Our Previous Samples
Neurodevelopment Disorders Study Guide NRNP6665Neurodevelopment Disorders Study ...
Neurodevelopment Disorders Study Guide NRNP6665
Neurodevelopment Disorders Study Guide NRNP6665 Week 8 Assignment
STUDY GUIDE FORUM

Abnormal brain development or damage at an early age can lead to neurodevelopmental disorders. Within this group of disorders, some are resolvable with appropriate and timely interventions, either pharmacological or nonpharmacological, while other disorders are chronic and need to be managed throughout the lifespan.
For this Assignment, you will develop a study guide for an assigned disorder and share it with your colleagues. In sum, these study guides will be a powerful tool in preparing for your certification exam.
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
WEEKLY LEARNING RESOURCES
Required Readings
- Hilt, R. J., & Nussbaum, A. M. (2016). DSM-5 pocket guide for child and adolescent mental healthLinks to an external site.. American Psychiatric Association Publishing.
- Chapter 12, “Developmental Milestones”Links to an external site.
- Thapar, A., Pine, D. S., Leckman, J. F., Scott, S., Snowling, M. J., & Taylor, E. A. (2015). Rutter’s child and adolescent psychiatry (6th ed.). Wiley Blackwell.
- Chapter 51, “Autism Spectrum Disorder”
- Chapter 55, “ADHD and Hyperkinetic Disorder”
- Utah State University. (n.d.). Creating study guidesLinks to an external site.. https://www.usu.edu/academic-support/test/creating_study_guidesLinks to an external site.
- Walden University. (2020). Success strategies: Self-paced interactive tutorialsLinks to an external site.. https://academicguides.waldenu.edu/academic-skills-center/skills/tutorials/success-strategiesLinks to an external site.
- Zakhari, R. (2020). The psychiatric-mental health nurse practitioner certification review manual. Springer.
- Chapter 13, “Child/Adolescent Neurodevelopmental Disorders”
Neurodevelopment Disorders Study Guide NRNP6665 Required Media
- Dillon, K. (2019, March 23). DSM-5 neurodevelopmental disordersLinks to an external site.. [Video]. YouTube. https://www.youtube.com/watch?v=Jx4GuyX5SgcLinks to an external site.
- The National Center for Learning Disabilities. (2013, February 20). What is ADHD?Links to an external site. [Video]. YouTube. https://youtu.be/0Wz7LdLFJVMLinks to an external site.
- Osmosis. (2017, October 17). Autism – causes, symptoms, diagnosis, treatment, pathologyLinks to an external site. [Video]. YouTube. https://youtu.be/x2hWVgZ8J4A
Medication Review
Irritability in autismAttention-deficit/hyperactivity disorderaripiprazolerisperidoneamphetamine IR, XR, and ER
dextroamphetamine
atomoxetineclonidine hydrocholoride ER
Dexmethylphenidate IR and XR
guanfacine hydrocholride ER
lisdexamfetamine
methylphenidate
methylphenidate hydrocholoride IR and ER, transdermal
TO PREPARE
- Your Instructor will assign you to a specific neurodevelopmental disorder from the DSM-5-TR.
- Research your assigned disorder using the Walden Library. Then, develop an organizational scheme for the important information about the disorder.
THE ASSIGNMENT
Create a study guide for your assigned disorder. Your study guide should be in the form of an outline with references, and you should incorporate visual elements such as concept maps, charts, diagrams, images, color coding, mnemonics, and/or flashcards. Be creative! It should not be in the format of an APA paper. Your guide should be informed by the DSM-5-TR but also supported by at least three other scholarly resources.
Areas of importance you should address, but are not limited to, are:
- Signs and symptoms according to the DSM-5-TR
- Differential diagnoses
- Incidence
- Development and course
- Prognosis
- Considerations related to culture, gender, age
- Pharmacological treatments, including any side effects
- Nonpharmacological treatments
- Diagnostics and labs
- Comorbidities
- Legal and ethical considerations
- Pertinent patient education considerations
BY DAY 7 OF WEEK 8
You will need to submit your Assignment to two places: the Week 8 Study Guide discussion forum as an attachment and the Week 8 Assignment submission link. Although no responses are required in the discussion forum, collegial discussion is welcome. You are encouraged to utilize your peers’ submitted guides on their assigned neurodevelopmental disorders for study.
Access the Study Guide Forum (or click the Next button).
Intellectual Disability Study Guide Example
How does DSM-5 define intellectual disability?
A deficit in intellectual and adaptive functioning of an individual (American Psychiatric Association, 2013)
What are the signs and symptoms of intellectual disability according to DSM-5?How common is intellectual disability?¾ Limitation in spoken language – vocabulary and grammar – conceptual domain¾ Limitation in conceptual skills such as understanding written language – social domain¾ Dependence for activities of daily living – dressing, bathing, cooking meals, elimination – practical domain
¾ Other criteria: symptoms begin during the period of development (American Psychiatric Association, 2013)
¾ Affects one percent of the population (American Psychiatric Association, 2013)¾ In the US, it affected about 3.5% (CDC, 2019)¾ More common among males than females, with 1.6/1 for mild to 1.2/1 for severe cases (American Psychiatric Association, 2013)
¾ About six in every thousand cases are severe
¾ Commonly diagnosed among older children (CDC, 2019)
¾ No significant racial predilection
What are the risk factors for intellectual disability?What is the Development and course of intellectual disability· Can be classified as genetic or physiological· Genetic factors – chromosomal disorders, inborn errors of metabolism, maternal disease· Physiological factors can be antenatal, natal, or postnatal
· Antenatal – toxins and alcohol
· Natal – traumatic labor, neonatal encephalopathy
· Postnatal – infections (meningitis), traumatic brain injury, child abuse, hypoxic-ischemic injury, toxic metabolic syndromes, seizure disorders, demyelinating disorders, and chronic social deprivations
· Deficient brain development leading to slow or absent neurodevelopment· Deficits in language and motor development are diagnosed first· The disease does not progress, but there is absent development of neurological and behavioral milestones
· Diagnosis can be made as early as 2 years of age (American Psychiatric Association, 2013)
· Lack of achievement of social and behavioral skills are seen
· Sometimes, the risks lead to the loss of achieved milestones
Diagnostics and labHow do I evaluate further the suspected cases?· Clinical and mental state examinations are required· Standardized intelligence tests are used to assess the intelligence quotient (IQ)· Chromosome analysis to screen chromosomal diseases
· Urine and blood analysis to screen comorbidities
· Metabolic screening
· Family pedigree – three generations· Evaluate associated medical illnesses – seizures, cerebral palsy· Cultural evaluation
· Assess the home environment
· Assess the availability of community reserves
What are the possible differential diagnoses for intellectual disability? SCAM -mnemonicWhat illnesses can cooccur with intellectual disability? AIDS CAB – mnemonic· Specific learning disorder· Communication disorder· Autism spectrum disorders
· Major and minor neurocognitive disorders – Alzheimer’s and Down’s syndromes (Lee et al., 2021)
· Attention deficit hyperactivity disorder· Impulse-control disorders· Depressive disorders and anxiety disorders
· Stereotypic movement disorder
· Cerebral palsy
· Autism spectrum disorders
· Bipolar disorders
What determines the outcome of the ID? – PrognosticatorsMedications used?· Timely intervention· Time at diagnosis· Comorbidities
· No approved medication for treatment· Aripiprazole and risperidone can be used to manage aggression (Lee et al., 2021)· A lifelong condition requiring early intervention
Nonpharmacological intervention usedWhat are the culture and gender-related considerations?· Behavioral interventions· Psychoeducation· Basic education
· Lie skills training
· Government resources
· Training on the transition to adulthood
· Screening for x-linked disorders as – common in males (American Psychiatric Association, 2013)· Understanding the cultural background of the patient regarding ID· Linguistic and ethnic background assessment
What are the legal and ethical related considerations?What should be considered during patient education?· Violence and aggression from the patient can lead to a legal arrest· Patients are more vulnerable to sexual abuse (Åker & Johnson, 2020)· Fair distribution of resources to patients
· Understanding the need to incorporate the patient’s cognitive level in decision-making.
· Hearing and visual difficulties· Language deficits· Involvement of family for maximal outcomes (Patel et al., 2020)
· Minimize restriction in learning
· Limited learning capacity
References
Åker, T. H., & Johnson, M. S. (2020). Sexual abuse and violence against people with intellectual disability and physical impairments: Characteristics of police-investigated cases in a Norwegian national sample. Journal of Applied Research in Intellectual Disabilities: JARID, 33(2), 139–145. https://doi.org/10.1111/jar.12656
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5 (R)) (5th ed.). American Psychiatric Association Publishing.
CDC. (2019, June 6). Products – data briefs – number 291 – November 2017. Cdc.Gov. https://www.cdc.gov/nchs/products/databriefs/db291.htm
Lee, K., Cascella, M., & Marwaha, R. (2021). Intellectual Disability. StatPearls Publishing.
Patel, D. R., Cabral, M. D., Ho, A., & Merrick, J. (2020). A clinical primer on intellectual disability. Translational Pediatrics, 9(Suppl 1), S23–S35. https://doi.org/10.21037/tp.2020.02.02
Neurodevelopment Disorders Study Guide NRNP6665 Rubric
NRNP_6665_Week8_Assignment_RubricNRNP_6665_Week8_Assignment_RubricCriteriaRatingsPtsThis criterion is linked to a Learning Outcome Create a study guide, in outline form with references, for your assigned disorder. Incorporate visual elements such as concept maps, charts, diagrams, images, color coding, mnemonics, and/or flashcards.
