plan (ISP).
- Integrate self-reflective practice in summarizing the practicum reflective journal entries.
NRS 493 Grand Canyon University Scholarly Virtual Tools Activities Discussion Sources
The resources provided on the Presenter’s Corner page of the Western Institute of Nursing website. URL: https://www.winursing.org/ Explore the Cochrane Collaboration website. URL: http://www.cochrane.org/ .Also Read:NRS 493 Topic 1 Individual Success Plan Essay Paper
READ MORE >>
it is possible to experience improved diagnosis ...
READ MORE >>
NRS 493 Topic 1 Capstone Change Project PaperWork with your preceptor to perform ...
NRS 493 Topic 1 Capstone Change Project Paper
Work with your preceptor to perform a needs assessment of the organization and community for your practicum. Review the needs assessment to identify possible project topics. In preparation for the capstone change project proposal, compile a list of three to five possible topics for your project and submit to the assignment instructor in LoudCloud.
You are not required to submit this NRS 493 Topic 1 Capstone Change Project Paper assignment to LopesWrite.
NRS 493 Topic 1 Professional Capstone and Practicum Reflective Journal
Students are required to submit weekly reflective narratives throughout the course that will culminate in a final, course-long reflective journal due in Topic 10. The narratives help students integrate leadership and inquiry into current practice.
This reflection journal also allows students to outline what they have discovered about their professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week students should also explain how they met a course competency or course objective(s).
In each week’s entry, students should reflect on the personal knowledge and skills gained throughout the course. Journal entries should address one or more of the areas stated below. In the Topic 10 graded submission, each of the areas below should be addressed as part of the summary submission.

- New practice approaches
- Interprofessional collaboration
- Health care delivery and clinical systems
- Ethical considerations in health care
- Practices of culturally sensitive care
- Ensuring the integrity of human dignity in the care of all patients
- Population health concerns
- The role of technology in improving health care outcomes
- Health policy
- Leadership and economic models
- Health disparities
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This NRS 493 Topic 1 Capstone Change Project Paper assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this NRS 493 Topic 1 Capstone Change Project Paper assignment to LopesWrite.
NRS 493 Topic 2 Capstone Topic Summary
In collaboration with the approved course preceptor, students will identify a specific evidence-based topic for the capstone project change proposal. Write a 150-250 word summary explaining which category your topic and intervention are under (community or leadership).
You are not required to submit this assignment to LopesWrite.
NRS 493 Topic 2 Capstone Project Topic Selection and Approval
In collaboration with the approved course preceptor, students will identify a specific evidence-based topic for the capstone project change proposal. Students should consider the clinical environment in which they are currently employed or have recently worked. The capstone project topic can be a clinical practice problem, an organizational issue, a leadership or quality improvement initiative, or an unmet educational need specific to a patient population or community. The student may also choose to work with an interprofessional collaborative team.
Students should select a topic that aligns to their area of interest as well as the clinical practice setting in which practice hours are completed.
Write a 500-750 word description of your proposed capstone project topic. Include the following:
- The problem or issue, intervention, quality initiative, educational need, or collaborative interprofessional team project that will be the focus of the change proposal.
- The setting or context in which the problem or issue, intervention, quality initiative, educational need, or collaborative interprofessional team project can be observed.
- A description (providing a high level of detail) regarding the problem or issue, intervention, quality initiative, educational need, or collaborative interprofessional team project.
- Effect of the problem or issue, intervention, quality initiative, educational need, or collaborative interprofessional team project.
- Significance of the topic and its implications for nursing practice.
- A proposed solution to the identified project topic with an explanation of how it will affect nursing practice.
You are required to cite to a minimum of eight peer-reviewed sources to complete this assignment. Sources must be published within the last 5 years, appropriate for the assignment criteria, and relevant to nursing practice. Plan your time accordingly to complete this assignment.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center. An abstract is not required.
You are required to submit this assignment to LopesWrite. Refer to the LopesWrite Technical Support articles for assistance.
Capstone Project Topic Selection and Approval Example Solution
Workplace Incivility in Nursing
Advancing a civil workplace culture has been a topic of interest in the current healthcare practice. Daily in nursing practice and training, nurses have to deal with some level of workplace incivility in many settings (Crawford et al., 2019). The impact of workplace incivility in nursing has been felt in more stressful environments such as emergency care units and operation units. This paper aims to describe this health issue, its impact on collaboration in nursing, its significance in nursing practice, and propose a solution to this issue.
Description of the Issue
Workplace incivility in nursing encompasses activities and behaviors that include but are not limited to bullying, eye-rolling, silent treatment, horizontal violence, and bullying, among other behaviors in the nursing workplace. In nursing education, incivility manifests as a lack of professionalism, disrespect to learners, and making these learners feel unwanted or ignored (Zhu et al., 2019). In worst-case scenarios, incivility in nursing education can present as illegal activities such as abuse, either sexual or physical, according to Zhu et al. (2019). Nursing incivility behaviors can be overt or covert. These behaviors can be perpetrated verbally or nonverbally. Disrespectful behaviors from staff toward learners can have consequences on civility in the long term because future nurses who will try to emulate these behaviors they learn from seniors.
