Our Previous Samples
NR451 Capstone Project Milestone 1 Practice Issue and Evidence SummaryNR451 CAPS ...
NR451 Capstone Project Milestone 1 Practice Issue and Evidence Summary
NR451 CAPSTONE PROJECT MILESTONE 1 PRACTICE ISSUE AND EVIDENCE SUMMARY
Capstone Project Milestone 1:
Practice Issue and Evidence Summary Worksheets
NR451 Capstone Project Milestone 1 Practice Issue and Evidence Summary Directions
1. Refer to the guidelines for specific details on how to complete this assignment.
2. Type your answers directly into the worksheets below.
3. Submit to the Dropbox by the end of Week 3, Sunday at 11:59 p.m. MT.
4. Post questions about this assignment to the Q & A Forum. You may also email questions to the instructor for a private response.

NR451 Capstone Project Milestone 1 Practice Issue and Evidence Summary Practice Issue Worksheet
- List the topic and include the citation for the systematic review you have selected:
- What is the practice issue you have identified related to the topic you have chosen?
- Define the scope of the practice issue:
- What is the practice area?
___ Clinical
___ Education
___ Administration
___ Other (List):
- How was the practice issue identified? (check all that apply)
___ Safety/risk management concerns
___ Unsatisfactory patient outcomes
___ Wide variations in practice
___ Significant financial concerns
___ Difference between hospital and community practice
___ Clinical practice issue is a concern
___ Procedure or process is a time waster
___ Clinical practice issue has no scientific base
__ Other:
- Describe the rationale for your checked selections:
- What evidence must be gathered? (check all that apply)
___ Literature search
___ Guidelines
___ Expert Opinion
___ Patient Preferences ___ Clinical Expertise
___ Financial Analysis
___ Standards (Regulatory, professional, community)
___ Other
- Describe the rationale for your checked selections:
NR451 Capstone Project Milestone 1 Practice Issue and Evidence Summary Worksheet
Directions: Please type your answers directly into the worksheet.
- Describe the practice problem in your own words with reference to the identified population, setting and magnitude of the problem in measurable terms:
- Type the complete APA reference for the systematic review article you chose from the list provided, It must be relevant to the practice issue you described above.
- Identify the objectives of the article.
- Provide a statement of the questions being addressed in the work and how they relate to your practice issue:
- Summarize (in your own words) the interventions the author(s) suggest to improve patient outcomes.
- Summarize the main findings by the authors of your systematic review including the strength of evidence for each main outcome. Consider the relevance to your project proposal for the Milestone 2 project paper.
- Outline evidence-based solutions that you will consider for your project.
- Discuss any limitations to the studies performed that you believe impacts your ability to utilize the research in your project.
Capstone Project Practice Issue and Evidence Summary – NR 451
NR 451 Capstone Project Milestone 1 Practice Issue and Evidence Summary Purpose
Clear identification of the practice issue is the first step in evidence-based nursing. Next, the evidence is reviewed to determine the best intervention to change practice outcomes. Completion of the milestone will include identification of the practice issue using the ACE Star Model of Knowledge Transformation and a review of the evidence that will support an intervention that will change outcomes. The evidence summary will be conducted through the ‘breaking down’ of a systematic review on your topic for your change project.
NR 451 Capstone Project Milestone 1 Practice Issue and Evidence Summary Course Outcomes
This Capstone Project assignment enables the student to meet the following course outcomes:
- CO4: Develops and outlines a scientific, systematic decision-making process to integrate critical thinking with clinical judgment to assure safe and effective outcomes. (PO4)
- CO8: Selects evidence for best practice when planning professional nursing care for individuals, families, aggregates, and communities. (PO8)
NR 451 Capstone Project Milestone 1 Practice Issue and Evidence Summary Due Dates
Milestone 1 consists of the completion of ONE form with two worksheets called the.courselearn.net/lms/content/1500/50031/NR451/NR451_W3_Milestone1_Evidence_Worksheet2.docx”>Practice Issue and Evidence Summary Worksheets. (Links to an external site.)Links to an external site. Complete both worksheets and submit the form by Sunday, 11:59 p.m. MT at the end of Week 3.
Points
Milestone 1 is worth175 points(75 points for the Practice Issue and 100 points for the Evidence Summary).
Practice Issue Worksheet Directions
- A tutorial with tips for completing this Capstone Project: Practice Issue and Evidence Summary – NR451 assignment may be viewed
- Choose the ONE systematic review topic that is of most interest to you, or most relevant to your practice situation, from
- Follow the grading criteria below to formulate your practice issue, which must be based on the topic of the systematic review you have selected.
- Use the worksheet to document the practice issue presented and approved by your instructor in the Week 2 Discussions.
- Your practice issue will be the same for all three Milestone assignments in this course.
- Please type your answers directly into the worksheet.
Evidence Summary Worksheet Directions
- Develop an evidence summary by following the grading criteria below.
- Document this on the evidence summary portion of the worksheet.
- You will use this worksheet to incorporate your evidence summary into your Week 4 Milestone 2 assignment.
- Please type your answers directly into the worksheet.
Academic Integrity Reminder
Chamberlain College of Nursing values honesty and integrity. All students should be aware of the Academic Integrity policy and follow it in all discussions and assignments.
By submitting this Capstone Project: Practice Issue and Evidence Summary – NR451 assignment, I pledge on my honor that all content contained is my own original work except as quoted and cited appropriately. I have not received any unauthorized assistance on this assignment.
Please see the grading criteria and rubrics on this page.
NOTE: Please use your browser’s File setting to save or print this page.
List of Approved Systematic Reviews
ORDER NOW
NR451 Capstone Project Milestone 1 Practice Issue and Evidence Summary Project
Directions: Please choose ONE topic and its corresponding systematic review that is of most interest to you, or most relevant to your practice. This systematic review will be the basis for your capstone project. Please refer to the guidelines for each milestone for more details.
Obstetrics/Delivery
Gupta, J. K., Sood, A., Hofmeyr, G. J., & Vogel, J. P. (2017). Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database of Systematic Reviews,Issue 5, Art. No.: CD002006.
Strobel, N. A., Arabena, K., East, C. E., Schultz, E.M., Kelaher, M., Edmond, K. M., … Chamberlain, C. (2017). Care co-ordination interventions to improve outcomes during pregnancy and early childhood (up to 5 years) (Protocol). Cochrane Database of Systematic Reviews, Issue 8. Art. No.: CD012761.
Health-Associated Infections (HAI)
Verbeek, J. H., Ijaz, S., Mischke, C., Ruotsalainen, J. H., Mäkelä, E., Neuvonen, K., … Mihalache, R. C. (2016). Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD011621.
Dumville, J. C., Gray, T. A., Walter, C. J., Sharp, C. A., Page, T., Macefield, R., … Blazeby, J. (2016). Dressings for the prevention of surgical site infection. Cochrane Database of Systematic Reviews, Issue 12. Art. No.: CD003091.
Wound Care
Walker, R. M., Gillespie, B. M., Thalib, L., Higgins, N. S., & Whitty, J. A. (2017). Foam dressings for treating pressure ulcers. Cochrane Database of Systematic Reviews, Issue 10. Art. No.: CD011332. DOI: 10.1002/14651858.CD011332.pub2.
Childhood/School Health
Hodder, R. K, Stacey, F. G., Wyse, R. J., O’Brien, K. M., Clinton-McHarg, T., Tzelepis, F., … Wolfenden, L. (2017). Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database of Systematic Reviews, Issue 9. Art. No.: CD008552. DOI: 10.1002/14651858.CD008552.pub3.
Parab, C. S, Cooper, C., Woolfenden, S., & Piper, S. M. (2013). Specialist home-based nursing services for children with acute and chronic illnesses. Cochrane Database of Systematic Reviews, Issue 6. Art. No.: CD004383. DOI: 10.1002/14651858.CD004383.pub3.
Hospital Readmissions
Hall, K. K., Chang, A. B., & O’Grady, K.F. (2016). Discharge plans to prevent hospital readmission for acute exacerbations in children with chronic respiratory illness (Protocol). Cochrane Database of Systematic Reviews, Issue 8. Art. No.: CD012315. DOI: 10.1002/14651858.CD012315.
NR451 Milestone 2: Design for Change Proposal
Purpose
You are to create a Design for Change proposal inclusive of your Practice Issue and Evidence Summary worksheet from your Project worksheet (PDF uploaded). Your plan is to convince your management team of a nursing problem you have uncovered and you feel is significant enough to change the way something is currently practiced. In the event you are not currently working as a nurse, please use a hypothetical clinical situation you experienced in nursing school, or nursing education issue you identified in your nursing program.
Rubric (PDF also uploaded)
Click to view and download the NR451 Milestone 2: Design for Change Proposal Rubric.
Points
Milestone 2 is worth 225 points.
Directions
- A tutorial with tips for completing this assignment may be viewed at https://atge.webex.com/atge/ldr.php?RCID=b0c912eaf53b4aabb1347a026466c60e
- Review the feedback you received from your instructor for worksheet, and use it to develop this milestone.
- Create a proposal for your Design for Change Capstone Project. Open the Milestone 2 Design Proposal Template. (PDF also uploaded)Use this to write your paper. You will include the information from Milestone 1, your practice issue and evidence summary worksheets, as you compose this proposal. Your plan is to convince your management team of a practice problem you have uncovered that is significant enough to change current practice.
- The format for this proposal will be a paper following the Publication manual of APA6th
- The paper is to be five pages.
- As you organize your information and evidence, include the following topics.
- Introduction: Write an introduction but do not use “Introduction” as a heading in accordance with the rules put forth in the Publication manual of the American Psychological Association (2010, p. 63). Introduce the reader to the plan with evidence-based problem identification and solution.
- Change Model Overview: Overview of the ACE Star model (the model we have been discussing this session); define the scope of the EBP; identify the stakeholders, and determine the responsibility of the team members.
- Evidence: Conduct internal and external searches of evidence; integrate and summarize the evidence summary worksheet from Milestone 1; develop a recommendation for change.
- Translation: develop a hypothetical action plan; include measurable outcomes, reporting to stakeholders; identify next steps and disseminate the findings.
- Conclusion: Provide a clear and concise summary, inclusive of the problem issue, the five points of the ACE Star change model; and ways to maintain the change plan.
- Citations and References must be included to support the information within each topic area. Refer to the APA manual, Chapter 7, for examples of proper reference format. In-text citations are to be noted for all information contained in your paper that is not your original idea or thought. Ask yourself, “How do I know this?” and then cite the source. Scholarly sources are expected, which means using peer-reviewed journals and credible websites.
- Tables and Figures may be added as appropriate to the project. They should be embedded within the body of the paper (see your APA manual for how to format and cite). Creating tables and figures offers visual aids to the reader and enhances understanding of your literature review and design for change.
NR 451 Week 6: Capstone Project: Milestone 3: Educating Staff (graded) Assignment
Capstone Project Milestone 3: Educating Staff: Implementing Change Guidelines
NR 451 Week 6: Capstone Project: Milestone 3 Purpose
The purpose of this assignment is to create the Educating Staff: Implementing Change Project PowerPoint presentation. Your plan is to educate the staff that will be involved in the pilot program. NR451 Capstone Project Milestone 1: Practice Issue and Evidence Summary. You will need to educate them on the problem, show the supporting evidence, and how your pilot plan will be implemented.
NR 451 Week 6: Capstone Project: Milestone 3 Course Outcomes
This assignment enables the student to meet the following Course Outcomes.
- CO2: Proposes leadership and collaboration strategies for use with consumers and other healthcare providers in managing care and/or delegating responsibilities for health promotion, illness prevention, health restoration and maintenance, and rehabilitative activities. (PO2)
- CO3: Communicates effectively with patient populations and other healthcare providers in managing the healthcare of individuals, families, aggregates, and communities. (PO3)
- CO7: Integrates the professional role of leader, teacher, communicator, and manager of care to plan cost-effective, quality healthcare to consumers in structured and unstructured settings. (PO7)
NR451 Capstone Project Milestone 1: Practice Issue and Evidence Summary Due Date
Milestone 3 consists of the PowerPoint presentation Educating Staff: Implementing Change Project. Submit the PowerPoint file by Sunday, 11:59 p.m. MT by the end of Week 6.
Points
Milestone 3 is worth 200 points.
NR 451 Week 6: Capstone Project: Milestone 3 Directions
- A tutorial with tips on completing this assignment may be viewed at https://atge.webex.com/atge/ldr.php?RCID=8912a4b3268463312e115abf9e73efd6 (Links to an external site.)Links to an external site.