30 to >26.0 pts
ExcellentThe response is in a well-organized and detailed outline form. Informative and well-designed visual elements are incorporated…. Followed directions correctly by uploading assignment to Gradebook and submitted to the discussion forum area.26 to >23.0 pts
GoodThe response is in an organized and detailed outline form. Appropriate visual elements are incorporated…. Partially followed directions by uploading assignment to Gradebook but did not submit to the discussion forum area.23 to >20.0 pts
FairThe response is in outline form, with some inaccuracies or details missing. Visual elements are somewhat vague or inaccurate…. Partially followed directions by submitting to the discussion forum area but did not upload assignment to Gradebook.20 to >0 pts
PoorThe response is unorganized, not in outline form, or is missing. Visual elements are inaccurate or missing….Did not follow directions as did not submit to discussion forum area and did not upload assignment to gradebook per late policy.30 ptsThis criterion is linked to a Learning Outcome Content areas of importance you should address, but are not limited to, are:• Signs and symptoms according to the DSM-5-TR• Differential diagnoses• Incidence• Development and course• Prognosis• Considerations related to culture, gender, age• Pharmacological treatments, including any side effects• Nonpharmacological treatments• Diagnostics and labs• Comorbidities• Legal and ethical considerations• Pertinent patient education considerations
50 to >44.0 pts
ExcellentThe response thoroughly addresses all required content areas.44 to >39.0 pts
GoodThe response adequately addresses all required content areas. Minor details may be missing.39 to >34.0 pts
FairThe response addresses all required content areas, with some inaccuracies or vagueness. No more than one or two content areas are missing.34 to >0 pts
PoorThe response vaguely or inaccurately addresses the required content areas. Or, three or more content areas are missing.50 ptsThis criterion is linked to a Learning Outcome Support your guide with references to the DSM-5-TR and at least three evidence-based, peer-reviewed journal articles or evidenced-based guidelines. Be sure they are current (no more than 5 years old).
10 to >8.0 pts
ExcellentThe response is supported by the DSM-5 and at least three current, evidence-based resources from the literature.8 to >7.0 pts
GoodThe response provides at least three current, evidence-based resources from the literature that appropriately support the assessment and diagnosis of the patient in the assigned case study.7 to >6.0 pts
FairThree evidence-based resources are provided to support assessment and diagnosis of the patient in the assigned case study, but they may only provide vague or weak justification.6 to >0 pts
PoorTwo or fewer resources are provided to support assessment and diagnosis decisions. The resources may not be current or evidence based.10 ptsThis criterion is linked to a Learning Outcome Written Expression and Formatting – English Writing Standards: Correct grammar, mechanics, and proper punctuation
5 to >4.0 pts
ExcellentUses correct grammar, spelling, and punctuation with no errors4 to >3.5 pts
GoodContains one or two grammar, spelling, and punctuation errors3.5 to >3.0 pts
FairContains several (three or four) grammar, spelling, and punctuation errors3 to >0 pts
PoorContains many (five or more) grammar, spelling, and punctuation errors that interfere with the reader’s understanding5 ptsThis criterion is linked to a Learning Outcome Written Expression and Formatting – The guide follows correct APA format for parenthetical/ narrative in-text citations and reference list.
5 to >4.0 pts
ExcellentUses correct APA format with no errors4 to >3.5 pts
GoodContains one or two APA format errors3.5 to >3.0 pts
FairContains several (three or four) APA format errors3 to >0 pts
PoorContains many (five or more) APA format errors5 ptsTotal Points: 100Also Read: PATIENT EDUCATION FOR CHILDREN AND ADOLESCENTS NRNP 6665 WEEK 5READ MORE >>
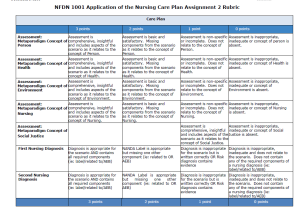
NorQuest College NFDN 1001 Application of the Nursing Process: Nursing Care Plan ...
NorQuest College NFDN 1001 Application of the Nursing Process: Nursing Care Plan 2 Example
Nursing Care Plan 2
NorQuest Care Plan Template FormName:
Chosen scenario (circle one): 2
Assessment· All components of the metaparadigm included.
· Literature support provided.
The nursing metaparadigm refers to a “theoretical definition for the substance and structure for determining the key bodies of knowledge needed to understand particular clinical situations” (Potter et al., 2019, p. 66). It provides opportunities for nurses to organize ideas, beliefs, and practices consistent with content and contexts.The four concepts of nursing metaparadigm are person/client, environment, healthcare, nursing care, and social justice (Deliktas et al., 2019). The person/client concept includes sub-themes such as individual interactions with the environment, social relationships, self-management competencies, individual needs, feelings, and situations.
· In Maria’s case study, it is possible to identify relevant personal information since it states that she is a 37-year-old single parent of two teenage boys
The health domain entails sub-themes such as physical, relational, psychological, and spiritual aspects regarding individuals, patients, and families. These aspects are dynamic, prompting healthcare professionals to help clients reach productive and satisfying outcomes (Potter et al., 2019).
Maria’s case study presents information that resonates with her health needs. The case states that she is on the verge of becoming type 2 diabetic because she embraces unhealthy diet habits. Also, she has gained 20 pounds over the last year because of the interplay between life stressors. Finally, she experiences loss of sleep due to life stress and worrying thoughts.
The environmental concept involves a person’s family and social ties, the community, health care systems, and geopolitical issues that affect health (Potter et al., 2019).
· Maria’s case study signifies a life without social or family ties because her two teenage boys do not live in Edmonton. Further, the case study does not describe the presence of social support systems.
The nursing concept includes understanding a person’s environment, life, and health goals (Potter et al., 2019). Also, it touches on attributes, humanism factors, and the aspect of touching people’s lives (Deliktas et al., 2019).
· Many considerations in Maria’s case study present a nursing concern. For instance, she is a borderline type 2 diabetic; she grapples with sleeping difficulties and worrying thoughts, she bears the stress of having two jobs and leads unhealthy life because of poor food choices. These factors can affect her quality of life and compromise her well-being.
First diagnosisStress overload is associated with resource constraints (financial and social), work-related burnout, and worrying thoughts that lead to sleeping difficulties. Also, the consideration of being a single parent of two teenage boys can lead to stress due to inadequate resources.Second diagnosisMaria can be overweight because of her unhealthy intake of fast foods, being a borderline type 2 diabetic, and gaining 20 pounds within a year.Priority Diagnosis Identified· Literature support provided.
Maria’s priority diagnosis is stress overload because she struggles with multiple stressors, including work-related struggles, the plausibility of lacking ideal support systems, and resources constraints. In this sense, it is essential to focus on addressing stressors as a strategy for improving Maria’s health.It is essential to understand the interplay between components of the nursing metaparadigm, including personal, environmental, nursing, and health aspects that compound Maria’s well-being. For example, multiple stressors contribute to Maria’s declining health, stress overload, and unhealthy diet plans result in her borderline type 2 diabetic status. Further, she is a single parent of two teenage boys and works 2 jobs to pay for the bills. These aspects require healthcare professionals to implement a contingency plan for healthcare delivery to capitalize on every aspect.
PlanningThe SMART goal for a contingency plan for providing care to Maria emphasizes the rationale of reducing stress overload by tracking progress and the causes of stress daily. Therefore, she will state the reduced prevalence of stress overload after interventions each day for 3 months of a contingency plan implementation.First Nursing Intervention· Literature support provided.
The priority for improving Maria’s health entails identifying the causative/precipitating factors for stress overload. Doenges et al. (2019) underscore the rationale of ascertaining what tragic/ difficult events have occurred, including family violence, death of loved one, chronic or terminal illness, and workplace stress when dealing with people with stress overload.Understanding the root causes of stress overload requires nurses to develop meaningful relationships with patients to motivate them to open up (Ackley et al., 2020). In turn, partnering with patients and developing meaningful relationships can facilitate developing SMART goals and evaluation plans for outcome measures of nurse-led and collaborative interventions.
Second Nursing Intervention
· Literature support provided.
The nurses will promote Maria’s wellness by using a locus of control to develop an individual plan of care to encourage her self-care strategies. Doenges et al. (2019) argue that incorporating strengths, assets, and past coping strategies that successfully address stress overload reinforces the client’s ability to deal with difficult situations.It is essential to implement evidence-based behavioral therapies and provide information about the stress and exhaustion phase, which occurs when a person is experiencing chronic or unresolved stress. According to Henry et al. (2021), it is possible to promote techniques for stress management such as encouraging healthy lifestyle behaviors, favoring relaxation, and incorporating strategies for improving cognitive and emotional functioning.
Third Nursing Intervention
· Literature support provided.
The nurse will assist maria in dealing with the current situation by actively listening to concerns, providing an empathetic presence, and providing for or encouraging a restful environment where possible (Doenges et al., 2019). The nurse needs to allow Maria to sort out things that she can control and determine responses for modifiable aspects. Also, the healthcare provider should reserve Maria’s autonomy to control care trajectories by avoiding judgemental thoughts and providing decisional support.Finally, it is vital to provide her with much sought-after social support necessary for addressing stress overload. As a single parent of two teenage boys, Maria grapples with multiple stressors, including resource constraints and work-related struggles. As a result, providing social support can enable her to strengthen self-care and stress management interventions.
EvaluationThe nurse will conduct a progress-oriented evaluation by following up on Maria every two weeks. Also, the caregiver will assist her in reviewing learning materials regarding stress management interventions. The testable outcome measures for the nursing plan include:
· Assessing whether Maria can verbalize or demonstrate reduced stress reactions.
· Evaluate if she can accurately assess the current situation
· Investigate whether she can identify ineffective stress management behaviors and consequences.
· Assess if Maria can implement strategies and insights acquired from collaborative efforts to manage stress.
Also Read:
NorQuest NFDN 1002 Professional Portfolio Assignment
Summary
Undoubtedly, Maria’s case study presents an ideal scenario where the components of the nursing metaparadigm interact to determine individual health and well-being. In this sense, healthcare professionals can utilize the interplay between person/client attributes, health, environment, and nursing sub-themes to develop an informed nursing care plan. A standard nursing process includes various stages, including assessment, diagnosis, planning, implementation, and evaluation (ADPIE). According to Semachew (2018), the nursing process is a systematic problem-solving approach that helps nurses identify, prevent, and treat actual and potential health problems to promote wellness.