Perpetrators of nursing incivility can be multiple in a single workplace. In most cases, the senior nurse practitioners or students are the key perpetrators of incivility (Stalter et al., 2020). Junior nurses experience uncivil nursing behaviors from instructors, healthcare assistants, subordinate workers, and sometimes physicians (Green, 2019). In other cases, these activities are horizontal. Behaviors are directed from fellow nurses and perpetrators are nurses of the same cadre in practice. Nursing incivility, especially bullying, aims at removing the victim’s power through aggression (Howard, 2019). Some cases of incivility can be deemed trivial in practice, but their impacts go beyond aggression and ego and power struggles.
Impacts of Nursing Incivility
Nursing workplace incivility impacts not only the individual victims but also the healthcare organization, the healthcare system, and the nursing profession. These impacts are organizational, academic, work unit-related, or personal (Crawford et al., 2019). Nursing, as a profession, is a system that relies on collaboration internally and with other professions to promote their interventions and achieve goals in care. These behaviors can seem insignificant but may have far-reaching negative consequences on nursing practice. The victims of nursing incivility can intentionally quit the profession or intentionally reduce their work effort.
The prevailing workforce shortage and availability or demand of nurses in the market are used to mask the impacts of incivility (Green, 2019). When these victims decide to stay in the profession, their intentions to leave the work or profession are always higher due to incivility. They spend a substantial amount of time worrying about their work and practice (Bar-David, 2018). In worse cases, the victims may take their frustrations on the clients.
Therefore, patient safety is jeopardized just because of workplace incivility. The risk of medication and medical errors rises due to frustration. Viciously, this culture can be passed down to learners who later practice uncivil behaviors in the workplace (Andersen et al., 2019). Poor mental health has been reported among nurses who experience workplace incivility (Howard, 2019). This impacts their productivity and the quality of the care they offer.
Significance of the Issue
Nursing workplace incivility is a universal issue that silently undermines the quality of care. By jeopardizing patient safety, patient satisfaction reduces. Work efficiency and effectiveness are also likely to reduce due to a lack of motivation and high intention to quit work or profession. This issue thus can be addressed in the early steps, that is, nursing education and the workplace, to mitigate its negative impact on the healthcare system and profession. The nursing profession was built on Caritas and tenderness and upholding these virtues to our clients, it is only logical that the nurses show them to their colleagues first. Addressing civility in the workplace improves nurses’ and nurse administrators’ leadership and administrative skills.
Proposed Solution
Addressing nursing workplace incivility can be achieved by evidence-based practice (EBP). Evidence-based teaching strategies promote systems thinking that would prevent patient harm by improving patient outcomes (Stalter et al., 2020). Evidence-based nursing education and teaching that encourages nurses and empowers them to create a civil environment for learning and working have improved nursing civility by addressing behavior change (Crawford et al., 2019). The American Nurses Association stands for zero tolerance against workplace incivility and to abide by their professional conduct codes, nurses must begin change at the personal levels. However, nursing incivility is multifactorial, and addressing the behavioral aspects only would not solve the issue completely.
Conclusion
The nursing profession has turned into a profession that ‘eats its own’ through workplace incivility. This has been seen in nursing education and practice. Some senior nurses and fellow nurses have practiced varying degrees of incivility that have consequences on the personal, academic, professional, system, and organizational outcomes. Evidence-based nursing teaching and education have been documented in literature evidence to help mitigate nursing workplace incivility
NRS 493 Topic 1 Capstone Change Project Paper References
Andersen, P., McAllister, M., Kardong-Edgren, S., Miller, C. W., & Churchouse, C. (2019). Incivility behaviors exhibited by nursing students: clinical educators’ perspectives of challenging teaching and assessment events in clinical practice. Contemporary Nurse, 55(4–5), 303–316. https://doi.org/10.1080/10376178.2019.1634480
Bar-David, S. (2018). What’s in an eye roll? It is time we explore the role of workplace incivility in healthcare. Israel Journal of Health Policy Research, 7(1), 15. https://doi.org/10.1186/s13584-018-0209-0
Crawford, C. L., Chu, F., Judson, L. H., Cuenca, E., Jadalla, A. A., Tze-Polo, L., Kawar, L. N., Runnels, C., & Garvida, R., Jr. (2019). An integrative review of nurse-to-nurse incivility, hostility, and workplace violence: A GPS for nurse leaders: A GPS for nurse leaders. Nursing Administration Quarterly, 43(2), 138–156. https://doi.org/10.1097/NAQ.0000000000000338
Green, C. (2019). Incivility among nursing professionals in clinical and academic environments: Emerging research and opportunities: Emerging research and opportunities (Vol. 181). Medical Information Science Reference. https://doi.org/10.4018/978-1-5225-7341-8
Handzel, S., BSN, & RN. (2020, October 19). Incivility in nursing: An approach for change. Wolterskluwer.com. https://www.wolterskluwer.com/en/expert-insights/incivility-in-nursing
Howard, M. S. (2019). Bullying in nursing: Implementing solutions for practice. Creating Healthy Work Environments 2019. https://stti.confex.com/stti/chwe19/webprogram/Paper94227.html
Stalter, A. M., Phillips, J. M., Goldschmidt, K. A., Brodhead, J., Ruggiero, J. S., Scardaville, D. L., McKay, M., Bonnett, P. L., & Merriam, D. (2020). Promoting civility in nursing practice using systems thinking: Evidence-based teaching strategies for nurse educators. Nursing Forum, 55(4), 754–762. https://doi.org/10.1111/nuf.12493
Zhu, Z., Xing, W., Lizarondo, L., Guo, M., & Hu, Y. (2019). Nursing students’ experiences with faculty incivility in the clinical education context: a qualitative systematic review and meta-synthesis. BMJ Open, 9(2), e024383. https://doi.org/10.1136/bmjopen-2018-024383
NRS 493 Topic 2 Professional Capstone and Practicum Reflective Journal
Students are required to submit weekly reflective narratives throughout the course that will culminate in a final, course-long reflective journal due in Topic 10. The narratives help students integrate leadership and inquiry into current practice.