- Create an educational presentation for staff before the launch of your change project. This should inform the staff of the problem, your potential solution, and their role in change project.
- The format for this proposal will be a PowerPoint presentation.
- Tutorial: For those not familiar with the development of a PowerPoint slideshow, the following link to the Microsoft website may be helpful. http://office.microsoft.com/en-us/support/training-FX101782702.aspx. The Chamberlain Student Success Strategies (SSPRNBSN) offers a module on Computer Literacy that contains a section on PowerPoint. You can access SSPRNBSN from your Canvas course list.
- The length of the PowerPoint presentation should be 15-20 slides; excluding the title and reference slides.
- Below are the main topics or bullet points for your slides:
- Title slide
- Description of the Ace Star change model that you have used for this project.
- Practice Issue
- Scope of the problem—use basic statistics from what you know of the problem in your work area.
- Your team/stakeholders
- Evidence to support your need for change—from your Evidence Summary
- Action Plan
- Timeline for the plan
- The nurse’s role and responsibility in the pilot program
- Procedure (what steps are to be taken to complete this change process, from start to finish?)
- Forms that will be used (if applicable)
- Resources available to the staff—including yourself
- Summary
- References
- Citations and References must be included to support the information within each topic area. Refer to the APA manual, Chapter 7, for examples of proper reference format. Citations are to be noted for all information contained in your paper that is not your original idea or thought. Ask yourself, “How do I know this?” and then cite the source. Scholarly sources are expected, which means choose peer-reviewed journals and credible websites.
NR 451 Week 6: Capstone Project: Milestone 3 Guidelines
- Application: Use Microsoft PowerPoint 2010 or later.
- Length: The PowerPoint slide show is expected to be between 15-20 slides in length (not including the title slide and reference list slides).
- Submission: Submit your by 11:59 p.m. Sunday by the end of Week 6.
- Late Submission: See the Policies on late submissions.
- Tutorial: For those not familiar with the development of a PowerPoint slideshow, the following link to the Microsoft website may be helpful. http://office.microsoft.com/en-us/support/training-FX101782702.aspx. The Chamberlain Student Success Strategies (CCSSS) offers a module on Computer Literacy that contains a section on PowerPoint. The link to SSP CCSSS may be found under your course list in the student portal.
Best Practices in Preparing a PowerPoint Presentation
The following are best practices in preparing this presentation.
- Be creative.
- Incorporate graphics, clip art, or photographs to increase interest.
- Make easy to read with short bullet points and large font.
- Use speaker notes (found under the section View and “Notes” in the PowerPoint template you choose. These are for your personal use to use as a reference if you are giving your presentation to an audience and they help faculty identify what you will speak to your audience about.
- Review directions thoroughly.
- Cite all sources within the slides with (author, year) as well as on the Reference slide.
- Proofread prior to final submission.
- Spell check for spelling and grammar errors prior to final submission.
**Academic Integrity Reminder**
Chamberlain College of Nursing values honesty and integrity. All students should be aware of the Academic Integrity policy and follow it in all discussions and assignments.
By submitting this assignment, I pledge on my honor that all content contained is my own original work except as quoted and cited appropriately. I have not received any unauthorized assistance on this assignment.
Please see the grading criteria and rubrics on this page.
READ MORE >>
NR451 Capstone Project Systematic ReviewsList of Approved Systematic Reviews NR4 ...
NR451 Capstone Project Systematic Reviews
List of Approved Systematic Reviews
NR451 Capstone Project
Directions: Please choose ONE topic and its corresponding systematic review that is of most interest to you, or most relevant to your practice. This systematic review will be the basis for your capstone project. Please refer to the guidelines for each milestone for more details.
Promoting breastfeeding
Sinha, B., Chowdhury, R., Sankar, M. J., Martines, J., Taneja, S., Mazumder, S., … Bhandari, N. (2015). Interventions to improve breastfeeding outcomes: A systematic review and meta-analysis. Acta Paediatrica, 104, 114-134. doi:10.1111/apa.13127.
Chamberlain Library Permalink: http://proxy.chamberlain.edu:8080/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=a2h&AN=110726890&site=eds-live&scope=site
Preventing central venous catheter-related infections
Lai, N. M., Lai, N. A., O’Riordan, E., Chaiyakunapruk, N., Taylor, J. E., & Tan, K. (2016). Skin antisepsis for reducing central venous catheter-related infections. Cochrane Database of Systematic Reviews, (7), CD010140. doi:10.1002/14651858.CD010140.pub2.
Chamberlain Library Permalink: http://onlinelibrary.wiley.com.proxy.chamberlain.edu:8080/doi/10.1002/14651858.CD010140.pub2/full
Increasing health insurance coverage for vulnerable populations
Jia, L., Yuan, B., Huang, F., Lu, Y., Garner, P., & Meng, Q. (2014). Strategies for expanding health insurance coverage in vulnerable populations. Cochrane Database of Systematic Reviews, (11), 1-41. CD008194. doi:10.1002/14651858.CD008194.pub3.
Chamberlain Library Permalink: http://proxy.chamberlain.edu:8080/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=25425010&site=eds-live&scope=site
Preventing teen pregnancy and sexually-transmitted disease
Mason-Jones, A. J., Sinclair, D., Mathews, C., Kagee, A., Hillman, A., & Lombard, C. (2016). School-based interventions for preventing HIV, sexually transmitted infections, and pregnancy in adolescents. Cochrane Database of Systematic Reviews, (11), CD006417. doi:10.1002/14651858.CD006417.pub3.
Chamberlain Library Permalink: http://proxy.chamberlain.edu:8080/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=27824221&site=eds-live&scope=site
Reducing hospital readmissions
Mistiaen, P., & Poot, E. (2006). Telephone follow-up, initiated by a hospital-based health professional, for post discharge problems in patients discharged from hospital to home. Cochrane Consumers and Communication Group. (4), CD004510. doi:10.1002/14651858.CD004510.pub3.
Chamberlain Library Permalink: http://onlinelibrary.wiley.com.proxy.chamberlain.edu:8080/doi/10.1002/14651858.CD004510.pub3/full
Obstetrics/Delivery
Lemos, A., Amorim, M. M. R., Dornelas de Andrade, A., Souza, A. I., Calbral Filho, J. E., & Correia, J. B. (2017). Pushing/bearing down methods for the second stage of labour. Cochrane Database of Systematic Reviews 2017, Issue 3. Art. No.: CD009124. DOI: 10.1002/14651858.CD009124.pub3.
Chamberlain Library Permalink: http://onlinelibrary.wiley.com.proxy.chamberlain.edu:8080/doi/10.1002/14651858.CD009124.pub3/full
Moore, E. R., Bergman, N., Anderson, G. C., & Medley, N. (2016). Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No.: CD003519. DOI: 10.1002/14651858.CD003519.pub4.
Chamberlain Library Permalink: http://onlinelibrary.wiley.com.proxy.chamberlain.edu:8080/doi/10.1002/14651858.CD003519.pub4/full
Health-Associated Infections (HAI)
Webster, J., & Osborne, S. (2015). Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database of Systematic Reviews 2015, Issue 2. Art. No.: CD004985. doi:10.1002/14651858.CD004985.pub5.
Chamberlain Library Permalink: http://onlinelibrary.wiley.com.proxy.chamberlain.edu:8080/doi/10.1002/14651858.CD004985.pub5/full
Wound Care
Moore, Z. E. H., Webster, J., & Samuriwo, J. (2015). Wound-care teams for preventing and treating pressure ulcers. Cochrane Database of Systematic Reviews 2015, Issue 9. Art. No.: CD011011. doi:10.1002/14651858.CD011011.pub2.
Chamberlain Library Permalink: http://onlinelibrary.wiley.com.proxy.chamberlain.edu:8080/doi/10.1002/14651858.CD011011.pub2/full
Childhood/School Health
Janicke, D. M., Steele, R. G., Gayes, L. A., Lim, C. S., Clifford, L. M., Schneider, E. M., & … Westen, S. (2014). Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. Journal of Pediatric Psychology, 39(8), 809-825.
Chamberlain Library Permalink:
http://proxy.chamberlain.edu:8080/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=edswss&AN=000343398100004&site=eds-live&scope=site
Hospital Readmissions
Leppin, A. L., Gionfriddo, M. R., Kessler, M., Brito, J. P., Mair, F. S., Gallacher, K., & … Montori, V. M. (2014). Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Internal Medicine, 174(7), 1095-1107. doi:10.1001/jamainternmed.2014.1608
Chamberlain Library Permalink: http://proxy.chamberlain.edu:8080/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=24820131&site=eds-live&scope=site
Fox, M. T., Persaud, M., Maimets, I., Brooks, D., O’Brien, K., & Tregunno, D. (2013). Effectiveness of early discharge planning in acutely ill or injured hospitalized older adults: A systematic review and meta-analysis. BMC Geriatrics, 13(1), 1. doi:10.1186/1471-2318-13-70
Chamberlain Library Permalink: http://proxy.chamberlain.edu:8080/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=edb&AN=89638554&site=eds-live&scope=site
READ MORE >>
NR501 Theoretical Basis for Advanced Nursing Practice Discussion EssaysNR501 The ...
NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays
NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays
NR501 Week 1 Discussion
Nursing Theory
For many? Students enrolled in NR501, this is an initial nursing course? Theory.? So, let’s have a debate.? Is nursing theory important to the? Nursing profession? In particular, is it important for nurse practitioners? Does theory inform nurse practitioner practice??
If you believe it is important, explain why it is? useful.? f you do not believe it is useful, explain why nursing theory. Is not necessary to the profession?
NR501 Week 2 Discussion
Ways of Knowing
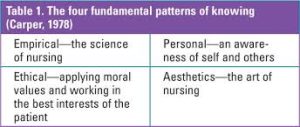
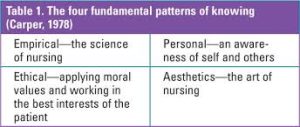
Nursing knowledge is classified in various ways, one of which is Carper’s Patterns of Knowing (Carper, 1978). Carper’s framework offers a lens through which the nurse can reflect upon insights acquired through empirical, ethical, personal, and aesthetic knowledge (Carper, 1978). NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays
Through intentional reflection using Carper’s Patterns of Knowing, nurses can process experiential learning and knowledge acquired through practice NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays.
This assignment aims to reflect upon a specific practice situation and better understand the professional knowledge and insights obtained through that experience.
Criteria for Content
Think of a surprising or challenging practice situation in which you felt underprepared, unprepared, or uncomfortable.
Select an important nursing issue/topic inherent to the identified situation NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays.
Briefly? explain the situation
Identify the nursing issue inherent in the identified situation
Use Carper’s Patterns of Knowing to analyze the situation as a method of refection. In your discussion, address ONE of the following Patterns of Knowing:
- What do you think was the underlying reason for the situation? (Esthetics)
- What were your thoughts and feeling in the situation? (Personal)
- What was one personal belief that impacted your actions? (Ethics)
- What evidence in nursing literature supports the nursing importance of the identified issue? (Empirical)
What new insights did you gain through this reflective practice opportunity? How will this apply to your practice as a nurse practitioner? Be sure to use scholarly literature to support your position NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays.
NR501 Week 3 Discussion Steps of Concept Analysis
At the end of Week 3, your concept analysis is due. This discussion provides an opportunity to start this assignment. Select a nursing concept supported by a nursing theory, and address the following components included in a concept analysis:?
- Definition of concept and discussion of the concept in the nurse practitioner role?
- Identification of three attributes of the concept?
- Description of one antecedent and one consequence of the concept?
- Identification of two empirical referents?
- A brief explanation of theoretical applications of the concept (How is the concept relevant to a nursing theory?)?
This information does not have to be comprehensive but provides a foundation for the upcoming assignment. Be sure to include scholarly references NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays.
NR501 Week 4 Discussion Nursing Theory
Identify your specialty area of NP practice. Select a nursing, borrowed, or interdisciplinary theory provided in the lesson plan or one of your findings. Address the following:
- Origin
- Meaning and scope
- Logical adequacy
- Usefulness and simplicity
- Generalizability
- Testability
Finally, provide an example of of how the theory could be used to improve or evaluate the practice quality in your specific setting. What rationale can you provide that validates the theory as applied to the role of the nurse practitioner?
NR501 Week 5 Discussion
Culture and Caring Theories
Which of the culture and caring theories most resonates with you for your practice as an NP? How does the theory integrate the nursing paradigm?? What parts of the theory do you identify with? How does the theory help to meet CLAS standards to advance health equity?