The assessment phase of the nursing process entails accessing, consolidating, and collecting patient data regarding health conditions and nursing metaparadigm components. Often, nurses obtain patient information by reviewing health history and collaborating with patients to obtain identified data. This step allows nurses to identify issues, patient needs, priorities, and goals that form the basis of patients’ diagnoses.
Patient diagnosis is the second phase of the nursing process that involves identifying actual or potential problems manageable by nurse-led or collaborative interventions (Semachew, 2018). A nursing diagnosis is essential in providing the basis of nursing interventions and allowing caregivers and patients to collaborate in developing SMART goals. Notably, this stage resonates with the planning phase by providing relevant information regarding the client’s health status.
Thirdly, the planning phase is a prerequisite for implementing nurse-led or collaborative interventions to improve care and prevent health conditions. According to Potter et al. (2019), care planning is a nursing behavior category that includes setting client-centered goals, outlining outcomes measures, developing plans for nursing interventions, and prioritizing approaches for resolving patient problems. The SMART approach enables nurses to create specific, measurable, attainable, reliable, and time goals consistent with clients’ needs and goals.
Fourthly, the implementation phase entails actualizing the nursing plan by enacting nurse-initiated, physician-led, and collaborative interventions (Semachew, 2018). At this point, it is essential to incorporate social justice by reserving the client’s right to participate in care delivery and consensus decision-making. According to Habibzadeh et al. (2021), social justice entails providing equal health for all clients, regardless of their characteristics. As a result, nurses should emphasize fairness and justice when implementing interventions for improving clients’ health and well-being.
Finally, the evaluation phase entails assessing the overall outcome measures of health interventions. According to Potter et al. (2019), evaluation processes reveal the successes and failures of care interventions by examining the condition/situation and assessing changes after implementing interventions. If care approaches fail to achieve the SMART goals, the nurse may update the initial plan by identifying areas of improvement. Undoubtedly, the evaluation phase is a profound stage for ensuring the successful implementation of quality improvement initiatives.
References
Ackley, B. J., et al. (2020) Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care (12th ed.). F.A. Davis
Deliktas, A., Korukcu, O., Aydin, R., & Kabukcuoglu, K. (2019). Nursing students’ perceptions of nursing metaparadigms: A phenomenological study. Journal of Nursing Research, 27(5). https://doi.org/10.1097/jnr.0000000000000311
Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2019). Nurse’s pocket guide: diagnoses, prioritized interventions, and rationales (15th ed). F.A. Davis Company
Habibzadeh, H., Jasemi, M., & Hosseinzadegan, F. (2021). Social Justice in the health system; a neglected component of Academic Nursing Education: A qualitative study. BMC Nursing, 20(1). https://doi.org/10.1186/s12912-021-00534-1
Henry, K. A., Neeser, K. J., & Muss, C. (2021). A short-term intervention to reduce stress levels in the workplace for office workers at UEFA—the Union of European Football Associations in Nyon/Switzerland. Open Journal of Preventive Medicine, 11(05), 211–228. https://doi.org/10.4236/ojpm.2021.115017
Potter, P. A., Perry, A. G., Stockert, P. A., & Hall, A. M. (2019). Canadian Fundamentals of Nursing (6th ed). Elsevier.
Semachew, A. (2018). Implementation of the nursing process in clinical settings: The case of three governmental hospitals in Ethiopia, 2017. BMC Research Notes, 11(1). https://doi.org/10.1186/s13104-018-3275-z
Application of the Nursing Process: Nursing Care Plan 2 Instructions
Purpose
This assignment is an opportunity to apply the nursing process to a client by developing a nursing care plan that meets the specific priority needs of the client in the scenario you choose.
You will be assessed on how you apply your understanding of the following general learning outcomes:
â— Explain how the nursing metaparadigm, theories, principles, and concepts from nursing and other professional disciplines contribute to holistic nursing practice
â— Examine the nursing process as a critical-thinking method of organizing and delivering nursing care.
NFDN 1001 Application of the Nursing Process: Nursing Care Plan 2 Instructions
Please read through all of the instructions in the documents below and review the rubric before you begin this assignment.
Complete all parts of the assignment.
You must utilize the template provided for this assignment.
Plagiarism and Academic Misconduct
Correct citation and reference formatting is an expectation for all written assignments at NorQuest College. Unfortunately, the correct use of APA is a struggle for many students, which can lead to plagiarism. Plagiarism is considered a serious offence at NorQuest College and will result in an Academic Misconduct and a reduction in assignment marks. Click here to access the NorQuest Library’s resources to learn how to prevent plagiarism. If you have not done so already, we strongly recommend clicking here to start the Online APA modules.
NFDN_1001_Nursing_Care_Plan_Assignment___2_Template
NFDN_1001_Nursing_Care_Plan_Rubric_Assignment_2_-_2021_(002).pdf
NFDN_1001_Nursing_Care_plan_Assignment__2_Instructions_(002).pdf
READ MORE >>
Neurotransmitters and Receptor Theory Sample PaperTransmission of electrical imp ...
Neurotransmitters and Receptor Theory Sample Paper
Transmission of electrical impulses from one neuron across the synapse to a different neuron or a cell is facilitated by neurotransmitters. Examples of neurotransmitters that facilitate central nervous functions include amino acids (GABA, aspartate, and glutamate), amines (catecholamines, acetylcholine, and serotonin), peptides (neuropeptide Y) and gases such as nitric oxide (Sheffler, Reddy & Pillarisetty, 2020). These neurotransmitters have specific receptors which bind to psychopharmacologic agents to either cause agonistic or antagonistic actions as illustrated hereafter.
Agonist-to-antagonist Spectrum of Action of Psychopharmacologic Agents
Psychopharmacologic agents are drugs used in the management of a wide spectrum of psychiatric disorders including behavioral disorders, depression, anxiety or stressor-related conditions. The drugs can either exhibit agonistic or antagonistic activities at the receptor site (Katzung, 2018). While agonists activate the receptors, antagonists block the receptors. For example, in the etiology of Schizophrenia, the Dopamine hypothesis is widely accepted. It is believed that excess Dopamine neurotransmission causes the Schizophrenic symptoms.
This has been evidenced by the presence of higher levels of Dopamine receptors in Schizophrenic patients. Management of Schizophrenia therefore utilizes drugs that block the Dopamine receptors (antagonists) for example Chlorpromazine (Katzung, 2018). Contrarily, the pathophysiology of neurodegenerative diseases such as Parkinson disease (PD) reveals decreased dopamine levels and receptor (Katzung, 2018). Therefore, dopamine agonists such as Levodopa are used in the management of PD.
Partial agonists bind and activate receptors but only have partial efficacy (Berg & Clarke, 2018). An example, used as an anxiolytic is Buspirone. Partial agonists exhibit both agonistic and antagonistic actions for example, while Buspirone is a partial agonist for 5HTA1 receptors; it’s an antagonist for D2 receptors (Katzung, 2018)). Therefore, it can be used both as an anxiolytic and antidepressant drug. Inverse agonists bind to receptors however, produces effects opposite to the agonist (Berg & Clarke, 2018). Naltrexone, a partial inverse agonist is used in the management of opioid addiction.
G-coupled proteins and Ion-gated Channels
G-protein receptors and ligand gated ion channels are both cell surface receptors. They are both found on the membrane of the cells. While ligand gated ion channels are controlled by neurotransmitters to release ions, a G-protein depends on the second messenger system to act (Miller & Lappin, 2020).
Therefore, due to the difference in the mechanism of stimulation, ligand gated ion channels take less time (milliseconds) to be activated compared to G-protein receptors which take a bit longer time (seconds). Additionally, examples of ligand gated ion channels include nicotinic acetylcholine receptors and GABA A receptors while G-coupled receptors examples include muscarinic acetylcholine receptors and adrenoceptors (Katzung, 2018; Miller & Lappin, 2020).
Role of Epigenetics in Pharmacologic Action
It has been shown that the gene environment influences its expression. Epigenetics, an emerging scientific area is the study of how the environment, child development, aging or diet influences the changes in gene expression (Ganesan et al., 2019). Epigenetic variations have been linked to multiple conditions such as a variety of cancers and psychiatric disorders.
Therefore, understanding the multiple epigenetic mechanisms and pathways involved is the key to treating such conditions. Drugs such as Decitabine have been used as epigenetic anticancer drugs (Ganesan et al., 2019). This drug manipulates the epigenetic changes and genes therefore, capable of halting the neoplastic progression. Currently, the epigenetic drugs are used alongside routine therapy, an approach which has produced myriad beneficial effects.
Significance of the Information
The information about the pharmacology of drugs is crucial in healthcare. A competent care provider must know the mechanism of actions and potential adverse effects of the drugs. For example, in the management of PD, the nurse must be aware of the pathophysiological mechanisms; the dopamine levels and its receptors. In this case, a nurse is aware that Dopamine agonists are indicated for the management and Dopamine antagonists would worsen the effects.
References
- Berg, K. A., & Clarke, W. P. (2018). Making sense of pharmacology: Inverse agonism and functional selectivity. The International Journal of Neuropsychopharmacology, 21(10), 962–977. doi:10.1093/ijnp/pyy071
- Ganesan, A., Arimondo, P. B., Rots, M. G., Jeronimo, C., & Berdasco, M. (2019). The timeline of epigenetic drug discovery: from reality to dreams. Clinical Epigenetics, 11(1), 174. doi:10.1186/s13148-019-0776-0
- Katzung, B. (2018). Basic & clinical pharmacology (14th ed.). New York: McGraw-Hill.
- Miller, E. J., & Lappin, S. L. (2020). Physiology, Cellular Receptor. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554403/#_NBK554403_pubdet_
- Sheffler, Z. M., Reddy, V., & Pillarisetty, L. S. (2021). Physiology, Neurotransmitters. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539894/
READ MORE >>
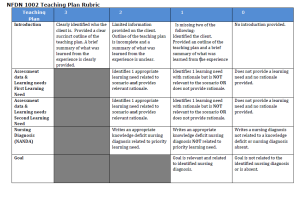
NorQuest College NFDN 1002 Assignment 2: Teaching Plan ExampleOne of the most cr ...