This reflection journal also allows students to outline what they have discovered about their professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week students should also explain how they met a course competency or course objective(s).
In each week’s entry, students should reflect on the personal knowledge and skills gained throughout the course. Journal entries should address one or more of the areas stated below. In the Topic 10 graded submission, each of the areas below should be addressed as part of the summary submission.
- New practice approaches
- Interprofessional collaboration
- Health care delivery and clinical systems
- Ethical considerations in health care
- Practices of culturally sensitive care
- Ensuring the integrity of human dignity in the care of all patients
- Population health concerns
- The role of technology in improving health care outcomes
- Health policy
- Leadership and economic models
- Health disparities
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
Professional Capstone and Practicum Reflective Journal- Topic 2 Example Solution
Topic Focus: Interprofessional Collaboration
Interprofessional collaboration involves interaction between two or more professionals with common goals and problem-solving needs. This topic has introduced me to various aspects of problem-solving and made me realize some strengths and weaknesses in my training so far. At the end of the course and training, I aim at acquiring the best quality and safety education in nursing (QSEN) competencies to offer the best care to my patients in the future.
In this topic, I aimed at dealing with teamwork and collaboration as a part of the progress to achieve the best competencies. My evaluation of problems and issues relevant to my practice and this competency element was civility in the workplace. I believe that a civil working and learning environment encourages reciprocal interaction that will enhance academic and professional growth. Therefore, based on my experience worth the topic I dug deep into the issue and presented my issue using evidence-based practice.
One of the strengths that I realized from this topic is evidence-based practice and interprofessional collaboration. The knowledge behind these strengths was enhanced by the passion to look up and interpret relevant literature evidence. In the future, I intend to work in an environment will many professionals thus the need to sharpen further my interprofessional skills. Hopefully, the skills that I will gain throughout the course will develop this strength and make me a competent nurse. Additional resources such as interactive multimedia learning and simulated scenarios will impact greatly my leadership and collaboration skills. This will expose my learning to various real-life scenarios and ensure stimulative learning. It is my wish that my individual commitment to work with my fellows will ensure future success.
NRS 493 Topic 3 PICOT Question Paper
Review your problem or issue and the study materials to formulate a PICOT question for your capstone project change proposal. A PICOT question starts with a designated patient population in a particular clinical area and identifies clinical problems or issues that arise from clinical care.
The intervention used to address the problem must be a nursing practice intervention. Include a comparison of the nursing intervention to a patient population not currently receiving the nursing intervention, and specify the timeframe needed to implement the change process. Formulate a PICOT question using the PICOT format (provided in the assigned readings) that addresses the clinical nursing problem.
The PICOT question will provide a framework for your capstone project change proposal.
In a paper of 500-750 words, clearly identify the clinical problem and how it can result in a positive patient outcome.
Describe the problem in the PICOT question as it relates to the following:
- Evidence-based solution
- Nursing intervention
- Patient care
- Health care agency
- Nursing practice
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center. An abstract is not required.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. Refer to the LopesWrite Technical Support articles for assistance.
PICOT Question Example
The human body comprises complex systems that perform various functions that promote life. The immune system is among the essential systems that prevent the body from infections. Immunity is not limited to the lymphoid system, intact skin, initial inflammatory response, and oral mucosa (Bankanie et al., 2021). Unlike healthy individuals who have improved immunity, patients in the intensive unit (ICU) are at increased risk of several infections due to reduced immunity and invasive life-saving procedures such as endotracheal intubation, central lines, and mechanical ventilation (Chen et al., 2022).