NR501 Week 6 Discussion Literature Review
Locate a scholarly journal article that uses either a health behavior theory or the Praxis Theory of Suffering as the basis for evidence-based research. Choose an article DIFFERENT than those provided in the weekly readings.
Summarize the research presented. How was the theory used? How do the research findings either support or refute the use of the theory in practice? How could you use the research in your practice as an NP?
NR501 Week 8 Discussion
In Week 7, you posted your Kaltura presentation to the Week 8 discussion area. This week, you will view and comment on peer presentations. For full credit, view and comment on at least TWO peer presentations by Saturday at 11:59 PM MT.
Your post should be substantive and professional and include at least one scholarly resource.
NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays References
Carper, B.A. (1978). Fundamental patterns of knowing in nursing. Retrieved 8 September 2019 from
https://www.google.co.ke/url?sa=t&source=web&rct=j&url=https://pdfs.semanticscholar.org/8871/eb88fb06168bb31e20e9c54e57920e575a47.pdf&ved=2ahUKEwje0JrqscHkAhVClFwKHYXzAgsQFjAQegQICRAB&usg=AOvVaw0CEuuz-eqnIwVMqcmUI55E
Haswell, N. (2019). The four ethical principles and their application in aesthetic practice. Journal of Aesthetic Nursing, 8(4), 177-179. Doi: 10.12968/joan.2019.8.4.177 NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays
Schmidt, L.A., Nelson, D. & Godfrey, L. (2003). A clinical ladder program based on Carper’s fundamental patterns of knowing in nursing. JONA, 33(3), 146-152. Doi: 10.1097/00005110-200303000-00005
Quaglietti, S., Blum, L. & Ellis, V. (2004). The role of the adult nurse practitioner in palliative care. Journal of Hospice and Palliative Nursing, 6(4), 209-214. Doi: 10.1097/00129191-200410000-00009 NR501 Theoretical Basis for Advanced Nursing Practice Discussion Essays
READ MORE >>
NR501 Week 2 Reflective Assignment Carper’s Pattern of Knowing Reflective Ess ...
NR501 Week 2 Reflective Assignment Carper’s Pattern of Knowing Reflective Essay
Fundamental Nursing Lessons Learnt from a Difficult Situation in Practice: Carper’s Pattern’s of Knowing in Nursing.
The Practical Situation Experienced
Nursing is about promoting health, preventing illness, and restoring hope. However, there are situations in which a nurse can find themselves almost helpless with regard to all the three above. A case in point is the prospect of having to reassure a patient with terminal illness by giving them hope yet you know very well that they may not have long to live.
Even more daunting is the task requiring you as the nurse to convince the patient and her relatives that they will benefit from hospice care. This is the situation I once found myself in. I was faced with this situation of a 37 year-old who had advanced ovarian cancer with a very poor prognosis. It was obvious that what she needed most in her…
Week 2 Assignment: Reflective Essay
Purpose
Nursing knowledge is classified in a variety of ways, one of which is Carper’s Patterns of Knowing (Carper, 1978). Carper’s framework offers a lens through which the nurse can reflect upon insights acquired through empirical, ethical, personal, and aesthetic knowledge (Carper, 1978).
Through intentional reflection using Carper’s Patterns of Knowing, nurses can process experiential learning and knowledge acquired through practice. This assignment aims to reflect upon a specific practice situation and better understand the professional knowledge and insights obtained through that experience.
Course Outcomes on NR501 Week 2 Reflective Assignment
Through this assessment, the student will meet the following Course Outcomes:
- Demonstrate logical and creative thinking in analyzing and applying theory to nursing practice. (CO #1)
- Examine broad theoretical concepts as foundational to advanced nursing practice roles. (CO #3)
Requirements
Criteria for Content
- Think of a surprising or challenging practice situation in which you felt underprepared, unprepared, or uncomfortable.
- Select an important nursing issue/topic that was inherent to the identified situation.
- As a method of refection, use Carper’s Patterns of Knowing to analyze the situation. In a two- to three-page paper address the following:
- Briefly explain the situation
- Identify the nursing issue inherent in the identified situation
- What do you think was the underlying reason for the situation? (Esthetics)
- What were your thoughts and feeling in the situation? (Personal)
- What was one personal belief that impacted your actions? (Ethics)
- What evidence in nursing literature supports the nursing importance of the identified issue? (Empirical)
- What new insights did you gain through this reflective practice opportunity?
Preparing the paper
- Application: Use Microsoft Word 2016™ to create the written component of this assessment.
- Length:
- The paper (excluding the title page and reference page) should be at least two but no more than three pages.
- A minimum of two (2) scholarly literature sources must be used.
- Submission: Submit your file to the Canvas course site by the due date/time indicated.
Best Practices in Preparing the Reflective Essay
The following are best practices in preparing this reflective essay.
- Review directions thoroughly.
- Follow assignment requirements.
- Make sure all elements on the grading rubric are included.
- Rules of grammar, spelling, word usage, and punctuation are followed and consistent with formal, scholarly writing.
- Because the paper is a reflective essay, first person is acceptable for this assignment.
- Title page, running head, body of paper, and reference page must follow APA guidelines as found in the 6th edition of the manual. This includes the use of headings for each section of the paper except for the introduction where no heading is used.
- Ideas and information that come from scholarly literature must be cited and referenced correctly.
- A minimum of two (2) scholarly literature sources must be used.
- Abide by CCN academic integrity policy.
Example Reflective Assignment on Aboriginal People
As a nurse, my beliefs and attitudes rely massively on my culture because I often apply various socio-cultural principles when delivering patient care. One of the most profound cultural aspects that shape my profession is religion. As a Christian, I have a different worldview regarding diseases and healing. In this sense, I believe that God created humans in his image to enjoy his companionship and favor.
However, human’s sinful nature destroyed their relationship with God. As a result, God punishes human races through diseases and other calamities because they shifted from mainstream guidelines (Choudry et al., 2018). Consequently, the only way to rekindle the lost love and companionship is through repentance and acknowledging Jesus’s role in restoring humankind.
Alongside Christian narratives of creation, fall, redemption, and restoration, my culture requires people to show impartiality, justice, and love to others. Arguably, these ethical guidelines blend well with the principles of evidence-based nursing practices.
In this sense, the evidence-based practice model (EBP) requires healthcare professionals to encourage justice, beneficence, nonmaleficence, and patient autonomy (Lulé et al., 2019). The ability to incorporate my beliefs and attitudes into the nursing profession is fundamental in enhancing my cultural competence to understand other people’s needs without providing biased care.
Cultural competence is crucial for care providers because it helps them understand and integrate cultural intelligence into healthcare delivery operations. Jongen et al. (2018) argue that healthcare professionals must improve cultural competence to serve the needs of a diverse population. On the other hand, Nair and Adetayo (2019) present cultural competence as “the ability to collaborate effectively with individuals from different cultures, and such competence improves healthcare experiences and outcomes.”
I believe that understanding other people’s cultural values and beliefs is the basic step of incorporating social determinants of health in mainstream care delivery. As a result, it is possible to understand factors that affect the underserved populations facing various healthcare concerns because of socio-economic issues, including low-level education, poverty, low income, and discrimination.
My cultural beliefs and attitudes enhance the desire to work with Aboriginal and Torres Strait Islander people because I feel that we share core values, including the role of religion in promoting people’s health and wellness. According to Davy et al. (2017), Aboriginal and Torres Strait Islander communities share cultural aspects that validate the synergies between culture, land, community, and family in determining people’s well-being.
In this sense, the definition of health for such native communities extends beyond physical and psychological dimensions (Dew et al., 2019). When considering social institutions that promote people’s interpretation of health and well-being among Aboriginal and Torres Strait Islander communities, it is valid to argue that any healthcare intervention should focus on capitalizing on unique connections and social institutions.
As a professional nurse determined to work with vulnerable and underserved populations, I believe that process honesty, respect for diversities, effective communication, and awareness are fundamental factors for understanding social determinants for these communities. Fortunately, my cultural beliefs and values encourage commitment, persistence, humility, and honesty when interacting with people from different cultures.
Social Responsibility to Work for Changes in Aboriginal Health
As a nurse, I have a social responsibility to work for changes in Aboriginal health because native communities face various challenges when accessing mainstream healthcare services. According to Davy et al. (2017), Aboriginal and Torres Strait Islander people experience a similar prevalence of chronic diseases to people in developing countries, although Australia is a developed country with a relatively well-funded healthcare system.
In this sense, chronic diseases such as cardiovascular conditions and diabetes are the leading causes of death in these communities. Also, kidney diseases pose higher risks to Aboriginal and Torres Strait Islander people compared to non-Indigenous Australians.
Arguably, many reasons explain health disparities among indigenous Australians, such as Aboriginal and Torres Strait Islander people. Wilson et al. (2020) argue that such large gaps in disease and life experiences between indigenous and non-Indigenous Australians rely massively upon poorer determinants of health, discriminatory practices, and the history of marginalization.
Undoubtedly, these factors compromise people’s access to health care and highlight the essential role that healthcare professionals should play in enabling Aboriginal patients to participate in quality healthcare services.
Although the history of marginalization, discriminatory practices, poor social determinants of health, and exclusion affect how native Australians access healthcare services, it is essential to approach such a situation from a positive perspective. In this sense, evaluating community potentials and avenues that determine their well-being is fundamental.
According to Wilson et al. (2017), Aboriginal and Torres Strait Islander people have a robust and rich history because they are among the oldest cultures in the world. Essentially, their endowed cultural values and beliefs are vital in demonstrating strength, resilience, and tenacity. Also, these communities rely massively upon social systems and cultural institutions such as religion and families as the primary aspects of health and well-being.
Undoubtedly, the presence of firmly held socio-cultural beliefs and practices among indigenous Australians presents various viable opportunities for allied health professionals to create changes. Firstly, I believe that allied health professionals (HPs) and Aboriginal health workers should collaborate in determining the trajectories of healthcare systems.
However, working closely with Aboriginal health workers and community members requires cultural competence because of the potentially varying socio-cultural aspects (Jongen et al., 2019). One of the basic requirements for allied health professionals working with indigenous communities is understanding the implications of colonialism history to health.
Taylor et al. (2020) argue that colonization had a devastating impact on traditional lifestyles because it led to lower education levels, unemployment, shorter life expectancy, and health disparities. As a result, nurses should understand these historical developments to develop informed healthcare frameworks for addressing poorer social determinants of health.
As I endeavor to work with Aboriginal and Torres Strait Islander people, I must deconstruct the conflicting opinions that allied health professionals lack culturally appropriate healthcare frameworks to mainstream care services to the underserved population in Australia. For instance, I believe that such a perception persists because of normalizing discriminative healthcare services, where indigenous people receive poor services compared to non-Indigenous Australians.
As a result, effective collaboration between healthcare professionals, high-level cultural competence, and evidence-based practice are crucial approaches to reducing health disparities among native communities (Nash & Arora, 2021). I am confident that I have a social responsibility to act as a change agent in improving the health trajectory of Aboriginal and Torres Strait Islander people by engaging them in nursing research, advocating for their inclusion in mainstream Australian healthcare, and encouraging high-level cultural competence.