NorQuest College NFDN 1002 Assignment 2: Teaching Plan Example
One of the most crucial aspects of the nursing process is developing a teaching plan. The patient’s active participation in the care process and compliance with instructions are the goals of patient teaching. The paper describes a teaching plan for Mr. Goldblum, a 72-year-old male with an ischemic stroke who has difficulty swallowing, speech and cognition. Patient education is a continuous process until the participants attain their goals, change their goals, or recognize that the goals will not enable them to meet their learning objectives (Anekwe & Rahkovsky, 2018). A stroke is a life-changing event that needs adjustments; therefore, comprehensive teaching is crucial.
Assessment Data and Learning Needs
The teaching plan will cover impaired communication and impaired swallowing. Due to the chronic pattern of stroke, the patient and family need to be trained on the patient’s various deficits, how to improve them, and the need to be patient because the patient may never fully recover to the pre–stoke state (Pierpoint & Pillay, 2020). For example, they are trained on the need for thickened fluids for dysphagia and to protect the airway.
The rationale for this is the request by the patient to take regular fluids despite having difficulty swallowing. Training to improve communication is a crucial need to enhance the achievement of the understanding of the priority need. Alternative communication techniques help to overcome the problem of speech disturbance (Mitchell et al., 2021). The family members later learn to use the tools to enhance communication.
Priority Learning Need and Diagnosis
Improvement in swallowing is the priority patient need. Difficulty swallowing compromises the airway by causing aspiration, which may lead to death. The nursing diagnosis is insufficient knowledge on the management of post-stroke impaired swallowing related to a lack of understanding of the interventions evidenced by the patient’s insistence to take regular foods. The goal is that at the end of the ten sessions, the patient demonstrates feeding methods and decisions that are appropriate to his situation with aspiration prevented. The outcome is the collaboration of the patient with the multidisciplinary care team in making appropriate feeding decisions.
Domains of Learning
The best suitable teaching methods will include psychomotor and cognitive learning. Psychomotor learning will include training the patient and the caregiver on the optimal position that prevents aspiration and methods of improving swallowing. The maneuvers are head turned to the weak side for unilateral pharyngeal paralysis, head back for decreased posterior propulsion of tongue, and lying down on either side for reduced pharyngeal contraction. The patient will be taught how to coordinate the muscles and sensory stimulation techniques to improve swallowing. Cognitive learning will emphasize scheduling of the meals, the preferred food consistency, and other characteristics such as temperature and type.
Barriers to Learning
Communication impairment is a crucial barrier to learning. Difficulty understanding will impede cognitive learning because the patient will not understand the rationale of the feeding decisions we are making for him. Speech difficulty will impair feedback from the patient regarding the teaching and raise any clarifications or concerns. The danger to this is imposing interventions that the patient is uncomfortable with.
Teaching Plan
The training will be done in the patient’s room, in the presence of the caregiver or family. The sessions will be held daily from 8:30 – 9:30 am for one hour for ten days. Later the patient will be referred to an occupational therapist, and early morning is chosen because the patient will not be fatigued. The session will be one hour because the process requires patience. The teaching resources A pen and paper are needed for the patient to write down what he cannot articulate.
The patient and caregiver will be taught about meal scheduling for cognitive learning. The patient should have a minimum of thirty minutes before meals to reduce fatigue and enhance swallowing. The caregiver should be patient with him and avoid distractions during feeding. Alcohol-free moisturizers will be indicated before and after meals to counteract the effects of dry mouth. They will teach appropriate food temperature is either cold or warm to stimulate salivation and that water should be chilled. The level of deficit determines food consistency, and for this patient level, three thickened fluids are indicated for enhanced swallowing. The food shall be placed on the unaffected side of the mouth.
Psychomotor training will include patient positioning, helping the patient with head control, and manual stimulation of the lips to close or open by applying lips or chin pressure. Applying ice on the weak parts of the tongue and stroke the cheek with a tongue blade to improve tongue movement and control. The patient will be scheduled for an exercise program that effectively increases appetite levels by releasing endorphins from the brain.
Evaluation of Learning
Evaluation of the psychomotor domain learning will be by demonstrating appropriate patient positioning and having control. Secondly, the effectiveness of the training will be marked by the caregiver demonstrating appropriate stimulating methods for the lips, tongue, and cheeks (Steigleder et al., 2019).
The patient understanding will mark the effectiveness of cognitive learning, the rationale for the level III feeds, and agreeing to take them. Secondly, the patient and caregiver will be active participants in formulating the treatment plan. During this process, they will demonstrate understanding by strategically scheduling feeding times and types of feeds, choosing appropriate food temperatures, and using the moisturizer. A quiz capturing the teaching areas will gauge their level of understanding.
Analysis of the Teaching process
A patient teaching plan increases patient understanding of a condition and benefits nurses by allowing them to plan their time efficiently. Patient education aids in managing chronic diseases by informing and involving patients in care guides and lifestyle modifications. The patient adopts positive coping mechanisms, and the family is empowered on how to take care of the patient and undertake therapy sessions with them.
A teaching plan helps systematically deliver concepts and skills in a way that does not overload the patient. The nurse does the prior organization of sessions and contents to be covered. Training, especially for chronic patients, ensures the patient’s compliance with the management plan even on discharge. Breaking down information in a manner that the patient understands without distortion or omission challenges using a teaching plan (Steigleder et al., 2019). Secondly, the patient’s state regarding age, culture, cognitive awareness, and attitude affects the patient’s reception of the training.
Conclusion
Teaching planning is an integral part of a nurse’s patient diagnosis. The plan is tailored- based on patient presentation. The teaching plan addresses post-stroke impaired swallowing training incorporating psychomotor and cognitive domain learning. The setting and contents are pre-determined to provide a sense of direction for the nurse. Patient cognitive impairment is the primary barrier to goal achievement. Patient education empowers them and the caregivers to participate actively in the care process.
References
Anekwe, T. D., & Rahkovsky, I. (2018). Self-management: a comprehensive approach to the management of chronic conditions. American Journal of Public Health, 108(S6), S430-S436. https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2014.302041r
Mitchell, C., Gittins, M., Tyson, S., Vail, A., Conroy, P., Paley, L., & Bowen, A. (2021). Prevalence of aphasia and dysarthria among inpatient stroke survivors: describing the population, therapy provision and outcomes on discharge. Aphasiology, 35(7), 950-960. https://doi.org/10.1080/02687038.2020.1759772
Pierpoint, M., & Pillay, M. (2020). Post-stroke dysphagia: An exploration of initial identification and management performed by nurses and doctors. South African Journal of Communication Disorders, 67(1), 1-13. http://dx.doi.org/10.4102/sajcd.v67i1.625
Steigleder, T., Kollmar, R., & Ostgathe, C. (2019). Palliative care for stroke patients and their families: barriers for implementation. Frontiers in Neurology, 10, 164. https://doi.org/10.3389/fneur.2019.00164
NFDN 1002 Assignment 2: Teaching Plan Instructions
Scenario – Mr. Goldblum
Mr. Goldblum is 72 years old and lives in a continuing care facility. He has had a recent ischemic stroke and has right-sided weakness. He was also diagnosed with difficulty swallowing. He has a history of hypertension, treated with Ramipril 10 mg daily. He has recently been started on Coumadin due to the stroke, and has an INR performed weekly. He is on Level 3 thickened fluids. He does not like the thickened fluids and has been asking for regular fluids. His speech was affected by the stroke and at times he is difficult to understand.
Introduction
Clearly identified who the client is. Provided a clear succinct outline of the teaching plan. A brief summary of what was learned from the experience is clearly provided.
3points
Limited information provided on the client. Outline of the teaching plan is incomplete and a summary of what was learned from the experience is unclear and/or one of the components listed is missing.
2points
Is missing two of the following: Identified the client. Provided an outline of the teaching plan and a brief summary of what was learned from the experience
1points
No introduction was provided.
0points
Assessment Data & Learning Needs
2 accurate & appropriate learning needs identified and supported by assessment data (rationale) that is comprehensive and concise based on the case study.
3points
2 basic learning needs identified and supported by assessment data (rationale) that is satisfactory and based on the case study.
2points
Identifies only 1 learning need OR learning needs identified are inaccurate or inappropriate and/or assessment data (rationale) is non-specific or incomplete based on the case study.
1points
Learning needs and assessment data (rationale) are inadequate, irrelevant or absent.
0points
Priority Learning Need & Diagnosis
Identifies priority learning need. Writes an appropriate nursing diagnosis that includes all components of a nursing diagnosis.
2points
Priority learning need is inaccurate or inappropriate. Includes nursing diagnosis but is missing components.
1points
Does not identify priority learning need and/or nursing diagnosis.
0points
Goal
Goal is relevant, appropriate and based on the priority health need.
2points
Goal is satisfactory, basic and based on the priority health need.
1points
Goal is inadequate, irrelevant or absent.
0points
Expected Outcome (SMART Criteria)
Expected outcome is relevant, appropriate, based on the learning needs and is related to the nursing diagnosis and contains all elements of SMART criteria
2points
Expected outcome is inaccurate or inappropriate, and is not related to the learning need and/or nursing diagnosis and/or is incomplete re: SMART criteria.
1points
Expected outcome is irrelevant or absent.
0points
Learning Domain
Information identified is accurate, prioritized and appropriate for the case study. Includes literature reference.
3points
Information identified is satisfactory, prioritized and/or somewhat appropriate for the case study. Includes reference.
2points
Information identified is off topic, and/or inappropriately prioritized for the case study. May or may not include reference.
1points
Information is inadequate, irrelevant or absent.
0points
Barriers to Learning
Chosen barriers are accurate and relevant for the section. Rationale is comprehensive and concise.
3points
Chosen barriers are somewhat accurate and relevant for the scenario. Rationale is satisfactory and basic.
2points
Chosen barriers are non-specific or off topic. Rationale is limited or absent.
1points
Chosen barriers are inappropriate, inadequate or absent.