As a result, they are susceptible to most infections, including bacteremia, periodontal disease, central line infections, infective endocarditis, and ventilator-acquired pneumonia (VAP). Reducing such infections requires nurse-led interventions to reduce incidences while improving patient outcomes. Among the common interventions aimed at improving oral hygiene, preventing aspiration of micro-biota, and reducing colonization by micro-organisms. To get more insight, I came up with a PICOT question that will aid in improving my knowledge of this subject.
PICOT: In adult patients intubated in ICU (P), how does daily use of Chlorohexidine (I) compared to not using (C) reduce the risk of ventilator-acquired pneumonia (VAP) (O) over three months? (T)
Clinical Problem
VAP is a lung infection that develops more than 48 hours after intubation for mechanical ventilation. It is the most common nosocomial infection among intubated ICU patients, accounting for 9-27% of infections in the ICU (Bankanie et al., 2021). Endotracheal intubation is performed to save the lives of critically ill patients who are unable to breathe, unconscious, or sedated by medications. It helps by maintaining the patency of the airway and supplying oxygen for metabolic demands. Despite being useful, they act as a breach through which microorganisms access the respiratory tract, causing VAP.
VAP is caused by various micro-organisms that invade the respiratory tract. Among the most common isolated bacteria include Staphylococcus aureus, Pseudomonas aeruginosa, and Enterobacteriaceae (Chen et al., 2022). These pathogens inoculate either in the oropharynx, gastrointestinal, subglottic, or oral mucosa, where they spread to the lower respiratory system, causing the infection.
In addition to endotracheal intubation, other risk factors increase the risk of VAP, including advanced age, immobilization, supine body positioning, certain medications, and ventilatory support (Dale et al., 2019). The development of VAP negatively impairs patient outcomes. It increases the risk of mortality, hospital stay, and morbidity, consequently increasing the cost of care. Reducing the negative outcomes requires the installation of preventive methods that improve outcomes.
Nursing Intervention
Despite the adverse effects caused by VAP, nurses have a vital role in devising preventive measures to reduce incidences. Among the various preventive measures, the use of chlorhexidine gluconate (CHG) is an evidence-based practice that has been used in various settings (Kocaçal et al., 2019). CHG is an antiseptic agent that has a bactericidal effect against harmful bacteria. It is effective against both gram-positive and gram-negative bacteria. It acts by binding to the cell wall of bacteria, thus inhibiting cell wall integrity and causing bacterial death (Niedzwiecka et al., 2019). Therefore, it leads to a reduction in microbial load while reducing incidences of nosocomial infections, including VAP. This leads to improved patient outcomes while reducing morbidity and mortality.
Summary
VAP is a common clinical problem yet preventable. Integration of using CHG in clinical practice has proved to be effective in reducing the incidences. Therefore, it is paramount that all nurses adhere to preventive methods while managing patients. This will help in reducing the cost of care, reduce hospital stays, improve patient satisfaction, reduce mortality and morbidity, and improve patient outcomes. Finally, prevention of VAP will reduce the rate of drug-resistant organisms that are difficult to treat.
References
Bankanie, V., Outwater, A. H., Wan, L., & Yinglan, L. (2021). Assessment of knowledge and compliance to evidence-based guidelines for VAP prevention among ICU nurses in Tanzania. BMC Nursing, 20(1), 209. https://doi.org/10.1186/s12912-021-00735-8
Chen, S., Hua, L., Jin, Q., & Wang, H. (2022). Correlation of ICU nurses’ cognitive level with their attitude and behavior toward the prevention of ventilator-associated pneumonia. Journal of Healthcare Engineering, 2022, 8229812. https://doi.org/10.1155/2022/8229812
Dale, C. M., Rose, L., Carbone, S., Smith, O. M., Burry, L., Fan, E., Amaral, A. C. K.-B., McCredie, V. A., Pinto, R., Quiñonez, C. R., Sutherland, S., Scales, D. C., & Cuthbertson, B. H. (2019). Protocol for a multi-centered stepped wedge, cluster randomized controlled trial of the de-adoption of oral chlorhexidine prophylaxis and implementation of an oral care bundle for mechanically ventilated critically ill patients: the CHORAL study. Trials, 20(1), 603. https://doi.org/10.1186/s13063-019-3673-0
Kocaçal Güler, E., & Türk, G. (2019). Oral chlorhexidine against ventilator-associated pneumonia and microbial colonization in intensive care patients. Western Journal of Nursing Research, 41(6), 901–919. https://doi.org/10.1177/0193945918781531
Niedzwiecka, T., Patton, D., Walsh, S., Moore, Z., O’Connor, T., & Nugent, L. (2019). What are the effects of care bundles on the incidence of ventilator-associated pneumonia in paediatric and neonatal intensive care units? A systematic review. Journal for Specialists in Pediatric Nursing: JSPN, 24(4), e12264. https://doi.org/10.1111/jspn.12264
NRS 493 Topic 3 Benchmark Capstone Change Project Objectives
Review your problem or issue and the cultural assessment. Consider how the findings connect to your topic and intervention for your capstone change project. Write a list of three to five objectives for your proposed intervention. Below each objective, provide a one or two sentence rationale.