NR501 Week 2 Reflective Assignment References
Choudry, M., Latif, A., & Warburton, K. (2018). An overview of the spiritual importance of end-of-life care among the five major faiths of the United Kingdom. Clinical Medicine, 18(1), 23-31. https://doi.org/10.7861/clinmedicine.18-1-23
Davy, C., Kite, E., Sivak, L., Brown, A., Ahmat, T., & Brahim, G. et al. (2017). Towards the development of a wellbeing model for Aboriginal and Torres Strait Islander peoples living with chronic disease. BMC Health Services Research, 17(1). https://doi.org/10.1186/s12913-017-2584-6
Dew, A., Barton, R., Gilroy, J., Ryall, L., Lincoln, M., & Jensen, H. et al. (2019). Importance of Land, family, and culture for a good life: Remote Aboriginal people with disability and carers. Australian Journal of Social Issues, 55(4), 418–438. https://doi.org/10.1002/ajs4.96
Jongen, C., McCalman, J., & Bainbridge, R. (2018). Health workforce cultural competency interventions: a systematic scoping review. BMC Health Services Research, 18(1). https://doi.org/10.1186/s12913-018-3001-5
Jongen, C., McCalman, J., Campbell, S., & Fagan, R. (2019). Working well: strategies to strengthen the workforce of the Indigenous primary healthcare sector. BMC Health Services Research, 19(1). https://doi.org/10.1186/s12913-019-4750-5
Lulé, D., Kübler, A., & Ludolph, A. (2019). Ethical Principles in patient-centered medical care to support quality of life in amyotrophic lateral sclerosis. Frontiers In Neurology, 10. https://doi.org/10.3389/fneur.2019.00259
Nair, L., & Adetayo, O. (2019). Cultural Competence and Ethnic Diversity in Healthcare. Plastic And Reconstructive Surgery – Global Open, 7(5), e2219. https://doi.org/10.1097/gox.0000000000002219
Nash, S., & Arora, A. (2021). Interventions to improve health literacy among Aboriginal and Torres Strait Islander Peoples: a systematic review. BMC Public Health, 21(1). https://doi.org/10.1186/s12889-021-10278-x
Taylor, E., Lyford, M., Parsons, L., Mason, T., Sabesan, S., & Thompson, S. (2020). “We’re very much part of the team here”: A culture of respect for the Indigenous health workforce transforms Indigenous health care. PLOS ONE, 15(9), e0239207. https://doi.org/10.1371/journal.pone.0239207
Wilson, A., Kelly, J., Jones, M., O’Donnell, K., Wilson, S., Tonkin, E., & Magarey, A. (2020). Working together in Aboriginal health: a framework to guide health professional practice. BMC Health Services Research, 20(1). https://doi.org/10.1186/s12913-020-05462-5
Fundamental Nursing Lessons Learnt from a Difficult Situation in Practice: Carper’s Pattern’s of Knowing in Nursing
The Practical Situation Experienced
Nursing is about promoting health, preventing illness, and restoring hope. However, there are situations in which a nurse can find themselves almost helpless with regard to all the three above. A case in point is the prospect of having to reassure a patient with terminal illness by giving them hope yet you know very well that they may not have long to live.
Even more daunting is the task requiring you as the nurse to convince the patient and her relatives that they will benefit from hospice care. This is the situation I once found myself in. I was faced with this situation of a 37 year-old who had advanced ovarian cancer with a very poor prognosis. It was obvious that what she needed most in her last days would be round-the-clock hospice care for especially pain relief.
The task, therefore, of convincing her together with her relatives to follow this route fell on me. Needless to say, I felt not only unprepared, but also uncomfortable because I knew there was no hope of her surviving for long. Yet I had to give her a reason to look forward to the next day.
The nursing issue inherent in this situation was the need for apt, caring and tactful guidance and counselling as an important role of me as the nurse in this end-of-life situation. I had to not only help the patient and her relatives make the right decision of checking into a hospice, but also give them convincing reasons why they needed to do so. This was not an easy mission to accomplish.
Reflection on the Situation Based on Carper’s Patterns of Knowing
Four facets of nursing knowledge have been identified as empirics or the scientific basis of nursing, esthetics or the consideration of nursing as an art, ethics or the morality in nursing, and the personal knowledge component of nursing (Carper, 1978; Schmidt et al., 2003). On empirics, therefore, I needed to be armed with evidence that hospice care indeed is beneficial for this patient and her family.
This is the evidence that I needed to base my argument on in trying to convince them to accept hospice care. Quaglietti, et al. (2004) have stated that the palliative care offered in the hospice takes care of the patient’s and her family’s expectations in terms of care. They continue that nurse practitioners (NPs) are well placed to meet these expectations.
On esthetics, empathy is the single most important factor in mastering the art of offering nursing care to patients (Carper, 1978). This was the underlying reason for the situation – need for empathy. Experience had taught me that to gain the patient’s trust and confidence; I as the nurse must feel genuine empathy for them. This way they will make less effort to accept any proposal such as going into hospice care.
On personal knowledge, Carper (1978) identifies interpersonal interaction as the barometer with which this knowledge is measured and gained. In this scenario, my personal feeling was that I had to relate with both the patient and her relatives at a personal level by establishing a personal bond with them. In doing this, I had to first know myself and confront my own personal fears and shortcomings.
Last but not least on ethics, I had to be aware that I had a moral obligation to only offer suggestions that would bring the greatest good to the patient and by extension her family (beneficence). Also, whatever suggestion or intervention that I suggested had to be devoid of the possibility of causing harm to the patient (nonmaleficence). But, most importantly, it dawned on me that I had to respect the decision of the patient and her relatives at the end (respect for autonomy) (Haswell, 2019).
Summary
This experience was indeed rich in knowledge for me. I learnt that the four factors of nursing knowledge are present in all practical nursing situations. Thus the double insight I got was the importance of evidence-based practice decisions and the power of empathy. Intentional reflective nursing practice is therefore imperative for improved future care.
References on NR501 Week 2 Reflective Assignment
Carper, B.A. (1978). Fundamental patterns of knowing in nursing. Retrieved 8 September 2019 from
https://www.google.co.ke/url?sa=t&source=web&rct=j&url=https://pdfs.semanticscholar.org/8871/eb88fb06168bb31e20e9c54e57920e575a47.pdf&ved=2ahUKEwje0JrqscHkAhVClFwKHYXzAgsQFjAQegQICRAB&usg=AOvVaw0CEuuz-eqnIwVMqcmUI55E
Haswell, N. (2019). The four ethical principles and their application in aesthetic practice. Journal of Aesthetic Nursing, 8(4), 177-179. Doi: 10.12968/joan.2019.8.4.177
Schmidt, L.A., Nelson, D. & Godfrey, L. (2003). A clinical ladder program based on Carper’s fundamental patterns of knowing in nursing. JONA, 33(3), 146-152. Doi: 10.1097/00005110-200303000-00005
Quaglietti, S., Blum, L. & Ellis, V. (2004). The role of the adult nurse practitioner in palliative care. Journal of Hospice and Palliative Nursing, 6(4), 209-214. Doi: 10.1097/00129191-200410000-00009
READ MORE >>
the three required elements below conclusion and reference page NR506NP Full C ...
You are now employed as an NP in primary care. Choose one performance measure from one of the six domains of care
READ MORE >>
economic and political factors (CO2)Demonstrate professional and personal growt ...
READ MORE >>
NR506NP Full Course AssignmentsNR506NP Healthcare Policy and LeadershipNR506NP F ...
NR506NP Full Course Assignments
NR506NP Healthcare Policy and Leadership
NR506NP Full Course Assignments Week 1 Discussion
Barriers to Practice
Purpose
Discuss barriers to practice as an APN in one’s state from both a state and national perspective. Research methods to influence policy change from various forms of competition, state legislative and executive branches of government and interest groups.
Activity Learning Outcomes
- Through this discussion, the student will demonstrate the ability to:
- Discuss the history of policy development and policy making in nursing (CO1)
- Examine different types of policy and their relationships to healthcare policy (CO1)
- Explain current barriers to practice for advanced practice nurses (CO2)
- Discuss health policy and methods of lifting barriers to practice (CO2)
NR506NP Full Course Assignments Requirements:
- Using the readings from this week as well as outside reliable resources to:
- Identify and describe practice barriers for APNs in your state and discuss these barriers on a state and national level.
- Identify forms of competition on the state and national level that interfere with APN’s ability to practice independently.
- Identify the lawmakers at the state level (i.e., key members of the state’s legislative branch and executive branch of government)
- Discuss interest groups that exist at the state and national levels that influence APN policy.
- Discuss methods used to influence change in policy in forms of competition, state legislative and executive branches of government and interest groups.
NR506NP Healthcare Policy and Leadership Week 2 Discussion
Organizational Change and Ethical-Legal Influences in Advanced Practice Nursing Case Study
Purpose
The purpose of this discussion is to discuss organizational changes and ethical-legal influences in a clinical scenario at an out-patient family practice. Students will explore potential effects on patient outcomes and ethical and legal implications for members of the heath care team as a result of illegal behaviors. Students will develop strategies that result in prevention of untoward outcomes that result in a positive practice culture NR506NP Full Course Assignments.
Activity Learning Outcomes
- Through this discussion, the student will demonstrate the ability to:
- Demonstrate effective leadership styles in the management of organizational change (CO3)
- Interpret various forms of ethical theories and application into practice (CO4)
- Discuss practice guidelines and malpractice prevention (CO2)
NR506NP Full Course Assignments Requirements:
You are a family nurse practitioner employed in a busy primary care office. The providers in the group include one physician and three nurse practitioners.
The back office staff includes eight medical assistants who assist with patient care as well as filing, answering calls from patients, processing laboratory results and taking prescription renewal requests from patients and pharmacies NR506NP Full Course Assignments.
Stephanie, a medical assistant, has worked in the practice for 10 years and is very proficient at her job. She knows almost every patient in the practice, and has an excellent rapport with all of the providers.
Mrs. Smith was seen today in the office for an annual physical. Her last appointment was a year ago for the same reason. During this visit, Mrs. Smith brought an empty bottle of amoxicillin with her and asked if she could have a refill. You noted the patient’s name on the label, and the date on the bottle was 1 week ago.
You also noted your name printed on the label as the prescriber. The patient admitted that she called last week concerned about her cough and spoke to Stephanie. You do not recall having discussed this patient with Stephanie nor do the other providers in the practice NR506NP Full Course Assignments.
Case Study Questions:
What are the potential ethical and legal implications for each of the following practice members?
- Medical assistant
- Nurse Practitioner
- Medical Director
- Practice
What strategies would you implement to prevent further episodes of potentially illegal behavior?
What leadership qualities would you apply to effect a positive change in the practice?? Be thinking about the culture of the practice.
Week 3 Discussion
Review the Hedis Measures and select ONE (1) measure. Briefly discuss the measure. Discuss how each intervention can result in improved patient outcomes and cost savings for the practice. Provide evidence to support your discussion.
Discuss how each intervention can result in improved patient ratings (an NP’s patient scorecard). Provide evidence to support your discussion.
Use the provided APA Paper Template to complete the assignment.
Review writing for grammar and mechanics. Consider using academic writing resources to support writing. Your paper should include a title page, introduction with a purpose statement, body with citations to support assertions, conclusion addressing the findings of the paper, and reference page.
Review APA formatting. Consider using APA resources to support citation and reference formation.
Enjoy the learning and reach out to me if you have questions.
Week Three Faculty Assignment Orientation Presentation
Access the Webex Recording
Access the Webex Recording
Purpose
The purpose of this assignment is to have students research the measurement tools of NP performance. Through the use of quality patient outcomes, student will l ist and discuss three different patient interventions and how they would specifically measure the outcomes and h o w these primary care interventions result in improved patient outcomes and cost savings for the practice . In addition, students will discuss how these interventions result in improved patient ratings .
Activity Learning Outcomes
Through this assignment, the student will demonstrate the ability to:
Employ strategies to impact the development, implementation, and consequences of holistic healthcare policies using evidence-based practice principles (CO1)
Critically analyze how healthcare systems and APRN practice are organized and influenced by ethical, legal, economic and political factors (CO2)
Demonstrate professional and personal growth concerning the advocacy role of the advanced practice nursing in fostering policy within diverse healthcare settings (CO3)
Analyze social, historical, ethical and political contexts of healthcare policies and advanced practice leadership (CO4)
Advocate for institutional, local, national and international policies that fosters person-centered healthcare and nursing practice (CO5)
Due Date: Sunday of week 3 by 11:59 PM MST.
Students are expected to submit assignments by the time they are due. Assignments submitted after the due date and time will receive a deduction of 10% of the total points possible for that assignment for each day the assignment is late. Assignments will be accepted, with penalty as described, up to a maximum of three days late, after which point a zero will be recorded for the assignment. Quizzes and discussions are not considered assignments and are not part of the late assignment policy.
Total Points Possible: 200
Requirements:
The National Committee for Quality Assurance (NCQA) was formed to ensure quality of patient care and measurement of patient outcomes with set standards.
Healthcare Effectiveness Data and Information Set (HEDIS) is a performance measurement tool used by millions of health insurance plans. There are 6 domains of care:
Effectiveness of Care.
Access/Availability of Care.
Experience of Care.
Utilization and Risk Adjusted Utilization.
Health Plan Descriptive Information.
Measures Collected Using Electronic Clinical Data Systems
You may access the 6 domains of care by clicking this link:
(NCQA, n.d. https://www.ncqa.org/hedis/)
As an APN, productivity will be an important measurement for the practice to determine reimbursement and salary. Fee-for-service practices will require a set number of patients per day to maintain productivity. A capitated practice will require the APN to have a large panel of patients but also will focus on controlling costs. This can be accomplished through effective primary care that is accessible, convenient for the patients and has a method of measuring quality of care.
Write a formal paper in APA format with title page, introduction, the three required elements below, conclusion and reference page.
You are now employed as an NP in primary care. Choose one performance measure from one of the six domains of care, i.e. Adult BMI Assessment, Prenatal and Postpartum care, etc.