0points
Teaching Plan: Educational Content
Comprehensive, concise and relevant information is provided for the section. Education content is appropriate and meaningful to the case study. Literature support provided.
3points
Satisfactory and basic information is provided for the section. Education content is somewhat appropriate and/or relevant to the case study. Adequate literature support provided.
2points
Information is minimal and/or limited for the section. Educational content is off topic or not always appropriate to the case study. Minimal literature support.
1points
Information is inadequate, irrelevant or absent. No literature support.
0points
Teaching Plan: Teaching Methods
Teaching methods are appropriate and relevant for the teaching plan. Literature support provided.
3points
Teaching methods are satisfactory and appropriate for the teaching plan. Adequate literature support provided.
2points
Teaching methods are non-specific or incomplete and are off-topic or not appropriate. Minimal literature support.
1points
Teaching methods are inappropriate, off-topic or absent. No literature support.
0points
Teaching Plan: Teaching Resources
Resources are appropriate, insightful and relevant to the teaching plan. Literature support provided.
3points
Resources are basic and satisfactory, and/or somewhat relevant to the teaching plan. Adequate literature support provided.
2points
Resources are minimal, limited and/or may not be relevant to the teaching plan. Minimal literature support.
1points
Resources are inadequate, irrelevant or absent. No literature support.
0points
Evaluation of Learning
Criteria is comprehensive, accurate and relevant for the section.
3points
Criteria is basic, satisfactory and appropriate for the section.
2points
Criteria is non-specific or incomplete. Evidence is off-topic, limited or not appropriate.
1points
Criteria is inappropriate, inadequate or absent.
0points
Reflection of the Teaching Process
Comprehensive, concise and relevant arguments are provided to highlight the importance of teaching plans.
3points
Satisfactory and basic arguments are provided to highlight the importance of teaching plans.
2points
Non-specific or incomplete arguments are provided related to the importance of teaching plans.
1points
Content is inappropriate, inadequate or absent.
0points
Reflection: Strengths and weaknesses of using the teaching plan.
Comprehensive, concise and relevant information is provided. Content is clear, appropriate and meaningful.
3points
Satisfactory, basic and appropriate information is provided. Content presented is somewhat clear and/or missing strengths or weaknesses
2points
Information presented is minimal. Content may be off topic and/or not appropriate.
1points
Information is inadequate, irrelevant or absent.
0points
Reflection: Benefits of using a teaching plan in future practice.
Comprehensive, concise and relevant information is provided. Content provided is clear, appropriate
3points
Satisfactory, basic and appropriate information is provided. Benefits presented are vague.
2points
Benefit information presented is minimal. Content may be off topic and/or not appropriate
1points
Information is inadequate, irrelevant or absent.
0points
Conclusion
Presents a logical, clear, concise summary of main points; presents clear recommendations on changes to be made next time teaching this topic
3points
Provides a conclusion but does not summarize main points and/or recommendations on changes to be made next time teaching this topic.
2points
Does not adequately explain findings or recommendations on changes to be made next time teaching this topic
1points
Conclusion not provided
0points
Grammar/Sentence Structure
Free from writing convention errors
1points
Many/Significant writing convention errors
0points
APA Formatting
Free from APA formatting errors
1points
Many/significant APA errors
0points
NFDN_1002_Teaching_Plan_Assignment.docx.pdf
NFDN_1002_Teaching_Plan_Rubric_2020.pdf
NFDN_1002_TEMPLATE_ASSIGNMENT_2_TEACHING_PLAN_(4)
READ MORE >>
NHS-FP6004 Assessment 2 Policy ProposalNHS-FP6004 Assessment 2 Policy ProposalDr ...
NHS-FP6004 Assessment 2 Policy Proposal
NHS-FP6004 Assessment 2 Policy Proposal
Draft a written proposal and implementation guidelines for an organizational policy that you believe would help lead to an improvement in quality and performance associated with the benchmark metric for which you advocated action in Assessment 1.
Note: Each assessment in this course builds on the work you completed in the previous assessment. Therefore, you must complete the assessments in this course in the order in which they are presented.
In advocating for institutional policy changes related to local, state, or federal health care laws or policies, health leaders must be able to develop and present clear and well-written policy and practice guidelines change proposals that will enable a team, unit, or the organization as a whole to resolve relevant performance issues and bring about improvements in the quality and safety of health care. This assessment offers you an opportunity to take the lead in proposing such changes.
Assessment Instructions for NHS-FP6004 Assessment 2 Policy Proposal
In this assessment, you will build on the dashboard benchmark evaluation work you completed in Assessment 1.
PREPARATION
After reviewing your benchmark evaluation, senior leaders in the organization have asked you to draft a policy change proposal and practice guidelines addressing the benchmark metric for which you advocated action.
In their request, senior leaders have asked for a proposal of not more than 2–4 pages that includes a concise policy description (about one paragraph), practice guidelines, and 3–5 credible references to relevant research, case studies, or best practices that support your analysis and recommendations. You are also expected to be precise, professional, and persuasive in justifying the merit of your proposed actions.
When creating your policy and guidelines it may be helpful to utilize the template that your current care setting or organization uses. Your setting’s risk management or quality department could be a good resource for finding an appropriate template or format. If you are not currently in practice, or your care setting does not have these resources, there are numerous appropriate templates freely available on the Internet.
PROPOSAL REQUIREMENTS for NHS-FP6004 Assessment 2 Policy Proposal
Note: The tasks outlined below correspond to grading criteria in the scoring guide.
In your proposal, senior leaders have asked that you:
- Explain why a change in organizational policy or practice guidelines is needed to address a shortfall in meeting a performance benchmark prescribed by applicable local, state, or federal health care laws or policies.
- What is the current benchmark for the organization? What is the numeric score for the underperformance?
- How might the benchmark underperformance be affecting the quality of care being provided or the operations of the organization?
- What are the potential repercussions of not making any changes?
- Recommend ethical, evidence-based strategies to resolve the performance issue.
- What does the evidence-based literature suggest are potential strategies to improve performance for your targeted benchmark?
- How would these strategies ensure improved performance or compliance with applicable local, state, or federal health care laws or policies?
- How would you propose to apply these strategies in the context of your chosen professional practice setting?
- How would you ensure that the application of these strategies is ethical and culturally inclusive?
- Does your policy encompass the key components of your recommendations?
- Analyze the potential effects of environmental factors on your recommended strategies.
- What regulatory considerations could affect your recommended strategies?
- What organizational resources could affect your recommended strategies (for example, staffing, finances, logistics, and support services)?
- Are your policy and guidelines realistic in light of existing environmental factors?
- Propose a succinct policy and guidelines to enable a team, unit, or the organization as a whole to implement recommended strategies to resolve the performance issue related to the relevant local, state, or federal health care policy or law.
- Identify colleagues, individual stakeholders, or stakeholder groups who should be involved in further development and implementation of your proposed policy, guidelines, and recommended strategies.
- Why is it important to engage these colleagues, individual stakeholders, or stakeholder groups?
- Do your proposed guidelines help colleagues, individual stakeholders, or stakeholder groups understand how to implement your proposed policy?
- How might engaging these colleagues, individual stakeholders, or stakeholder groups result in a better organizational policy and smoother implementation?
- Are your proposal and recommended strategies realistic, given the care team, unit, or organization you are considering?
- Communicate your proposed policy, guidelines, and recommended strategies in a professional and persuasive manner.
- Write clearly and logically, using correct grammar, punctuation, and mechanics.
Integrate relevant sources to support your arguments, correctly formatting source citations and references using current APA style.
- Did you cite an additional 3–5 credible sources to support your analysis and recommendations?
SUGGESTED RESOURCES
The resources provided here are optional. You may use other resources of your choice to prepare for this assessment; however, you will need to ensure that they are appropriate, credible, and valid. The NHS-FP6004 – Health Care Policy and Law Library Guide can help direct your research, and the Supplemental Resources and Research Resources, both linked from the left navigation menu in your courseroom, provide additional resources to help support you.
Ethical Decision-Making to Improve Quality Performance

This interactive media applies an ethical decision-making process to a workplace health care issue in a hypothetical scenario, which may give you some ideas about how to incorporate ethical considerations into your policy change.
Organizational Ethics Decision-Making Process in Health Care.
This short briefing outlines issues related to quality-related policy development and the potential solutions offered by new regulations such as the Medicare Access and CHIP Reauthorization Act (MACRA) and the ACA.
- Whitlock, R. (2016, April 15). United States: Talking about the challenge of quality in health care policy development. Mondaq Business Briefing.
NHS-FP6004 Assessment 2 Policy Proposal Example
Statistics show there are preventable measures to reduce falls and avoid them from reoccurring. Typically, 700,000 and 1 million patients fall in hospitals yearly, as stated by the Agency for Healthcare Research and Quality.
Data reports show that many of the patients who fail are not seriously hurt, however, fall rate injuries are substantial. The Joint Commission data shows an average growth in a hospital’s overhead costs for an injury that is fall-related costs the hospital more than $13,000, and the patient’s time spent increases by an average of 6.27 days.
Also, research shows that between 30 and 51 percent of falls result in an injury. (Butcher, 2017) Mercy Medical dashboard metrics data showed an increase in falls and documentation errors due to the mistakes of employees in the years 2015 and 2016.
Many factors can lead to high fall rates, such as poor communication between staff, incorrect documentation, and poor nurse assessments. This policy proposal should be considered to decrease the number of falls and prevent the possibility of falls from occurring. Furthermore, this will increase overall performance, the likelihood of meeting targets, and effective patient care delivery.
Ethical Evidence-Based Strategies
Improving the performance of this benchmark can be accomplished through various ways to decrease preventable falls. Strategic planning will provide a direction in making tough decisions for Medical Mercy Center to deliver superior service to their patients and prevent falls, reducing readmission rates. This policy proposal will support MMC’s leadership to acknowledge a weakness within the organization and implement ways to improve those areas of underperformance.