After writing your objectives, provide a rationale for how your proposed project and objectives advocate for autonomy and social justice for individuals and diverse populations.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
Benchmark Information
This benchmark assignment assesses the following programmatic competencies:
RN to BSN
1.5: Advocate for autonomy and social justice for individuals and diverse populations.
NRS 493 Topic 3 Professional Capstone and Practicum Reflective Journal
Students are required to submit weekly reflective narratives throughout the course that will culminate in a final, course-long reflective journal due in Topic 10. The narratives help students integrate leadership and inquiry into current practice.
This reflection journal also allows students to outline what they have discovered about their professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week students should also explain how they met a course competency or course objective(s).
In each week’s entry, students should reflect on the personal knowledge and skills gained throughout the course. Journal entries should address one or more of the areas stated below. In the Topic 10 graded submission, each of the areas below should be addressed as part of the summary submission.
- New practice approaches
- Interprofessional collaboration
- Health care delivery and clinical systems
- Ethical considerations in health care
- Practices of culturally sensitive care
- Ensuring the integrity of human dignity in the care of all patients
- Population health concerns
- The role of technology in improving health care outcomes
- Health policy
- Leadership and economic models
- Health disparities
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
Professional Capstone and Practicum Reflective Journal Topic 3 Example
Health Care Delivery and Clinical Systems
As a nursing student, I have realized that clinical systems and healthcare delivery are crucial components in a work environment. A good collaboration between the two guarantees that the organization and patient interests are observed efficiently. I have also learned the importance of teamwork. I am confident that working together with other players in the healthcare industry can ensure success for both the institution, patients, and care providers. This paper will reflect on the critical aspects that make healthcare delivery and clinical systems crucial and their significance in the institution.
In the healthcare system, healthcare delivery is a critical segment, and it determines the perception of the system to the outside world. That is all the patients and the public see when they look at healthcare institutions. Reg
READ MORE >>
and in-text citations and references should be presented using APA documentatio ...
READ MORE >>
course-long reflective journal due in Topic 10. The narratives help students in ...
This reflection journal also allows students to outline what they have discovered about their professional practice
READ MORE >>
NRS 493 Topic 1 Professional Capstone and Practicum Reflective Journal Assignmen ...
NRS 493 Topic 1 Professional Capstone and Practicum Reflective Journal Assignment
NRS 493 Topic 1 Professional Capstone and Practicum Reflective Journal Assignment
Students are required to submit weekly reflective narratives throughout the course that will culminate in a final, course-long reflective journal due in Topic 10. The narratives help students integrate leadership and inquiry into current practice.
This reflection journal also allows students to outline what they have discovered about their professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week students should also explain how they met a course competency or course objective(s).
In each week’s entry, students should reflect on the personal knowledge and skills gained throughout the course. Journal entries should address one or more of the areas stated below. In the Topic 10 graded submission, each of the areas below should be addressed as part of the summary submission.

- New practice approaches
- Interprofessional collaboration
- Health care delivery and clinical systems
- Ethical considerations in health care
- Practices of culturally sensitive care
- Ensuring the integrity of human dignity in the care of all patients
- Population health concerns
- The role of technology in improving health care outcomes
- Health policy
- Leadership and economic models
- Health disparities
While APA style is not required for the body of this Assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This Assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this Assignment to LopesWrite.
NRS 493 Topic 2 Capstone Topic Summary
In collaboration with the approved course preceptor, students will identify a specific evidence-based topic for the capstone project change proposal. Write a 150-250 word summary explaining which category your topic and intervention are under (community or leadership).
You are not required to submit this assignment to LopesWrite.
Professional Capstone and Practicum Reflective Journal- Topic 2 Example
Topic Focus: Interprofessional Collaboration
Interprofessional collaboration involves interaction between two or more professionals with common goals and problem-solving needs. This topic has introduced me to various aspects of problem-solving and made me realize some strengths and weaknesses in my training so far. At the end of the course and training, I aim at acquiring the best quality and safety education in nursing (QSEN) competencies to offer the best care to my patients in the future.
In this topic, I aimed at dealing with teamwork and collaboration as a part of the progress to achieve the best competencies. My evaluation of problems and issues relevant to my practice and this competency element was civility in the workplace. I believe that a civil working and learning environment encourages reciprocal interaction that will enhance academic and professional growth. Therefore, based on my experience worth the topic I dug deep into the issue and presented my issue using evidence-based practice.
One of the strengths that I realized from this topic is evidence-based practice and interprofessional collaboration. The knowledge behind these strengths was enhanced by the passion to look up and interpret relevant literature evidence. In the future, I intend to work in an environment will many professionals thus the need to sharpen further my interprofessional skills. Hopefully, the skills that I will gain throughout the course will develop this strength and make me a competent nurse.
Additional resources such as interactive multimedia learning and simulated scenarios will impact greatly my leadership and collaboration skills. This will expose my learning to various real-life scenarios and ensure stimulative learning. It is my wish that my individual commitment to work with my fellows will ensure future success.