Develop three different patient interventions for that one performance measure and how you would specifically implement the intervention and measure the outcomes for that particular performance measure in clinical practice.
How would these primary care interventions result in improved patient outcomes and health care cost savings?
How can these interventions result in improved NP patient ratings?
Grading Rubric
Category
Points
%
Description
List and discuss three different patient interventions and how you would specifically measure the outcomes.
60
30%
From the National Committee for Quality Assurance (NCQA) website, discuss three patient interventions for the one performance measure.
Develop a measurement tool to track patient outcomes.
How would these primary care interventions result in improved patient outcomes and cost savings for the practice?
60
30%
Discuss how the interventions can result in improved patient outcomes and cost savings for the practice.
How can these interventions result in improved patient ratings?
60
30%
Discuss how these interventions can result in improved patient ratings (an NP’s patient scorecard).
180
90%
Total CONTENT Points= 180 pts
Category
Points
%
Description
Clarity of Writing
10
5%
Excellent use of standard English showing original thought. No spelling or grammar errors. Well organized with proper flow of meaning.
APA Format
10
5%
APA format, grammar, spelling, and/or punctuation are accurate.
20
10%
Total FORMAT Points= 20 pts
200
100%
ASSIGNMENT TOTAL= 200 points
NR 506 Week 3 Quality Healthcare: Measuring Nurse Practitioner Performance Sample Paper
Healthcare professionals play a significant role in improving patient and community health and well-being. However, healthcare professionals face multiple challenges, including increased demands for quality care, nursing staff shortages, a high prevalence of chronic conditions, and the need to integrate technology into clinical practice. These issues can affect care providers’ performance, prompting the need to measure nurse practitioners’ performance consistently.
According to Kahya & Oral (2018), assessing the performance of healthcare professionals is a profound strategy for guaranteeing high-quality care and achieving the desired medical outcomes. The National Committee for Quality Assurance (NCQA) provides a set of standards for improving care quality and measuring patient outcomes consistent with nursing interventions. Consequently, this paper discusses BMI (Body Mass Index) assessment as a performance measure and identifies strategies for improving patient outcomes, cost saving, and enhancing patient ratings.
Patient Interventions
Adult body mass index (BMI) assessment is a profound approach for enabling people to maintain healthy body weights and preventing multiple overweight-associated conditions. According to the National Committee for Quality Assurance [NCQA) (n.d), BMI remains the most useful population-level measure of obesity and overweight. When justifying the rationale for frequent adult BMI assessment, it is vital to consider obesity as a significant population health problem that results in detrimental consequences, including a high prevalence of chronic conditions like diabetes, cardiovascular diseases (CVDs), and premature deaths.
The National Committee for Quality Assurance (n.d) contends that obesity contributes to approximately one in five deaths in the United States. Other consequences associated with obesity and overweight include social stigma, psychological stress, compromised quality of life, and increased care costs (Gutin, 2017). As a result, weight-for-height screening (BMI assessment) enables healthcare professionals to estimate and identify the amount of body fat.
Equally, careful BMI monitoring helps healthcare professionals to identify at-risk populations and develop individualized interventions for preventing and treating obesity, including involving adults in regulated physical exercises, practicing diet control mechanisms, and educating them on self-care interventions. Arguably, it is possible to ensure appropriate BMI assessment and improvement of patient outcomes by obtaining, documenting, and frequently updating records regarding weight, height, and BMI for all outpatient adults, educating at-risk populations on interventions for managing healthy body weights, and developing follow-up plans to ensure long-term effects of the enacted strategies for preventing obesity and overweight.
Obtaining, Documenting, and Updating Records for Adults BMI
Healthcare professionals can adopt various ways of assessing adults’ BMIs and identifying at-risk individuals. According to Khanna et al. (2022), strategies for measuring and evaluating the body mass index include establishing the percentage of the body or visceral fat, measuring the waist circumference, and computing the waist-to-hip ratio. These criteria are fundamental in defining obesity and overweight. The World Health Organization [WHO] (2021) defines obesity as a body mass index (BMI) greater or equal to 30kg/m², while overweight represents a BMI greater or equal to 25kg/m². Based on the World Health Organization’s definitions of obesity and overweight, it is possible to detect the levels of risk and proximity to the risk factors for obesity and overweight.
After assessing adult BMI based on waist-to-hip ratios, waist circumference and computing the percentage of the body or visceral fat, healthcare professionals are responsible for keeping accurate documentation and frequently updating records to establish the effectiveness of interventions in preventing and treating overweight and obesity. Healthcare professionals should ensure accurate documentation of BMI by using electronic medical record systems (EMRS).
Verberne et al. (2018) contend that electronic health records (EHRs) contain complete and structured patient health status information documentation. Also, these technology-mediated modalities allow clinicians to accurately compute adult BMI by automating the process and leveraging data regarding patients’ heights and weights. Therefore, they enhance procedure accuracy and convenience. After applying these strategies to compute and assess adult BMI, it is possible to track and measure patient outcomes by creating spreadsheets and updating the team consistent with results from subsequent BMI assessments.
Educating At-risk People on Effective Strategy for Managing Weight
The second population-level intervention for improving BMI assessment and preventing obesity is educating at-risk people on appropriate strategies for managing weight and addressing risk factors for obesity and overweight. Hartmann-Boyce et al. (2018) contend that individual-level efforts for preventing and treating obesity are transferable to the broader population, providing opportunities for reducing the burden of obesity-related diseases, including cardiovascular conditions, some types of cancer, and diabetes. In the same vein, the World Health Organization [WHO] (2021) presents obesity as a multifactorial public health problem that prevails due to various risk factors, including an increased intake of unhealthy foods (high in fat and sugars), physical inactivity, and sedentary lifestyles. A lack of knowledge and awareness of self-management practices can increase an individual’s susceptibility to obesity and other associated problems.
Amidst the need to improve individual and population health literacy and awareness of preventive behaviors and activities, it is essential to tailor an educational program to enlighten people about self-management interventions. According to Hodgkinson et al. (2019), obesity awareness campaigns and educational programs focus on socio-behavioral factors that cause obesity. For instance, educating individuals and the community improves people’s knowledge of healthy diets and physical activity levels. It would be essential to assess the outcomes of this intervention by using Kirkpatrick’s evaluation model that evaluates educational programs based on participants’ training experience, learners’ learning outcomes, change in behavior and improvement, and the overall impacts of the educational program (Heydari et al., 2019). This approach can evaluate the program’s impact on staff satisfaction, behavior, and learning.
Developing Follow-up Plans
Although accurately recording BMI measurements and educating people about obesity and preventative measures can enhance interventions for preventing and treating obesity, these efforts are unsustainable if a proper follow-up plan is lacking. Welzel et al. (2018) argue that healthcare professionals should assist patients in continuous weight management. A comprehensive and well-timed follow-up can improve patient outcomes by fostering meaningful relationships with healthcare organizations, improving adherence to preventative and treatment options, and enhancing effective communication to support care coordination.
Improved Patient Outcomes
Implementing the identified population-level interventions aims to improve patient outcomes by reducing their susceptibility to obesity and overweight-associated conditions, such as cardiovascular diseases (CVDs) and diabetes. Also, early BMI assessment, community-based educational programs, and follow promote preventive behaviors by providing opportunities for early obesity detection, emphasizing preventative measures, and adherence to treatment interventions. According to Hodgkinson et al. (2019), educational interventions targeting at-risk populations can improve their health literacy, influence and promote preventive behaviors and activities, and enable people to sustain preventive and treatment strategies, including healthy diets and physical exercise. As a result, it is valid to associate the identified patient interventions with improved patient outcomes.
Cost Savings
Obesity and overweight inflict a massive cost burden on individuals, families, and healthcare systems. According to the Centers for Disease Control and Prevention [CDC] (2022), obesity costs the United States government approximately $173 billion annually. More essentially, a high prevalence of obesity-related diseases, including cardiovascular conditions, some types of cancer, and diabetes, exacerbate and increase care costs. As a result, implementing the identified measures can reduce care costs by promoting preventive behaviors and acts, providing early obesity screening and detection opportunities, and improving people’s health literacy.
Patient Ratings
Patient ratings are products of consumer experiences and satisfaction levels. Positive experiences and highly satisfactory healthcare services can improve care acceptability, appropriateness, and utilization. The proposed patient interventions for preventing and treating obesity are engaging and evidence-based. Hong et al. (2019) argue that obesity is a stigmatized condition that leads to weight-based discrimination. As a result, engaging patients and at-risk people in early BMI assessment, education programs, and follow-up plans can enhance their health, reduce susceptibility to obesity-related conditions, and curtail care costs. Participative and practical approaches can improve patient safety and contribute to care acceptance.
Conclusion
Healthcare professionals encounter various tools for measuring their performance amidst dynamics in healthcare. Consistent measuring nurse practitioner performance is a profound approach to improving health quality and patient outcomes. The National Committee for Quality Assurance (NCQA) provides a set of standards for improving care quality and measuring patient outcomes consistent with nursing interventions. For example, adult BMI assessment is the primary measure of obesity and overweight. This performance measure enables healthcare professionals to identify at-risk adults and develop/implement evidence-based, population-oriented services. This paper discusses BMI (Body Mass Index) assessment as a performance measure and identifies strategies for improving patient outcomes, cost-saving, and enhancing patient ratings.
References
Centers for Disease Control and Prevention. (2022, July 14). Why it matters. https://www.cdc.gov/obesity/about-obesity/why-it-matters.html#
Gutin, I. (2017). In BMI we trust: Reframing the body mass index as a measure of health. Social Theory & Health, 16(3), 256–271. https://doi.org/10.1057/s41285-017-0055-0
Hartmann-Boyce, J., Aveyard, P., Piernas, C., Koshiaris, C., Velardo, C., Salvi, D., & Jebb, S. A. (2018). Cognitive and behavioral strategies for weight management in overweight adults: Results from the Oxford food and activity behaviors (OxFAB) cohort study. PLOS ONE, 13(8), e0202072. https://doi.org/10.1371/journal.pone.0202072
Heydari, M. R., Taghva, F., Amini, M., & Delavari, S. (2019). Using Kirkpatrick’s model to measure the effect of new teaching and learning methods workshop for health care staff. BMC Research Notes, 12(1). https://doi.org/10.1186/s13104-019-4421-y
Hodgkinson, A., Abbott, J., Hurley, M. A., Lowe, N., & Qualter, P. (2019). An educational intervention to prevent overweight in pre-school years: A cluster randomized trial with a focus on disadvantaged families. BMC Public Health, 19(1). https://doi.org/10.1186/s12889-019-7595-2
Hong, Y.-R., Pavela, G., Lee, A. M., Williamson, V. G., & Cardel, M. I. (2019). Satisfaction with health care among individuals with overweight and obesity: A nationally representative cross-sectional study. Journal of General Internal Medicine, 34(8), 1397–1399. https://doi.org/10.1007/s11606-019-04939-2
Kahya, E., & Oral, N. (2018). Measurement of clinical nurse performance: Developing a tool including contextual items. Journal of Nursing Education and Practice, 8(6), 112. https://doi.org/10.5430/jnep.v8n6p112
Khanna, D., Peltzer, C., Kahar, P., & Parmar, M. S. (2022). Body mass index (BMI): A screening tool analysis. Cureus, 14(2). https://doi.org/10.7759/cureus.22119
National Committee for Quality Assurance. (n.d.). Adult BMI assessment. Retrieved November 11, 2022, from https://www.ncqa.org/hedis/measures/adult-bmi-assessment/
Verberne, L. D. M., Nielen, M. M. J., Leemrijse, C. J., Verheij, R. A., & Friele, R. D. (2018). Recording of weight in electronic health records: An observational study in general practice. BMC Family Practice, 19(1). https://doi.org/10.1186/s12875-018-0863-x
Welzel, F. D., Stein, J., Pabst, A., Luppa, M., Kersting, A., Blüher, M., Luck-Sikorski, C., König, H.-H., & Riedel-Heller, S. G. (2018). Five A’s counseling in weight management of obese patients in primary care: A cluster-randomized controlled trial (INTERACT). BMC Family Practice, 19(1). https://doi.org/10.1186/s12875-018-0785-7
World Health Organization. (2021, June 9). Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
NR506NP Healthcare Policy and Leadership Week 4 Discussion
This is a required, but not graded open forum. Your post should add further clarity to the assignment and content of the readings and lessons for the week. Please feel free to post questions related to content or assignments.
NR 506 Week 4 Presentation Assignment
This presentation needs speaker notes with the presentation, since I have to present the power point presentation. please add speakers notes.