A lack of communication between staff has caused the fall rates to increase in the center. The “SBAR” concept (situation, background, assessment and, recommendations) is a great tool for maintaining effective communication. Communicating with the staff by using the “SBAR” concept will significantly reduce the chances of miscommunication from the staff and decrease any preventable falls from happening again.
Each time a nurse assesses a patient, using the SBAR concept will support them in identifying the patient’s situation, background, and application recommendations. This will be a great resource in which nurses can then contribute to an enhanced assessment and recommendations on what the patient will need for future treatment. (Lee., Dong, Lim, Poh., & Lim, 2016).
Strategies should be established for patients who are at risk for falls, which are known to cause injuries to patients. There also should be ways to alert employees if patients are falling more often or patients that could potentially be at risk of falling. Implementing a color-coded system identifying a patient as a fall risk will support decreasing falls and educating new staff about the program.
Proposed Policy
A policy is brought to the attention of the stakeholders and leaders of Mercy Medical due to the systematic failure of reoccurring falls. It is up to the leaders of this organization to bring about change to increase patient satisfaction and patient safety. It is vital to take in the necessary strategies to reduce falls from transpiring. These strategies can contribute to influencing high-quality patient care. (Rawlins, 2014)
Competent staff will support the decrease of stress brought on by an increased workload and the pressures of being short-staffed. Having a knowledgeable team would help when chaotic situations arise and patient care is jeopardized.
It would help relieve the pressures towards a single employee and help to keep each other accountable as a team and decrease unnecessary shortcuts made by an employee. Requiring reporting of fall incidents will help the organization find the areas of weaknesses within the staff and organization. Putting into practice inquiring about the employees’ needs will create a stress-free environment.
Alerts should be issued to patients who are at high risk for falls. Using a color-coded system identifying the fall risk will help employees lessen repeated falls. Educating patients and staff members about the fall prevention policy would be vital in applying safe practices. (Morse,2018)
Conclusion
Human errors are common, but they can be avoided by focusing on education and implementing safe practices. Mercy Medical does not have to be a part of patient fall statistics. Implementing these policies within the organization will provide exemplary safe practices to serve as a role model for organizations and those within the organization.
It’s up to the leaders at Mercy Medical to set the right policies and make impacting changes that would enhance the quality of patient care. We may never be able to prevent patient falls completely, but with strategic efforts and skilled decision-making, we will provide our staff with the best opportunities to minimize falls and maximize patient care.
MMC Fall Prevention Policy
Effective date: October 14, 2019
I. PURPOSE:
To reduce and avoid falls by medication, ensuring proper nurse assessments and reducing risks to provide excellent quality care and correct usage of preventive and protective measures
II. POLICY:
- All patients should be adequately assessed and classified as to what type of fall risk they are identified when being admitted according to the policy and procedures of Mercy Medical. If any patients are considered high fall risk, all alerts, preventative, and protective measures are considered and must be put in place to ensure proper
- If a patient has a fall, the fall must be reported and documented in the system and a written report.
- All staff and leadership must be notified of an unlikely event and must be handled appropriately with the necessary actions for the patient to be taken care
- The patient must be adequately informed and given instructions and a detailed summary of the
III. Procedure:
- If an unlikely event occurs, the fall must be reported to the manager and director.
- An incident report must be filled out on the detailed location, type of fall and description of the
- A thorough patient follow-up must ensue and all safety precautions should be taken into effect.
- A follow-up meeting should be held with the manager and all leadership, including staff, to ensure the incident does not occur
NHS-FP6004 Assessment 2 Policy Proposal Resources
Butcher, L. (2017, June 1). The No-Fall Zone. Retrieved from https://www.hhnmag.com/articles/6404-Hospitals-work-to-prevent-patient-falls.
Lee, S. Y., Dong, L., Lim, Y. H., Poh, C. L., & Lim, W. S. (2016). SBAR: towards a common interprofessional team-based communication tool. Medical Education, 50(11), 1167– 1168. https://doi-org.library.capella.edu/10.1111/medu.13171
Morse, J. M. (2008). Preventing patient falls: Second edition. Retrieved from https://ebookcentral-proquest-com.library.capella.edu
Rawlins, M. D. (2014). Engaging with health-care policy. The Lancet, 383, S7-8. doi:http://dx.doi.org.library.capella.edu/10.1016/S0140-6736(14)60048-9
READ MORE >>
huh? Yeah it’d be good to have a disaster plan. It’s hard to do in real li ...
READ MORE >>
NHS-FPX 4060 Assessment 3 Disaster Recovery PlanWhen it comes to NHS-FPX 4060 As ...
NHS-FPX 4060 Assessment 3 Disaster Recovery Plan
When it comes to NHS-FPX 4060 Assessments, rest assured we can help you complete all the tasks, from assessment 1 to assessment 4. Here we have shown you assessment 3 instructions as well as sample paper. Use the sample paper to assess the quality of work we can deliver to you anytime. Chat us for more information. Or simply place your order and let us work it out for you.
Assessment 3 Instructions: Disaster Recovery Plan
- Develop a disaster recovery plan to lessen health disparities and improve access to community services after a disaster. Develop an oral presentation, 6 pages, for the Vila Health system, city officials, and the disaster relief team.

Professional Context
Nurses perform a variety of roles and their responsibilities as health care providers extend to the community. The decisions we make daily and in times of crisis often involve the balancing of human rights with medical necessities, equitable access to services, legal and ethical mandates, and financial constraints.
In the event of a major accident or natural disaster, many issues can complicate decisions concerning the needs of an individual or group, including understanding and upholding rights and desires, mediating conflict, and applying established ethical and legal standards of nursing care. As a nurse, you must be knowledgeable about disaster preparedness and recovery to safeguard those in your care. As an advocate, you are also accountable for promoting equitable services and quality care for the diverse community.
Nurses work alongside first responders, other professionals, volunteers, and the health department to safeguard the community. Some concerns during a disaster and recovery period include the possibility of death and infectious disease due to debris and/or contamination of the water, air, food supply, or environment. Various degrees of injury may also occur during disasters, terrorism, and violent conflicts.
To maximize survival, first responders must use a triage system to assign victims according to the severity of their condition/prognosis in order to allocate equitable resources and provide treatment. During infectious disease outbreaks, triage does not take the place of routine clinical triage.
Trace-mapping becomes an important step to interrupting the spread of all infectious diseases to prevent or curtail morbidity and mortality in the community. A vital step in trace-mapping is the identification of the infectious individual or group and isolating or quarantining them. During the trace-mapping process, these individuals are interviewed to identify those who have had close contact with them. Contacts are notified of their potential exposure, testing referrals become paramount, and individuals are connected with appropriate services they might need during the self-quarantine period (CDC, 2020).
An example of such disaster is the COVID-19 pandemic of 2020. People who had contact with someone who were in contact with the COVID-19 virus were encouraged to stay home and maintain social distance (at least 6 feet) from others until 14 days after their last exposure to a person with COVID-19. Contacts were required to monitor themselves by checking their temperature twice daily and watching for symptoms of COVID-19 (CDC, 2020).
Local, state, and health department guidelines were essential in establishing the recovery phase. Triage Standard Operating Procedure (SOP) in the case of COVID-19 focused on inpatient and outpatient health care facilities that would be receiving, or preparing to receive, suspected, or confirmed COVID- 19 victims. Controlling droplet transmission through hand washing, social distancing, self-quarantine, PPE, installing barriers, education, and standardized triage algorithm/questionnaires became essential to the triage system (CDC, 2020; WHO, 2020).
This assessment provides an opportunity for you to apply the concepts of emergency preparedness, public health assessment, triage, management, and surveillance after a disaster. You will also focus on evacuation, extended displacement periods, and contact tracing based on the disaster scenario provided.
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
- Competency 1: Analyze health risks and health care needs among distinct populations.
- Describe the determinants of health and the cultural, social, and economic barriers that impact safety, health, and disaster recovery efforts in a community.
- Competency 2: Propose health promotion strategies to improve the health of populations.
- Present specific, evidence-based strategies to overcome communication barriers and enhance interprofessional collaboration to improve disaster recovery efforts.
- Competency 3: Evaluate health policies, based on their ability to achieve desired outcomes.
- Explain how health and governmental policy affect disaster recovery efforts.
- Competency 4: Integrate principles of social justice in community health interventions.
- Explain how a proposed disaster recovery plan will lessen health disparities and improve access to community services.
- Competency 5: Apply professional, scholarly communication strategies to lead health promotion and improve population health.
- Organize content with clear purpose/goals and with relevant and evidence-based sources (published within 5 years).
Preparation for NHS-FPX-4060 Assessment 3 Disaster Recovery Plan
When disaster strikes, community members must be protected. A comprehensive recovery plan, guided by the MAP-IT (Mobilize, Assess, Plan, Implement, Track) framework, is essential to help ensure everyone’s safety. The unique needs of residents must be assessed to lessen health disparities and improve access to equitable services after a disaster.
Recovery efforts depend on the appropriateness of the plan, the extent to which key stakeholders have been prepared, the quality of the trace-mapping, and the allocation of available resources. In a time of cost containment, when personnel and resources may be limited, the needs of residents must be weighed carefully against available resources.
In this assessment, you are a community task force member responsible for developing a disaster recovery plan for the Vila Health community using MAP-IT and trace-mapping, which you will present to city officials and the disaster relief team.
To prepare for the assessment, complete the Vila Health: Disaster Recovery Scenario simulation.
In addition, you are encouraged to complete the Disaster Preparedness and Management activity. The information gained from completing this activity will help you succeed with the assessment as you think through key issues in disaster preparedness and management in the community or workplace. Completing activities is also a way to demonstrate engagement.
Begin thinking about:
- Community needs.
- Resources, personnel, budget, and community makeup.
- People accountable for implementation of the disaster recovery plan.
- Healthy People 2020 goals and 2030 objectives.
- A timeline for the recovery effort.
You may also wish to:
- Review the MAP-IT (Mobilize, Assess, Plan, Implement, Track) framework, which you will use to guide the development of your plan:
- Mobilize collaborative partners.
- Assess community needs.
- Plan to lessen health disparities and improve access to services.