NRS 493 Topic 2 Capstone Project Topic Selection and Approval
In collaboration with the approved course preceptor, students will identify a specific evidence-based topic for the capstone project change proposal. Students should consider the clinical environment in which they are currently employed or have recently worked. The capstone project topic can be a clinical practice problem, an organizational issue, a leadership or quality improvement initiative, or an unmet educational need specific to a patient population or community. The student may also choose to work with an interprofessional collaborative team.
Students should select a topic that aligns to their area of interest as well as the clinical practice setting in which practice hours are completed.
Write a 500-750 word description of your proposed capstone project topic. Include the following:
- The problem or issue, intervention, quality initiative, educational need, or collaborative interprofessional team project that will be the focus of the change proposal.
- The setting or context in which the problem or issue, intervention, quality initiative, educational need, or collaborative interprofessional team project can be observed.
- A description (providing a high level of detail) regarding the problem or issue, intervention, quality initiative, educational need, or collaborative interprofessional team project.
- Effect of the problem or issue, intervention, quality initiative, educational need, or collaborative interprofessional team project.
- Significance of the topic and its implications for nursing practice.
- A proposed solution to the identified project topic with an explanation of how it will affect nursing practice.
You are required to cite to a minimum of eight peer-reviewed sources to complete this assignment. Sources must be published within the last 5 years, appropriate for the assignment criteria, and relevant to nursing practice. Plan your time accordingly to complete this assignment.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center. An abstract is not required.
You are required to submit this assignment to LopesWrite. Refer to the LopesWrite Technical Support articles for assistance.
NRS 493 Topic 2 Professional Capstone and Practicum Reflective Journal
Students are required to submit weekly reflective narratives throughout the course that will culminate in a final, course-long reflective journal due in Topic 10. The narratives help students integrate leadership and inquiry into current practice.
This reflection journal also allows students to outline what they have discovered about their professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week students should also explain how they met a course competency or course objective(s).
In each week’s entry, students should reflect on the personal knowledge and skills gained throughout the course. Journal entries should address one or more of the areas stated below. In the Topic 10 graded submission, each of the areas below should be addressed as part of the summary submission.
- New practice approaches
- Interprofessional collaboration
- Health care delivery and clinical systems
- Ethical considerations in health care
- Practices of culturally sensitive care
- Ensuring the integrity of human dignity in the care of all patients
- Population health concerns
- The role of technology in improving health care outcomes
- Health policy
- Leadership and economic models
- Health disparities
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
NRS 493 Topic 3 PICOT Question Paper
Review your problem or issue and the study materials to formulate a PICOT question for your capstone project change proposal. A PICOT question starts with a designated patient population in a particular clinical area and identifies clinical problems or issues that arise from clinical care.
The intervention used to address the problem must be a nursing practice intervention. Include a comparison of the nursing intervention to a patient population not currently receiving the nursing intervention, and specify the timeframe needed to implement the change process. Formulate a PICOT question using the PICOT format (provided in the assigned readings) that addresses the clinical nursing problem.
The PICOT question will provide a framework for your capstone project change proposal.
In a paper of 500-750 words, clearly identify the clinical problem and how it can result in a positive patient outcome.
Describe the problem in the PICOT question as it relates to the following:
- Evidence-based solution
- Nursing intervention
- Patient care
- Health care agency
- Nursing practice
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center. An abstract is not required.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. Refer to the LopesWrite Technical Support articles for assistance.
NRS 493 Topic 3 Benchmark Capstone Change Project Objectives
Review your problem or issue and the cultural assessment. Consider how the findings connect to your topic and intervention for your capstone change project. Write a list of three to five objectives for your proposed intervention. Below each objective, provide a one or two sentence rationale.
After writing your objectives, provide a rationale for how your proposed project and objectives advocate for autonomy and social justice for individuals and diverse populations.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
Benchmark Information
This benchmark assignment assesses the following programmatic competencies:
RN to BSN
1.5: Advocate for autonomy and social justice for individuals and diverse populations.
NRS 493 Topic 3 Professional Capstone and Practicum Reflective Journal
Students are required to submit weekly reflective narratives throughout the course that will culminate in a final, course-long reflective journal due in Topic 10. The narratives help students integrate leadership and inquiry into current practice.
This reflection journal also allows students to outline what they have discovered about their professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week students should also explain how they met a course competency or course objective(s).
In each week’s entry, students should reflect on the personal knowledge and skills gained throughout the course. Journal entries should address one or more of the areas stated below. In the Topic 10 graded submission, each of the areas below should be addressed as part of the summary submission.
- New practice approaches
- Interprofessional collaboration
- Health care delivery and clinical systems
- Ethical considerations in health care
- Practices of culturally sensitive care
- Ensuring the integrity of human dignity in the care of all patients
- Population health concerns
- The role of technology in improving health care outcomes
- Health policy
- Leadership and economic models
- Health disparities
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
Professional Capstone and Practicum Reflective Journal Topic 3 Example
Health Care Delivery and Clinical Systems
As a nursing student, I have realized that clinical systems and healthcare delivery are crucial components in a work environment. A good collaboration between the two guarantees that the organization and patient interests are observed efficiently. I have also learned the importance of teamwork. I am confident that working together with other players in the healthcare industry can ensure success for both the institution, patients, and care providers. This paper will reflect on the critical aspects that make healthcare delivery and clinical systems crucial and their significance in the institution.