Now on to week four. Start by viewing the Student Assignment Recording in the week 4 assignment area.
Research healthcare issues that have been identified in your local community. Develop a power point presentation with speaker notes. You will then use the power point during your Kaltura recording. Structure a health policy analysis presentation that addresses the following topics particular to your health problem.
Problem Statement
Background
Landscape
Options
Recommendations
Next, record your Kaltura presentation showing your power point and yourself speaking. Upload your Kaltura presentation into the week 4 assignment. How to use Kaltura resources are in Home/Resources/Technology Resources.
Posting your recording:
This week you will be producing a power point on a health policy analysis. From what you learned in week three about national data on healthcare issues, you will now examine one healthcare issue that is predominant in your local community. From your weekly readings (be sure to read chapter 14 from the Teitelbaum text in detail) you will:
Structure a health policy analysis presentation that addresses the following topics particular to your health problem. Develop a PowerPoint offline to address:
Problem Statement
Background
Landscape
Options
Recommendations
Important: This is not a patient treatment plan. This is a change in health policy to prevent secondary and tertiary effects from a health problem or unhealthy behavior.
Next, record your Kaltura presentation and upload it into the week 4 assignment. Recorded instructions on how to use Kaltura is imbedded under Resources on the left side, then Technology Resources.
Purpose
This assignment will focus on developing a health policy analysis presentation that includes a problem statement, background, landscape, options and recommendations from the week’s readings. The health policy analysis presentation is based upon an identified healthcare issue in one’s local community.
Activity Learning Outcomes
Through this assignment, the student will demonstrate the ability to:
Employ strategies to impact the development, implementation, and consequences of holistic healthcare policies using evidence-based practice principles (CO1)
Critically analyze how healthcare systems and APRN practice are organized and influenced by ethical, legal, economic and political factors (CO2)
Analyze social, historical, ethical and political contexts of healthcare policies and advanced practice leadership (CO4)
Advocate for institutional, local, national and international policies that fosters person-centered healthcare and nursing practice (CO5)
NR506NP Healthcare Policy and Leadership Week 5 Discussion
Ethical and Legal Implications
Purpose
Discuss potential complications in a clinical scenario at an out-patient family practice. Students will explore potential effects on patient outcomes and implications for members of the heath care team as a result of conflict among the healthcare team. Students will develop strategies that result in prevention of untoward outcomes that result in a positive practice culture.
Activity Learning Outcomes
Through this discussion, the student will demonstrate the ability to:
- Recognize potential areas of conflict in NP clinical practice (CO1)
- Determine methods of data collection to assess the conflict (CO3)
- Examine corporate compliance and its effect on clinical practice (CO2)
- Understand risk management in clinical practice (CO4)
Requirements:
You are a family nurse practitioner working in an outpatient primary care office of a large hospital system. The practice has been operating for over 15 years, and many of the administrative and clinical staff were hired when the practice opened.
You have been in the practice for less than 3 months. In that short amount of time, you have witnessed several of the clinical staff engaging in heated arguments with each other, sometimes in patient areas NR506NP Full Course Assignments.
You overhear an argument occurring today between two staff. You pick up a patient’s chart and notice a very low blood pressure that the medical assistant failed to notify you about. When you confront the MA, she states that she was going to report the vital signs to you when she became engaged in the heated argument you overheard and forgot to notify you.
Unfortunately, this pattern of behavior is not unusual in this practice. Working with staff who cannot cooperate effectively can negatively influence your ability to spend time with patients, can impede the flow of patients through the office, and could impact patient safety.
Case Study Responses:
Analyze the case study for potential issues for members of the healthcare team from office conflict. Contrast the potential effects for each member of the healthcare team based upon the required readings from the week. Discuss the potential ethical and legal implications for each of the following practice members:
- Medical assistant
- Nurse Practitioner
- Medical Director
- Practice
- What strategies would you implement to prevent further episodes of potentially dangerous patient outcomes?
- What leadership qualities would you apply to effect positive change in the practice? Focus on the culture of the practice.
NR506NP Healthcare Policy and Leadership Week 6 Discussion
Scope of Practice and Patient’s Healthcare Accessibility
Purpose
The purpose of this assignment is to identify the scope of practice in one’s state including level of independence of practice, prescribing authority, any limitations of practice, process for obtaining licensure in your state, certification and education requirements for licensure. Next, students will discuss how the level of independence of practice in their state, i.e., reduced, restricted or full practice, affects patient’s access to care in their local community.
Activity Learning Outcomes
Through this discussion, the student will demonstrate the ability to:
- Understand NP practice as defined by law (CO2)
- Determine legislation as defined by legislation, statutes and regulations (CO2)
- Identify barriers to ensuring patient’s rights (CO3)
NR506NP Full Course Assignments Requirements
Discuss your state NP community in terms of scope of practice. Include the your state’s scope of practice for NPs including:
- Level of independence of practice
- Prescribing authority
- Any limitations of practice
- Process for obtaining licensure in your state
- Certification and education requirements for licensure.
If you live in a restricted or reduced practice state, how has patient care been impacted in your local community from these barriers? For instance, is the ED used for primary care? Are the EDs overcrowded with long wait times? Are there urgent ca
READ MORE >>
NR506NP Week 5 Ethical and Legal Implications PapersThis is a graded discussion: ...
NR506NP Week 5 Ethical and Legal Implications Papers
This is a graded discussion: 100 points possible
Week 5:Ethical and Legal Implications (orig post due Wednesday, responses due Sunday)
Purpose
Discuss potential complications in a clinical scenario at an out-patient family practice. Students will explore potential effects on patient outcomes and implications for members of the heath care team as a result of conflict among the healthcare team. Students will develop strategies that result in prevention of untoward outcomes that result in a positive practice culture.
Activity Learning Outcomes
Through this discussion, the student will demonstrate the ability to:
- Recognize potential areas of conflict in NP clinical practice (CO1)
- Determine methods of data collection to assess the conflict (CO3)
- Examine corporate compliance and its effect on clinical practice (CO2)
- Understand risk management in clinical practice (CO4)
Due Date: Wednesday by 11:59PM MST of Week 5
Initial responses to the discussion topic must be posted by Wednesday 11:59pm MT. Two additional posts to peers and/or faculty are due by Sunday at 11:59pm MT. Students are expected to submit assignments by the time they are due.
A 10% late penalty will be imposed for discussions posted after the deadline on Wednesday of week 5, regardless of the number of days late. NOTHING will be accepted after 11:59pm MT on Sunday (i.e. student will receive an automatic 0).
Total Points Possible: 100
Requirements:
You are a family nurse practitioner working in an outpatient primary care office of a large hospital system. The practice has been operating for over 15 years, and many of the administrative and clinical staff were hired when the practice opened. You have been in the practice for less than 3 months. In that short amount of time, you have witnessed several of the clinical staff engaging in heated arguments with each other, sometimes in patient areas. You overhear an argument occurring today between two staff. You pick up a patient’s chart and notice a very low blood pressure that the medical assistant failed to notify you about. When you confront the MA, she states that she was going to report the vital signs to you when she became engaged in the heated argument you overheard and forgot to notify you.
Unfortunately, this pattern of behavior is not unusual in this practice. Working with staff who cannot cooperate effectively can negatively influence your ability to spend time with patients, can impede the flow of patients through the office, and could impact patient safety.
Case Study Responses:
- Analyze the case study for potential issues for members of the healthcare team from office conflict. Contrast the potential effects for each member of the healthcare team based upon the required readings from the week. Discuss the potential ethical and legal implications for each of the following practice members:
- Medical assistant
- Nurse Practitioner
- Medical Director
- Practice
- What strategies would you implement to prevent further episodes of potentially dangerous patient outcomes?
- What leadership qualities would you apply to effect positive change in the practice? Focus on the culture of the practice.
- A scholarly resource must be used for EACH discussion question each week.
Legal and Ethical Implications of Conflicts in Healthcare Sample Solution
Being a workplace like any other, conflicts in the healthcare setting are common. These conflicts have dire consequences on care quality both directly and indirectly. Team conflicts directly affect care quality by delaying care provision and failure to provide essential care to patients. Indirectly, team conflicts may demotivate healthcare professionals, thus making them exhibit a negative attitude towards patients and their families (Cullati et al., 2019). This discussion focuses on the legal and ethical implications of conflict to the care team, strategies to prevent conflicts that lead to undesirable patient outcomes, and the leadership qualities to effect positive change.
Conflicts have potential legal and ethical implications for each healthcare team member. To begin with, the nurse practitioner can be faced with ethical cases of negligence and work overload when tasks are not delegated. The medical director, who should be in charge of the team, may face legal implications when conflicts lead to negligence and the institution issued for it. On the other hand, the medical assistant can be met with legal implications of malpractice. For instance, in the case study, a patient with very low blood pressure had not been attended to. Practice can be faced with an ethical issue of inappropriate nurse-patient relationships, which would lead to loss of clientele due to arguing inpatient areas.
I would implement strategies to prevent further episodes of potentially dangerous patient outcomes: staff training, clearly outlining duty roasters, setting clear goals, and having conflict resolution guidelines. These would help prevent conflicts among the healthcare team members and inform them of the steps to take in case of a dispute arises.
The leadership qualities I would apply to effect positive change include change management. I would steer the team towards cultivating a conflict-free working environment. I would also ensure effective communication to avoid conflicts arising from a communication breakdown. Effective communication enhances interpersonal and professional relationships, preventing conflicts (Katz et al., 2020).
Conflicts in the healthcare setting should be avoided at all costs. They alter team dynamics and communication, decrease trust, and reduce team performance. As discussed above, conflicts also have legal and ethical implications for the team members. Team members should work together to minimize and manage conflicts.
References
Cullati, S., Bochatay, N., Maître, F., Laroche, T., Muller-Juge, V., Blondon, K. S., Junod Perron, N., Bajwa, N. M., Viet Vu, N., Kim, S., Savoldelli, G. L., Hudelson, P., Chopard, P., & Nendaz, M. R. (2019). When Team Conflicts Threaten Quality of Care: A Study of Health Care Professionals’ Experiences and Perceptions. Mayo Clinic proceedings. Innovations, quality & outcomes, 3(1), 43–51 https://doi.org/10.1016/j.mayocpiqo.2018.11.003
Katz, N. H., Lawyer, J. W., Sosa, K. J., Sweedler, M., & Tokar, P. (2020). Communication and Conflict Resolution Skills., 1-161. Retrieved from 30th May 2022 from https://nsuworks.nova.edu/shss_facbooks/177
NR506NP Week 6: Scope of Practice and Patient’s Healthcare Accessibility
No unread replies. No replies.
Purpose
The purpose of this assignment is to identify the scope of practice in one’s state including level of independence of practice, prescribing authority, any limitations of practice, process for obtaining licensure in your state, certification and education requirements for licensure. Next, students will discuss how the level of independence of practice in their state, i.e., reduced, restricted or full practice, affects patient’s access to care in their local community.
Activity Learning Outcomes
Through this discussion, the student will demonstrate the ability to:
- Understand NP practice as defined by law (CO2)
- Determine legislation as defined by legislation, statutes and regulations (CO2)
- Identify barriers to ensuring patient’s rights (CO3)
Due Date: Wednesday by 11:59pm MST of Week 6
Initial responses to the discussion topic must be posted by Wednesday 11:59pm MT. Two additional posts to peers and/or faculty are due by Sunday at 11:59pm MT. Students are expected to submit assignments by the time they are due.
A 10% late penalty will be imposed for discussions posted after the deadline on Wednesday of week 6, regardless of the number of days late. NOTHING will be accepted after 11:59pm MT on Sunday (i.e. student will receive an automatic 0).
Total Points Possible: 100
Requirements:
(State virginia)
- Discuss your state NP community in terms of scope of practice. Include the your state’s scope of practice for NPs including:
- Level of independence of practice **In California, NPs are required to practice under Standardized Procedure Guidelines. If CA is your intended practice state, please provide details on how Standardized Procedures Guidelines are developed in California and an example of a California SPG.
- Prescribing authority
- Any limitations of practice
- Process for obtaining licensure in your state
- Certification and education requirements for licensure.
- If you live in a restricted or reduced practice state, how has patient care been impacted in your local community from these barriers? For instance, is the ED used for primary care? Are the EDs overcrowded with long wait times? Are there urgent care clinics readily available? Is there adequate access to primary care? If you live in a full practice, how has independent practice of the APN resulted in improved patient access to healthcare?
- How does access to NPs impacts any healthcare disparities?