- Implement a plan to reach Healthy People 2020 goals or 2030 objectives.
- Track community progress.
- Review the assessment instructions and scoring guide to ensure that you understand the work you will be asked to complete.
NHS-FPX-4060 Assessment 3 Disaster Recovery Plan Instructions
Every 10 years, The U.S. Department of Health and Human Services and the Office of Disease Prevention and Health Promotion release information on health indicators, public health issues, and current trends. At the end of 2020, Healthy People 2030 was released to provide information for the next 10 years.
Healthy People 2030 provides the most updated content when it comes to prioritizing public health issues; however, there are historical contents that offer a better understanding of some topics. Disaster preparedness is addressed in Healthy People 2030, but a more robust understanding of MAP-IT, triage, and recovery efforts is found in Healthy People 2020. For this reason, you will find references to both Healthy People 2020 and Healthy People 2030 in this course.
Complete the following:
- Develop a disaster recovery plan for the Vila Health community that will lessen health disparities and improve access to services after a disaster. Refer back to the Vila Health: Disaster Recovery Scenario to understand the Vila Health community.
- Assess community needs.
- Consider resources, personnel, budget, and community makeup.
- Identify the people accountable for implementation of the plan and describe their roles.
- Focus on specific Healthy People 2020 goals and 2030 objectives.
- Include a timeline for the recovery effort.
- Apply the MAP-IT (Mobilize, Assess, Plan, Implement, Track) framework to guide the development of your plan:
- Mobilize collaborative partners.
- Assess community needs.
- Use the demographic data and specifics related to the disaster to identify the needs of the community and develop a recovery plan. Consider physical, emotional, cultural, and financial needs of the entire community.
- Include in your plan the equitable allocation of services for the diverse community.
- Apply the triage classification to provide a rationale for those who may have been injured during the train derailment. Provide support for your position.
- Include in your plan contact tracing of the homeless, disabled, displaced community members, migrant workers, and those who have hearing impairment or English as a second language in the event of severe tornadoes.
- Plan to lessen health disparities and improve access to services.
- Implement a plan to reach Healthy People 2020 goals and 2030 objectives.
- Track and trace-map community progress.
- Use the CDC’s Contract Tracing Resources for Health Departmentsas a template to create your contact tracing.
Describe the plan for contact tracing during the disaster and recovery phase.
NHS-FPX-4060 Assessment 3 Disaster Recovery Plan Graded Requirements
The requirements outlined below correspond to the grading criteria in the scoring guide, so be sure to address each point:
- Describe the determinants of health and the cultural, social, and economic barriers that impact safety, health, and recovery efforts in the community.
- Consider the interrelationships among these factors.
- Explain how your proposed disaster recovery plan will lessen health disparities and improve access to community services.
- Consider principles of social justice and cultural sensitivity with respect to ensuring health equity for individuals, families, and aggregates within the community.
- Explain how health and governmental policy impact disaster recovery efforts.
- Consider the implications for individuals, families, and aggregates within the community of legislation that includes, but is not limited to, the Americans with Disabilities Act (ADA), the Robert T. Stafford Disaster Relief and Emergency Assistance Act, and the Disaster Recovery Reform Act (DRRA).
- Present specific, evidence-based strategies to overcome communication barriers and enhance interprofessional collaboration to improve the disaster recovery effort.
- Consider how your proposed strategies will affect members of the disaster relief team, individuals, families, and aggregates within the community.
- Include evidence to support your strategies.
- Organize content with clear purpose/goals and with relevant and evidence-based sources (published within 5 years).
- Develop your presentation with a specific purpose and audience in mind.
- Adhere to scholarly and disciplinary writing standards and APA formatting requirements.
MUST INCLUDE !!!!!
- Provides a concise, accurate description of the determinants of health and the cultural, social, and economic barriers that impact safety, health, and disaster recovery efforts in a community. Clearly describes the interrelationships among these factors.
- Explains how a proposed disaster recovery plan will lessen health disparities and improve access to community services. Provides clear insight into how principles of social justice and cultural sensitivity help to ensure health equity for individuals, families, and aggregates in the community.
- Explains how health and governmental policy impact disaster recovery efforts. Articulates the logical policy implications for community members linked to specific policy provisions.
- Presents specific, evidence-based strategies to overcome communication barriers and enhance interprofessional collaboration to improve disaster recovery efforts that are well-supported by with relevant and credible evidence. Articulates the implications and potential consequences of proposed strategies.
- Organizes content with clear purpose/goals. support main points, assertions, arguments, conclusions, or recommendations with relevant and evidence-based sources (published within 5 years).
Disaster Recovery Plan Sample Paper
Name (Presenter) Institution Affiliated
Introduction and Objectives
- Disaster Recovery Plan-An approach to preserve an organization during and
after an emergency or disastrous event.
- Disaster-A catastrophic event that causes significant damage or deaths
Objectives
- Discuss Determinants of Health
- Identify the needs of the community and develop a recovery plan
- Discuss the tools and personal resources to implement it
- Discuss principles of social justice and cultural sensitivity
- Describe the obstacles that health and disaster recovery initiatives face
- How to avoid communication barriers, and improve inter-professional
collaboration
Determinants of Health
- Definition-Factors that affect health of a population
- At Vila Health Community, the factors include the following
- Economic status-The need to reduce health disparity as a
target of the plan
? Health services-Reduced access to health services after a
disaster
? Physical environment
- Policy making-affects health of patients (Healthy People, 2020)
The Needs of the Vila Health Community
? The purpose of the disaster strategy plan for Villa Health Community is to lessen health disparities and improve access to services after a disaster
? Derived needs from the main the purpose of the disaster strategy plan include
? Favorable public policies
? Improved public services
? Health services
? Education
? Transport and communication
Tools To Implement the Disaster Recovery Plan
MAP-IT Framework
? MAP-IT (Mobilize, Assess, Plan, Implement, Track) is a tool for planning and evaluating public health interventions
? It involves all stakeholders
? Assessment means that the effort will start
from the reality of the community
Change of Command
? The basic ingredient of any recovery plan
? Involvement of different agencies in addition to the community emergency response
? Determining the leading agencies in the
recovery process
Disaster Recovery Members and Recovery Timeline
Disaster Recovery Members
? Selection of executive and team members
? Introduction of the parties to the region (McGinnis, 2021)
? Allocations of various roles to different members
General Disaster Recovery Plan Timeline
? Stipulation of the extend of recovery plan implementation
? Keep track of timing of major activities to be implemented during different phases of recovery (McGinnis, 2021)
Barriers to Safety Health and Disaster Recovery Efforts
? Cultural barriers-Rigidity in beliefs (religion) and language
differences
? Economic barriers
? Financial constraints
? Social barriers
? Poor collaboration between the disaster management team
? Ineffective communication among the disaster management team
? Lack of an integrated disaster management system
Proposed Disaster Recovery Plan and Benefits
? The purpose of the proposed disaster recovery plan is to reduce health
disparities and improve access to services through
? Focusing on the most disadvantaged groups (Stafford & Wood, 2017)
? Narrowing Health gaps
? Reducing the social gradient
? Recovery plan inclusive of all patients irrespective of their demographics (reduces disparity) (Stafford & Wood, 2017)
? Infrastructure improvement-improve access to services (Yu et al., 2017)
? The DR plan ensures that the critical areas necessary for return to normalcy
are handled (CDC, 2020).
Social Justice and Cultural Sensitivity
? Equity, as a principle of social justice is applied in healthcare
? Care is given based on the need
? Cultural sensitivity-Enables delivery of culturally competent care
? Ability to acknowledge cultural norms of patients-skill of a care
provider
? Enables provision of a nonbiased care to a diverse group (CDC,
2020)
? Fairness in provision of care irrespective of the differences-
equity
Health and Governmental Policies
? Federal Emergency Management Agency [FEMA] (2017) outlines
the policies
? Example-Presidential Policy Directive 8-whole community
involvement
? Disaster Recovery Reform Act of 2018 -prepares a nation for a future
disaster
? Impact on recovery efforts are as follows
? Encourages collaboration among community-shared responsibility
? Policies support creation of a national preparedness goal
? Identification of loopholes to be addressed
Overcoming Communication Barrier
? Non-functional communication that may result during a disaster
includes
? Problem coordinating radio communication
? No contact with first responders the first few hours
? Language boards
? Kwik point Medical Translator
? Mobile apps to inform the emergency center (Abbas & Norris, 2018)
? Activate emergency alarms
? Use of social media to reach a massive population (Abbas & Norris, 2018)
How to Enhance Inter-professional Collaboration (IPC)
? Various professions displayed by the case
? Health care workers, administrators, financial officers
? EMTs, police, fire department team
? Disorganization during the catastrophe reveals a poor IPC
? Delegation of duties help (Digregorio et al., 2019)
? Implementation of IPC education in schools
? Proper disaster plan-specify role of each participant
Conclusion
? Economic status, physical environment and policies determine
their health
? Cultural, economic and social factors can be barriers to disaster
recovery efforts
? Proposed plan-reduce health disparity; improve health access
? Governmental or state policies significantly affect health
? Language boards, cell phones, social media enhance communication
? Delegation, IPC education, proper disaster plan enhance IPC
References
? Abbas, R., & Norris, T. (2018). Inter-Agency Communication and Information Exchange in Disaster Healthcare. ISCRAM, 2- 7.
? Centers for Disease Control and Prevention. (2020). Emergency Preparedness and Response. Retrieved from CDC: https://emergency.cdc.gov/
? Department of Economic and Social Affairs. (2019). Population and Vital Statistics Report: Statistical Papers Series A Vol.
LXXI. New York: United Nations.
? Digregorio, H., Graber, J. S., Saylor, J., & Ness, M. (2019). Assessment of inter-professional collaboration before and after a
simulated disaster drill experience. Nurse education today (79, 194-197.
? Federal Emergency Management Agency (FEMA). (2017). Pre-Disaster Recovery Planning Guide for Local Governments.
FEMA Publication FD 008-03, 5-10.