In the healthcare system, healthcare delivery is a critical segment, and it determines the perception of the system to the outside world. That is all the patients and the public see when they look at healthcare institutions. Regarding how a hospital is equipped or the type of services they provide, the most critical aspect is ensuring that the healthcare delivery is convenient for the people (Cerise et al., 2021). This topic further elaborated on the healthcare system and its diverse aspects. Therefore, it helps me understand the concept of the healthcare system in a greater way and provides me with different perceptions.
As a nursing student, I have realized that the most crucial point is that when there is good healthcare delivery, it is possible to experience improved diagnosis, treatment of ailments, and enhance health promotion. There is a guarantee of covering public health, primary and specialized care, pharmaceutical care, and mental healthcare with better healthcare delivery. Through my interactions in the healthcare industry, I have also learned some important healthcare aspects, such as the importance of patient-centeredness and integration in care delivery.
Through innovation and proactive practices, I feel these areas can help improve healthcare delivery and profit the patients and the public more. It also guarantees effective and smooth operations for the healthcare workers and enhances the organization’s satisfaction by meeting the expectations of their respective clients.
On the other hand, for healthcare delivery to be effective, it is essential to operate hand-to-hand with the clinical systems. In my capacity, I have come to realize that for healthcare delivery to be effective. The present clinical systems have to be efficient. According to Rhatigan (2020, the systems make it possible to provide patient-centered and evidence-based care under all care preferences. It ensures that the hospital experiences minimal medical errors, reduces unnecessary healthcare costs increase legibility, and boosts the quality of care.
With better clinical systems, it is easy for the hospital to capture, store, and process critical information and ensure timely transfer to relevant bodies to guarantee rapid and correct decision-making. Therefore, it ensures that the patients visiting the facility receive personalized care and build a network of trust with caregivers for future healthcare benefits. In my opinion, by enhancing the clinical systems, the deficit of trust between team players will be eliminated, allowing all institution organs to operate together for the interests of the patients.
Additionally, through mobilizing better clinical systems, the organization has better and increased opportunities to expand and improve critical hospital equipment (Rhatigan, 2020). Therefore, service delivery will be efficient and directly address the issues of concern to the specific clients that the hospital receives. Synchronizing clinical systems and healthcare delivery also enhances hospital decongestion by ensuring that the facility reduces the number of patient admissions. This way, the organization’s economic model will be functional, and patient’s satisfaction will increase.
References
Cerise, F. P., Moran, B., Huang, P. P., & Bhavan, K. P. (2021). The imperative for integrating public health and health care delivery systems. NEJM Catalyst Innovations in Care Delivery, 2(4). DOI:https://doi.org/10.1056/CAT.20.0580
Rhatigan Jr, J. J. (2020). Health systems and health care delivery. In Hunter’s Tropical Medicine and Emerging Infectious Diseases (pp. 214-218). Elsevier. https://doi.org/10.1016/B978-0-323-55512-8.00028-4
NRS 493 Professional Capstone Practicum Essays GCU – Topic 4 Literature Evaluation Table
In nursing practice, accurate identification and application of research is essential to achieving successful outcomes. The ability to articulate research data and summarize relevant content supports the student’s ability to further develop and synthesize the assignments that constitute the components of the capstone project.
The assignment will be used to develop a written implementation plan.
For this assignment, provide a synopsis of the review of the research literature. Using the “Literature Evaluation Table,” determine the level and strength of the evidence for each of the eight research articles you have selected. The articles should be current (within the last 5 years) and closely relate to the PICOT question developed earlier in this course.
The articles may include quantitative research, descriptive analyses, longitudinal studies, or meta-analysis articles. A systematic review may be used to provide background information for the purpose or problem identified in the proposed capstone project.
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
NRS 493 Topic 4 Capstone Change Project Outcomes
After working with your preceptor to assess organizational policies, create a list of measurable outcomes for your capstone project intervention. Write a list of three to five outcomes for your proposed intervention. Below each outcome, provide a one or two sentence rationale.
The assignment will be used to develop a written implementation plan.
APA style is not required, but solid academic writing is expected.
You are not required to submit this assignment to LopesWrite.
NRS 493 Topic 4 Professional Capstone and Practicum Reflective Journal
Students are required to submit weekly reflective narratives throughout the course that will culminate in a final, course-long reflective journal due in Topic 10. The narratives help students integrate leadership and inquiry into current practice.
This reflection journal also allows students to outline what they have discovered about their professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week students should also explain how they met a course competency or course objective(s).