- A scholarly resource must be used for EACH discussion question each week.
NR506NP Week 7: APNs as Healthcare Policy Leaders
No unread replies. No replies.
Purpose
The purpose of this assignment is to discuss healthcare policy of the APN profession and how Transformational Leadership can help to influence policy changes. This week’s assignment focuses on the APN as a Health Policy Leader, one of the nine NONPF NP competencies. Students will analyze how health policy may affect NP practice and how Transformational Leadership can help to influence policy changes.
Activity Learning Outcomes
Through this discussion, the student will demonstrate the ability to:
- Critically analyze how healthcare systems and APRN practice are organized and influenced by ethical, legal, economic and political factors (CO2)
- Demonstrate professional and personal growth concerning the advocacy role of the advanced practice nursing in fostering policy within diverse healthcare settings (CO3)
- Advocate for institutional, local, national and international policies that fosters person-centered healthcare and nursing practice (CO4)
Due Date: Wednesday of week 7 by 11:59PM MST
Initial responses to the discussion topic must be posted by Wednesday 11:59pm MT. Two additional posts to peers and/or faculty are due by Sunday at 11:59pm MT. Students are expected to submit assignments by the time they are due.
A 10% late penalty will be imposed for discussions posted after the deadline on Wednesday of week 7, regardless of the number of days late. NOTHING will be accepted after 11:59pm MT on Sunday (i.e. student will receive an automatic 0).
Total Points Possible: 100
Requirements:
Criteria for Content
- Explanation of how healthcare policy can impact the advanced practice nurse profession
- Explanation of why advocacy is considered an essential component of the advance practice nurse’s role
- Discuss the four pillars of Transformational leadership and the effect it may have on influencing policy change
- A scholarly resource must be used for EACH discussion question each week.
APNs as Healthcare Policy Leaders Example Solution
Universal and state healthcare policies enormously impact the advanced practice nurses (APN) profession. These policies may enhance or limit their practice. However, advanced practice nurses can play a role in changing unfavorable policies. This discussion focuses on the impact of healthcare policy on the advanced practice nurse profession, the concept of advocacy in nursing and its effect on patient care, and transformational leadership and policy change.
Healthcare policy considerably impacts the advanced practice nurses’ profession on state, regional and national levels. Due to their scope of practice, advanced nurses should ideally bring healthcare services closer to the populations. However, healthcare policies in some states limit this by having restrictions on the practice of APNs. Advanced practice nurses can carry out comprehensive nursing interventions, thus helping a state achieve universal health coverage (Sevilla et al., 2022). Healthcare policies that allow APNs to run their healthcare institutions encourage APN professionals to fully use their knowledge and education in practice. Favorable healthcare policies can promote the growth of the advanced nurse practice profession. Healthcare professionals should advocate for healthcare policies that favor the practice of advanced practice nurses.
Advocacy in nursing has been defined as the act of nurses expressing patients’ needs and preferences to the hospital staff on their behalf (Kalaitzidis &Jewell, 2020). Advocacy is one of the roles that advanced practice nurses must play. Advocacy is considered an advanced practice nurse’s role since nurses are the ones who interact with the patients most compared to other healthcare providers’ team members. Therefore, they are best suited to know the patients’ preferences and needs. They are also best suited to link the hospital staff and the patients due to the strong nurse-patient relationships created when giving care to the patients. The nurse is the patient’s voice; thus, it is an obligation to advocate for their needs to other stakeholders in the healthcare department. Advocacy in nursing has had a significant positive impact on patient care. It has influenced service delivery and the overall quality of care in healthcare institutions, leading to better patient outcomes and patient satisfaction. Advocacy can also influence change of policies in healthcare, thus better care delivery.
Transformational leadership in nursing is a management concept that entails the motivation of nurses to have ownership of their roles and perform them beyond the minimum expectations. Transformational leadership enhances better demonstration of moral values and integrity in practice by cultivating teamwork among care providers. Transformational leaders focus on stimulating and inspiring followers by developing good relationships and enhancing change by emphasizing values (Giddens, 2018). The four pillars of transformational leadership are individualized consideration, idealized influence, intellectual stimulation, and inspirational motivation. These four-pillar pillars are integral for policy change.
Change of policy requires first understanding individual stakeholders of the policy, especially the policymakers and influencers, as well as the people affected by the policy and how the policy affects them. Policy change is hen followed by a planned strategy of how to influence the policymakers to change it. It also requires carefully devised logical and intellectual evidence of why the policy should be changed. In addition, the pillar of inspirational motivation would impact policy change by showing the policy makers how the change of policy would positively impact the people affected.
Advanced practice nurses can use advocacy to improve patient care and satisfaction in their institutions. They should also be on the frontline in applying transformational leadership to influence the change of policies that influence them, thus improving care delivery in their institutions and the entire healthcare field.
References
Giddens, J. (2018). Transformational leadership: What every nursing dean should know. Journal of Professional Nursing, 34(2), 117-121. https://doi.org/10.1016/j.profnurs.2017.10.004
Kalaitzidis, E., & Jewell, P. (2020). The concept of advocacy in nursing: a critical analysis. The Health Care Manager, 39(2), 77-84. https://doi:10.1097/HCM.0000000000000292
Sevilla Guerra, S., Zabalegui, A., Comellas Oliva, M., Estrem Cuesta, M., Martín?Baranera, M., & Ferrus Estopa, L. (2022). Advanced practice nurses: Analysis of their role from a multicentre cross?sectional study. International Nursing Review, 69(1), 30-37. https://doi.org/10.1111/inr.12706
NR506NP Week 8: Week 8: Reflection on Achievement of Outcomes
No unread replies. No replies.
Purpose
The final week will focus on Global Policy Reform and the impact on patient care. Students read the Berwick article and respond to the required discussions. In addition, students reflect on what they have learned in NR506NP and how it is applicable to their upcoming clinical courses.
Activity Learning Outcomes
Through this discussion, the student will demonstrate the ability to:
- Understand the role of advanced practice nursing in the International Context (CO2)
- Research global aspects of healthcare and the effect on the US healthcare system (CO5)
- Discuss the implications of global health on your clinical practice (CO5)
Due Date: Wednesday by 11:59pm MT of week 8
Initial responses to the discussion topic must be posted by Wednesday 11:59pm MT. Two additional posts to peers and/or faculty are due by Sunday at 11:59pm MT. Students are expected to submit assignments by the time they are due.
A 10% late penalty will be imposed for discussions posted after the deadline on Wednesday of week 8 by 11:59PM MST, regardless of the number of days late. NOTHING will be accepted after 11:59pm MT on Saturday (i.e. student will receive an automatic 0). Week 8 discussion closes on Saturday at 11:59pm MT.
Total Points Possible: 100
Requirements:
Berwick, D., Snair, M., & Nishtar, S. (2018). Crossing the global health care quality chasm: A key component of universal health coverage. Journal of American Medical Association, 320(13), 1317-1318.
Read the Berwick article and reflect on the concepts and practices you have learned in NR506 on healthcare systems, politics, and health policy. Reflections should include:
- How to make informed decisions on nursing practice and patient outcomes on a global basis.? In addition, state how you will apply what you have learned in this course to your upcoming practicum experience.?
- Describe how one will apply content from NR506NP to the upcoming clinical courses.
READ MORE >>
NR602 Primary Care of the Childbearing and Childrearing Family PapersNR602 Prima ...
NR602 Primary Care of the Childbearing and Childrearing Family Papers
NR602 Primary Care of the Childbearing and Childrearing Family Papers
Course Information
Course Number:NR602Course Title:Primary Care of the Childbearing and Childrearing FamilyCourse Credits:3 Credits (Theory .4, Clinical 2.6) 6/0/125/3Course Prerequisites:Students enrolled prior to May 2019: NR-500, NR-501, NR-503, NR-505, NR-506, NR-507, NR-508, NR-509, NR-510, NR-511, NR-512, NR-601; Effective May 2019: NR-500NP, NR-501NP, NR-503, NR-505NP, NR-506NP, NR-507, NR-509, NR-511, NR-565, NR-566, NR-599, NR-601 NR602 Primary Care of the Childbearing and Childrearing Family PapersCourse Description
With a focus on the healthcare requirements of women and families throughout the reproductive and parenting years, this course continues to broaden the understanding of health assessment concepts particular to the job of the FNP. NR602 Primary Care of the Childbearing and Childrearing Family Papers
Students will improve their knowledge of health promotion, sickness prevention, diagnosis, and management of common health issues. Through a clinical practicum experience in a primary care environment under the supervision of a preceptor, care tactics such as patient education, protocol formulation, follow-up, and referral will be used. NR602 Primary Care of the Childbearing and Childrearing Family Papers
ORDER COMPREHESIVE SOLUTION PAPERS
Textbooks and Resources
Required Textbooks
The following books are required for this course:

American Psychological Association. (2020).?Publication manual of the American Psychological Association?(7th ed.).?American Psychological Association. https://doi.org/10.1037/0000165-000

Lee, D., Starr, N.B., Brady, M. A., Gaylord, N. M., Driessnack, M., & Duderstadt, K. (2020). Burns’ Pediatric Primary Care (7th ed.). Elsevier.
This textbook is available as an e-book and can be accessed from the module view. NR602 Primary Care of the Childbearing and Childrearing Family Papers

Schuiling, K. D., & Likis, F. E. (2017). Women’s gynecologic health (3rd ed.). Jones and Bartlett Publishers. NR602 Primary Care of the Childbearing and Childrearing Family Papers
If your course has an E-Book, make sure to review this information.
Chamberlain Policies
Please review the NP Chamberlain Policies, along with the Chamberlain College of Nursing College Catalog or the Chamberlain College of Nursing Student Handbook for detailed information about Chamberlain policies.
Program Outcomes – NR602 Primary Care of the Childbearing and Childrearing Family Papers
Program Outcomes of Chamberlain nursing programs can be found in the Program Descriptions section of your College Catalog. You can access your College Catalog at http://www.chamberlain.edu/catalog
The MSN program outcomes are aligned with the American Association of Colleges of Nursing publication, The Essentials of Master’s Education in Nursing (2011). Upon completion of the MSN degree program, the graduate will be able to:
1
Provide high quality, safe, patient-centered care grounded in holistic health principles. (Holistic Health & Patient-Centered Care)
2
Create a caring environment for achieving quality health outcomes. (Care-Focused) NR602 Primary Care of the Childbearing and Childrearing Family Papers
3
Engage in lifelong personal and professional growth through reflective practice and appreciation of cultural diversity. (Cultural Humility) NR602 Primary Care of the Childbearing and Childrearing Family Papers
4
Integrate professional values through scholarship and service in health care. (Professional Identity)
5
Advocates for positive health outcomes through compassionate, evidence-based, collaborative advanced nursing practice. (Extraordinary Nursing) NR602 Primary Care of the Childbearing and Childrearing Family Papers
Course Outcomes – NR602 Primary Care of the Childbearing and Childrearing Family Papers
Chamberlain College of Nursing courses are built to align course content with specific Course Outcomes (COs). The COs define the learning objectives that the student will be required to comprehend and demonstrate by course completion. NR602 Primary Care of the Childbearing and Childrearing Family Papers
The COs that will be covered in detail each week can be found in the Overview page in that particular week. Whenever possible, a reference will be made from a particular assignment or discussion back to the CO that it emphasizes.
Upon completion of this course, the student will be able to do the following.
1
Integrate current evidence based clinical practice guidelines in the care of childbearing and childrearing families (PO 5). 1, 2, 3, 4, 5, 6, 7, 8
2
Appropriately apply anticipatory guidance and health promotion in the care of childbearing and childrearing families (PO 5). 1, 3, 4, 5, 6, 7, 8
3
Assess growth and developmental milestones in the care of childbearing and childrearing families (PO 5). 1, 3, 4
4
Construct an evidence based reproductive health management plan (PO 5). 1, 2
5
Identify and address healthcare needs of marginalized childbearing and childrearing families (PO 5) 8
Student Attestation
Students are required to complete the Student Attestation for each course you are enrolled. The Attestation will appear in the course, at the top of the Modules page. We ask that you complete the following steps:
- Review the Student Handbook
- Review the five statements in the item of the Attestation
- Next, mark “I accept”
- Then submit the Attestation.
You are required to complete the Student Attestation.
Assignment Summary
Due DateDetails
Sun Nov 1, 2020Assignment Week 1: Activity: iHuman Case 1due by 11:59pmAssignment Week 1: Clinical Site Discussiondue by 11:59pmAssignment Week 1: Homework- MyEvaluations Logdue by 11:59pmAssignment Week 1: Introductionsdue by 11:59pmAssignment Week 1: Readingsdue by 11:59pmAssignment Week 1: Submission: iHuman Case 1due by 11:59pmSun Nov 8, 2020Assignment Week 2: Activity: iHuman Case 2due by 11:59pmAssignment Week 2: Homework- MyEvaluations Logdue by 11:59pmAssignment Week 2: Readingsdue by 11:59pmAssignment Week 2: Submission: iHuman Case 2due by 11:59pmSun Nov 15, 2020Assignment Week 3: CEAP-NP Surveydue by 11:59pmAssignment Week 3: Homework- MyEvaluations Logdue by 11:59pmAssignment Week 3: Homework- Website Explorationdue by 11:59pmAssignment Week 3: Immunization Case Study Assignmentdue by 11:59pmAssignment Week 3: Readingsdue by 11:59pmSun Nov 22, 2020Assignment Week 4: Midterm Exam – Requires Respondus LockDown Browser + Webcamdue by 11:59pmAssignment Week 4: Clinical Vise Assignmentdue by 11:59pmAssignment Week 4: Homework- MyEvaluations Logdue by 11:59pmAssignment Week 4: Homework- Website Explorationdue by 11:59pmAssignment Week 4: Pediatric Clinical Pearl Case Study Assignmentdue by 11:59pmAssignment Week 4: Readingdue by 11:59pmSun Nov 29, 2020Assignment Week 5: Activity: iHuman Case 3due by 11:59pmAssignment Week 5: Homework- MyEvaluations Logdue by 11:59pmAssignment Week 5: Homework-Website Explorationdue by 11:59pmAssignment Week 5: Readingdue by 11:59pmAssignment Week 5: Submission: iHuman Case 3due by 11:59pmSun Dec 6, 2020Assignment Week 6: Activity: iHuman Case 4due by 11:59pmAssignment Week 6: Homework- MyEvaluations Logdue by 11:59pmAssignment Week 6: Homework- Website Explorationdue by 11:59pmAssignment Week 6: Readingdue by 11:59pmAssignment Week 6: Submission: iHuman Case 4due by 11:59pmSun Dec 13, 2020Assignment Week 7: Activity: iHuman Case 5due by 11:59pmAssignment Week 7: Homework- MyEvaluations Logdue by 11:59pmAssignment Week 7: Homework- Website Explorationdue by 11:59pmAssignment Week 7: Readingdue by 11:59pmAssignment Week 7: Submission: iHuman Case 5due by 11:59pmSat Dec 19, 2020Assignment Week 8: Final Exam – Requires Respondus LockDown Browser + Webcamdue by 11:59pmAssignment Week 8: Marginalized Women and Childbearing Familiesdue by 11:59pmAssignment End of Course Surveydue by 11:59pmAssignment Week 8: Homework- MyEvaluations Logdue by 11:59pmAssignment Week 8: Homework- Website Explorationdue by 11:59pmAssignment Week 8: Readingdue by 11:59pmAssignment Academic WriterAssignment Clinical Performance EvaluationAssignment iHuman Performance Overview Score Sheet – Practice CasesLate Assignment Policy
Students are expected to submit assignments by the time they are due. Assignments submitted after the due date and time will receive a deduction of 10% of the total points possible for that assignment for each day the assignment is late. Assignments will be accepted, with penalty as described, up to a maximum of three days late, after which point a zero will be recorded for the assignment.
In the event of an emergency that prevents timely submission of an assignment, students may petition their instructor for a waiver of the late submission grade reduction. The instructor will review the student’s rationale for the request and make a determination based on the merits of the student’s appeal.
Consideration of the student’s total course performance to date will be a contributing factor in the determination. Students should continue to attend class, actively participate, and complete other assignments while the appeal is pending. NR602 Primary Care of the Childbearing and Childrearing Family Papers
This Policy applies to assignments that contribute to the numerical calculation of the course letter grade.
Quizzes and discussions are not considered assignments and are not part of the late assignment policy. NR602 Primary Care of the Childbearing and Childrearing Family Papers
Late Discussion Policy
Please review the individual discussion board grading rubric for participation requirements within the course.
Evaluation Methods – NR602 Primary Care of the Childbearing and Childrearing Family Papers
The maximum score in this class is 1,000 points. The categories, which contribute to your final grade, are weighted as follows.
Graded ItemPointsWeightingDiscussion- Clinical Site Discussion (Weeks 1 – 50 points)
- Marginalized Women & Childbearing Families (Week 8 – 75 points)
- Breast Disorder (Week 1)
- STI/Cervicitis (Week 2)
- Asthma (Week 5)
- Bacterial Endocarditis (Week 6)
- Constipation/Encopresis (Week 7)
Clinical Practicum
The successful passage of clinical practicum for this course includes satisfactory completion of the specific list of requirements for this course and includes, but is not limited to the following:
- 125 accurately documented clinical hours that includes appropriate patient encounters by an approved preceptor at an approved site. Appropriate level of student independence for the clinical course. Abiding by all clinical policies found in compliance documents and the practicum handbook.
- Completion of a mid-term evaluation in the time-frame presented by both preceptor and faculty. A satisfactory final clinical evaluation by both preceptor and faculty. Mid-term contact with faculty by both student and preceptor reviewing student progress, goals, and any areas of need. Successful completion of any performance improvement plans (PIP) directly related to clinical if developed during the course of clinical for this course. Demonstration of meeting course objectives through clinical activities.
- Successful completion of clinical VISE (Virtual Interactive Student Evaluation) presentation to instructor between weeks 3-5.MyEvaluations Log & Passing Clinical
Clinical encounters must be posted within 7 days of the office visit. Failure to stay current may result in a “Not Met” on the mid-term and final evaluations.
Students must satisfactorily meet all the clinical requirements noted in the clinical grading rubric to pass clinical. NR602 Primary Care of the Childbearing and Childrearing Family Papers
All of your course requirements are graded using points. At the end of the course, the points are converted to a letter grade using the scale in the table below. Rounding may occur for final grade computation. A final grade of 80% (letter grade C) is required to pass the course. NR602 Primary Care of the Childbearing and Childrearing Family Papers
Letter GradePointsPercentageA 940–1,00094% to 100%A- 920–93992% to 93%B+890–91989% to 91%B 860–88986% to 88%B- 840–85984% to 85%C+820–83982% to 83%C 800–81980% to 81%F 799 and below79% and belowAttendance
Attendance is tracked through the Canvas Learning Management System. Students who do not participate in a course for seven (7) consecutive calendar days will be sent an impending attendance dismissal notice advising that he or she must attend within the next seven (7) calendar days or will be withdrawn from the course. NR602 Primary Care of the Childbearing and Childrearing Family Papers
Participation is defined as submitting a class assignment, participating in discussions, or completing quizzes and exams. For more information on the attendance policy and how violations of the policy may result in an administrative withdrawal, please see the Attendance and Administrative Withdrawal and Appeal sections of the Academic Catalog.NR602 Primary Care of the Childbearing and Childrearing Family Papers NR602 Primary Care of the Childbearing and Childrearing Family Papers
Clinical Practicum
The successful passage of clinical practicum for this course includes satisfactory completion of the specific list of requirements for this course and includes, but is not limited to the following:
- 125 accurately documented clinical hours that includes appropriate patient encounters by an approved preceptor at an approved site. Appropriate level of student independence for the clinical course. Abiding by all clinical policies found in compliance documents and the practicum handbook. NR602 Primary Care of the Childbearing and Childrearing Family Papers
- Completion of a mid-term evaluation in the time-frame presented by both preceptor and faculty. A satisfactory final clinical evaluation by both preceptor and faculty. Mid-term contact with faculty by both student and preceptor reviewing student progress, goals, and any areas of need. Successful completion of any performance improvement plans (PIP) directly related to clinical if developed during the course of clinical for this course. Demonstration of meeting course objectives through clinical activities. NR602 Primary Care of the Childbearing and Childrearing Family Papers
- Successful completion of clinical VISE (Virtual Interactive Student Evaluation) presentation to instructor between weeks 3-5.
Disability Accommodations in Academic Programs
OFFICE OF DISABILITY SERVICES
Chamberlain University is committed to providing reasonable accommodations for eligible students with documented disabilities as defined by state and federal laws relating to the Americans with Disabilities Act (ADA). Our intent is to ensure that every student who makes a request for accommodations under ADA is advised of the accommodation process as promptly as possible. NR602 Primary Care of the Childbearing and Childrearing Family Papers
If you are a student with a verifiable documented disability, and you can provide medical documentation regarding this disability, please contact the Office of Student Disability Services at adaofficer@chamberlain.edu or 855-229-0848 for more information on how to receive ADA. You may also fax your request to 630.596.1651.
Web Resources Disclaimer
The purpose of the Webliography is to provide students with annotated bibliographies of world wide websites relevant to their courses. These websites are not meant to be all inclusive of what is available for each course’s subjects and have not been sanctioned as academically rigorous or scholarly by Chamberlain College of Nursing. Please exercise caution when using these websites for course assignments and references. NR602 Primary Care of the Childbearing and Childrearing Family Papers
Also Read:
NR602 Week 3: CEAP-NP Survey Paper
NR602 Week 5 Evaluation of Marginalized Women Paper
NR602 Week 7: Submission: iHuman Case 5
NR602 Week 6: Activity: iHuman Case 4 Assignment
READ MORE >>
NR 602 Week 1 Activity iHuman Case 1 AssignmentNR 602 Week 1 Activity iHuman Cas ...
NR 602 Week 1 Activity iHuman Case 1 Assignment
NR 602 Week 1 Activity iHuman Case 1 Assignment
Purpose
The iHuman assignments provide students with an opportunity to experience clinical scenarios that are relevant to the lesson content through virtual patient encounters. iHuman is a highly interactive and a dynamic way to enhance your learning.
ORDER COMPREHSIVE SOLUTION PAPERS ON NR602 Week 1: Activity: iHuman Case 1 Assignment
NR 602 Week 1 Activity iHuman Case 1 Assignment Activity Learning Outcomes
Through this assignment, the student will demonstrate the ability to:
- Utilize interactive simulation technology to reinforce assessment and diagnostic reasoning skills in the care of a woman or pediatric patient (CO4) NR 602 Week 1 Activity iHuman Case 1 Assignment.

NR 602 Week 1 Activity iHuman Case 1 Assignment Due Date
Students need to complete the first attempt of the assigned iHuman case by Wednesday 11:59pm MT. Faculty will provide feedback to the student by Friday of the same week NR 602 Week 1 Activity iHuman Case 1 Assignment. The student has the option of 1 additional attempt to improve their score by Sunday 11:59pm MT at the end of week 1. There will only be a total of 2 attempts max per each iHuman assigned case.
Students are expected to submit assignments by the time they are due. Assignments submitted after the due date and time will receive a deduction of 10% of the total points possible for that assignment for each day the assignment is late NR 602 Week 1 Activity iHuman Case 1 Assignment. Assignments will be accepted, with penalty as described, up to a maximum of three days late, after which point a zero will be recorded for the assignment.
In the event of an emergency that prevents timely submission of an assignment, students may petition their instructor for a waiver of the late submission grade reduction. The instructor will review the student’s rationale for the request and make a determination based on the merits of the student’s appeal NR 602 Week 1 Activity iHuman Case 1 Assignment. Consideration of the student’s total course performance to date will be a contributing factor in the determination. Students should continue to attend class, actively participate, and complete other assignments while the appeal is pending.
Total Points Possible: 75 Points
NR 602 Week 1 Activity iHuman Case 1 Assignment Requirements
- Complete the week 1 module content prior to starting the iHuman assignment.
- Access iHuman by clicking the link provided below. Clicking the blue bar will launch the activity in a new browser window.
- Complete the case titled Case 1.
- This week, a 42-year old female presents to the clinic after discovering 2 lumps in her breast. This case does not pose a challenging diagnostic dilemma; it is meant to highlight indications for breast-cancer screening, and to outline the standard evaluation of a female who presents with a breast mass.
- Once you complete the case, click “Submit.”
- You will submit your iHuman Case study completion score sheet to the corresponding iHuman submission assignment.
In NR602, iHuman assignments will be assessed on the following areas: History Taking, Physical Exam, Differential Diagnoses, Rank diagnoses, MNM (must not miss) Diagnoses, Order tests, Final Diagnosis, Management Plan. A score of 80% or better is your target with this assignment NR 602 Week 1 Activity iHuman Case 1 Assignment. You will have (2) two attempts; the highest score of two attempts will be taken as the final grade.
READ MORE >>