In each week’s entry, students should reflect on the personal knowledge and skills gained throughout the course. Journal entries should address one or more of the areas stated below. In the Topic 10 graded submission, each of the areas below should be addressed as part of the summary submission.
- New practice approaches
- Interprofessional collaboration
- Health care delivery and clinical systems
- Ethical considerations in health care
- Practices of culturally sensitive care
- Ensuring the integrity of human dignity in the care of all patients
- Population health concerns
- The role of technology in improving health care outcomes
- Health policy
- Leadership and economic models
- Health disparities
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
NRS 493 Topic 5 Practice Experience Conference (Mid-Conference)
Students are required to initiate a mid-conference that will occur during Topic 5, using the “Practice Experience Conference Form (Mid-Conference)” resource. This conference is intended for the student, preceptor, and faculty to discuss progress toward meeting the learning goals and course objectives contained in the Individual Success Plan (ISP). Progress toward completing the written capstone project will also be discussed, including faculty recommendations for project development.
Student progress will be documented on the Clinical Evaluation Tool (CET), which is submitted in LoudCloud prior to the conference. The CET will be discussed during the mid-conference and graded in LoudCloud by the faculty after the mid-conference. If the student receives an “Unacceptable” or “Below Expectations” in any category, the student will remediate for that category of the CET.
NRS 493 Topic 5 Midterm Evaluation of Student
The preceptor will perform a midterm evaluation with the faculty. The faculty will input the evaluation content into the Lopes Activity Tracker. The student will upload the evaluation into LoudCloud after meeting with the preceptor to discuss the midterm evaluation.
Students must meet all clinical expectations of the course, earn a passing grade on all benchmark assignments, and successfully complete remediation (if necessary) in order to receive a passing grade in the NRS-493 course.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
NRS 493 Professional Capstone Practicum Essays GCU – Topic 5 Clinical Practice Experience Remediation
Students who are not making appropriate progress on their capstone project and receive an “Unacceptable” or “Below Expectations” on the CET will be required to complete remediation activities. Required remediation activities are listed on the “NRS-493: Clinical Experience Remediation” document. The required activities must be submitted in LoudCloud upon their completion by the end of Topic 7. All required remediation activities will be reviewed and approved by the faculty.
NRS 493 Topic 5 Professional Capstone and Practicum Reflective Journal
Students are required to submit weekly reflective narratives throughout the course that will culminate in a final, course-long reflective journal due in Topic 10. The narratives help students integrate leadership and inquiry into current practice.
This reflection journal also allows students to outline what they have discovered about their professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week students should also explain how they met a course competency or course objective(s).
In each week’s entry, students should reflect on the personal knowledge and skills gained throughout the course. Journal entries should address one or more of the areas stated below. In the Topic 10 graded submission, each of the areas below should be addressed as part of the summary submission.
- New practice approaches
- Interprofessional collaboration
- Health care delivery and clinical systems
- Ethical considerations in health care
- Practices of culturally sensitive care
- Ensuring the integrity of human dignity in the care of all patients
- Population health concerns
- The role of technology in improving health care outcomes
- Health policy
- Leadership and economic models
- Health disparities
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
NRS 493 Topic 5 Strategic Plan Summary
Assess the culture of the organization for potential challenges in incorporating the nursing practice intervention. Use this assessment when creating the strategic plan.
Write a 150-250 word strategic plan defining how the nursing practice intervention will be implemented in the capstone project change proposal.
APA style is not required, but solid academic writing is expected.
You are not required to submit this assignment to LopesWrite.
NRS 493 Topic 6 Literature Review
While the implementation plan prepares students to apply their research to the problem or issue they have identified for their capstone project change proposal, the literature review enables students to map out and move into the active planning and development stages of the project.
A literature review analyzes how current research supports the PICOT, as well as identifies what is known and what is not known in the evidence. Students will use the information from the earlier PICOT Question Paper and Literature Evaluation Table assignments to develop a 750-1,000 word review that includes the following sections:
- Title page
- Introduction section
- A comparison of research questions
- A comparison of sample populations
- A comparison of the limitations of the study
- A conclusion section, incorporating recommendations for further research
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center. An abstract is not required.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. Refer to the LopesWrite Technical Support articles for assistance.
NRS 493 Professional Capstone Practicum Essays GCU – Topic 6 Capstone Change Project Resources
Work with your preceptor to assess the organization for required resources needed for the strategic plan if the change proposal were to be implemented. Review your strategic
READ MORE >>
including ventilator-associated pneumonia signify poor compliance to hand hygi ...
READ MORE >>
students will initiate a preconference with the faculty and preceptor to review ...
You are not required to submit this NRS 493 Topic 1 Individual Success Plan Essay Paper assignment to LopesWrite.
CLICK HERE TO ORDER YOUR NRS 493 Topic 1 Individual Success Plan Essay Paper
NRS 493 Topic 1 Practice Experience Conference (Pre-Conference)
Students are required to initiate a preconference that will occur during the first week of class and must include the faculty member and the preceptor. Conferences may be conducted face-to-face or via synchronous technology such as Skype
READ MORE >>