? Healthy People. (2020). Determinants of Health. Retrieved from U.S Department of Health and Human Services: https://www.healthypeople.gov/2020/about/foundation-health-measures/Determinants-of-Health
? McGinnis, J. M. (2021). Healthy people 2030: A compass in the storm. Journal of Public Health Management and Practice:
JPHMP, Publish Ahead of Print(6), S213–S214. https://doi.org/10.1097/phh.0000000000001328
? Stafford, A., & Wood, L. (2017). Tackling health disparities for people who are homeless? Start with social determinants.
International Journal of Environmental Research and Public Health, 14(12), 1535. https://doi.org/10.3390/ijerph14121535
? Yu, S. W. Y., Hill, C., Ricks, M. L., Bennet, J., & Oriol, N. E. (2017). The scope and impact of mobile health clinics in the United States: a literature review. International Journal for Equity in Health, 16(1), 178. https://doi.org/10.1186/s12939-017- 0671-2
VILA HEALTH Disaster Recovery Scenario (NHS-FPX-4060 Assessment 3: Disaster Recovery Plan)
For a health care facility to be able to fill its role in the community, it must actively plan not only for normal operation, but also for worst-case scenarios which could occur. In such disasters, the hospital’s services will be particularly crucial, even if the specifics of the disaster make it more difficult for the facility to stay open.
In this scenario, you will resume your role as the senior nurse at Valley City Regional Hospital. Like many facilities within the Vila Health network, Valley City Regional serves as the primary source of health care for a wide area of North Dakota. As such, it is even more imperative than usual that it stay open and operational in all situations. Doing this means planning and preparation.
The administrator of the hospital, Jennifer Paulson, wants to talk to you about disaster preparedness and recovery at Valley City Regional. But first, you should read some background information about events in Valley City in the past few years, including the involvement of the hospital.
ARTICLE:
HOPE FOR THE BEST, PLAN FOR THE WORST
Op-ed by Anne Levy, Valley City Herald
Valley City has had a great year, growing on a number of fronts. But all of our growth and success exists in the shadow of the recent past, a case of recent wounds slowly healing and fading to scars.
No one who was in Valley City two years ago will ever forget the catastrophic derailment of an oil-tanker train and the subsequent explosion and fire. While fatalities were fewer than they could have been, six residents of our city lost their lives. Nearly two hundred were hospitalized, and much of the city was temporarily evacuated. Several homes near the railroad tracks were leveled, and our water supply was contaminated by oil leakage for several months.
Life has resumed, and we have begun to thrive again, in our fashion. But the nagging feeling recurs: When the disaster struck, were our institutions properly prepared? No one wakes up in the morning expecting a train derailment, of course. But responsible institutions think about things that could go wrong within the realm of possibility, and make a plan. Many individuals performed brave, inspired, selfless service in the chaos of the derailment, but it is clear in retrospect that much of the work was improvised, disorganized, and often circular or at cross-purposes.
For the first two hours of the crisis, the Valley City Fire Department was caught unprepared by the damage to the city water supply caused by the explosion, which was more extensive than had been considered possible. The Fire and Police departments had trouble coordinating radio communications, and a clear chain of command at the scene between departments was painfully slow to emerge. The hospital was woefully understaffed for the first six hours of the crisis, taking far too long to find a way to bring additional staff and resources onto the scene. The city health department was unacceptably dilatory in testing the municipal water supply for contaminants.
A call from the Herald’s offices to City Hall confirmed that the city’s disaster plan is over a decade old, and is unfortunately myopic both in the events it considers as possible disasters and in the agencies it plans for. It is of utmost importance to the future of our city that this plan be revised, revisited, and expanded. All city agencies should review their own disaster plans and coordinate with the city for a master plan. The same goes for crucial non-government agencies, most especially the Valley City Regional Hospital. Of course, this all exists in the shadow of budget cuts both at city hall and the hospital.
The sun is shining today, without a cloud in the sky. This is the time to make sure we are ready for the next storm, so to speak, to hit our city. No one knows what the next crisis will be or when it will come. But we can count on the fact that no one will get up that morning expecting it.
FACT SHEET:
Valley City, ND, Demographics – NHS-FPX-4060 Assessment 3: Disaster Recovery Plan
Population: 8,295 (up from 6,585 in 2010 census)
Median Age: 43.6 years. 17.1% under age 18; 14.8% between 18 and 24; 21.1% between 25 and 44; 24.9% 46 – 64; 22% 65 or older.
Officially, residents are 93% white, 3% Latino, 2% African-American, 1% Native American, 1% other.
—additionally, unknown number of undocumented migrant workers with limited English proficiency
Special needs: 204 residents are elderly with complex health conditions; 147 physically disabled and/or use lip-reading or American Sign Language to communicate.
Note that the Valley City Homeless shelter runs at capacity and is generally unable to accommodate all of the city’s homeless population. Also, the city is in the midst of a financial crisis, with bankruptcy looming, and has instituted layoffs at the police and fire departments.
Valley City Region Hospital Fact Sheet
105-bed hospital (currently 97 patients; 5 on ventilators, 2 in hospice care.)
NOTEWORTHY: Both of VCRH’s ambulances are aging and in need of overhaul. Also, much of the hospital’s basic infrastructure and equipment is old and showing wear. The hospital has run at persistent deficits and has been unable to upgrade; may be looking at downsizing nursing staff.
Jennifer Paulson
Administrator, Valley City Hospital
Hello, thanks for stopping by. I hope you’re settling in well.
I’d been planning on talking to you about disaster planning in the near future anyway, but now it looks like it’s a lot more urgent. I’m not sure if you’ve heard, but the National Weather Service says we’re going to be at an elevated risk for severe tornadoes in Valley City this season. I’m taking that as a clear sign that it’s time we get serious about disaster planning.
And it’s not just me… The mayor just called me and asked the hospital to check our preparedness for a mass-casualty event, given recent qualms about the way the derailment was handled. For instance, did you see that op-ed in the paper about disaster planning?
Anyway. My particular concern is patient triage in the near term and recovery efforts over the next six months. As I work on a more formal response to the Mayor about where we’re at for this threat, I’d appreciate it if you could do some research and planning on this matter. Even if we dodge the bullet on these tornadoes, there’ll be something else in the future. We need to stop putting it off and get serious about our disaster planning.
What I’d like for you to do first is take some time to talk to a good cross-section of people here at the hospital about what happened last time, and about our disaster plan in general. Make sure you get people from administration as well as frontline care staff; after all, problems can be visible in one area but not another a lot of times.
So spread it around! Since you weren’t here for the train crisis, I think you’re in a unique position to have a fresh, unbiased outlook on it. Actually, first you might find it useful to take a look at the hospital fact sheet, just to brush up on our basics here.
After you’ve looked at the fact sheet and done some talking to people, I’d like you to swing back by and we’ll talk about next steps.
Thanks!
Kate McVeigh
RN
Hey there! Yeah, I think I have a minute or two to talk about the derailment. Wow. It’s crazy. I guess that’s been a while, but it still feels like it just happened. It’s all so vivid!
I was on shift when it happened, so I was here for the whole thing. The blast, the first few injuries, and then the wave. I think I was working for 16 hours before Heather, the former head nurse, told me to leave before I passed out.
I just remember a big jumble. We had waves of people coming in before we were really aware of what we were up against. Someone actually brought out the disaster plan but it was kind of useless. Just a bunch of words abou
READ MORE >>
you should use the first four steps of the Socratic Problem-Solving Approach t ...
- Identify at least three scholarly or academic peer-reviewed journal articles about the topic.
- You may find the How Do I Find Peer-Reviewed Articles? library guide helpful in locating appropriate references.
- You may use articles you found while working on Assessment 2 or you may search the Capella library for other articles.
- You may find the applicable Undergraduate Library Research Guide helpful in your search.
- Review the Think Critically About Source Quality to help you complete the following:
- Assess the credibility of the information sources.
- Assess the relevance of the information sources.
- Analyze the health care problem or issue.
- Describe the setting or context for the problem or issue.
- Describe why the problem or issue is important to you.
- Identify groups of people affected by the problem or issue.
- Provide examples that support your analysis of the problem or issue.
- Discuss potential solutions for the health care problem or issue.
- Describe what would be required to implement a solution.
- Describe potential consequences of ignoring the problem or issue.
- Provide the pros and cons for one of the solutions you are proposing.
- Explain the ethical principles (Beneficence
READ MORE >>
NHS-FPX4000 Assessment 1 Developing a Health Care Perspective Case Study: To Vac ...
NHS-FPX4000 Assessment 1 Developing a Health Care Perspective Case Study: To Vaccinate or not Vaccinate Children Example Paper
Child vaccination is a widely accepted routine worldwide. However, there are ethical considerations that involve a balance between a parent’s right in allowing vaccination or their children and the benefits to public health emanating from vaccination of children. While healthcare givers are alive to the benefits of vaccination of children, they have to contend with the right of children to accept or refuse a vaccine.
It is the responsibility of health professionals to clarify to patients the merits they stand to gain from a vaccine and why it is necessary. For example, it is unethical and unreasonable to administer a vaccine to a child when they/their parents have no understanding of the vaccine. It is recommended that such health workers should explain to parents why their children a vaccine and what they stand to lose if their child does not get the jab.
Case Overview
The case scenario, dubbed incident 10 talks about the Smiths family and their five-year old daughter Ana. The Smith’s take their child Ana to their pediatrician to discuss whether or not to vaccinate their daughter. The Smiths’ were concerned about rising number of cases of autism in vaccinated children. They are concerned that vaccinating their child might result in autism-something they would want to avoid at all costs.
Both Ana’s mother and father have prior education/information regarding importance of child vaccination. They have also widely researched this issue through online search on blogs and other social media sites. Being a trained medical professional, Dr. Kerr listened keenly to the concerns presented to him by the Smiths ‘before giving his informed opinion/recommendation about the need to have children vaccinated.
Dr. Kerr told the Smiths’ that the consequences of not vaccinating a child are far too severe compared to vaccinating a child. According to Dr. Kerr, there is no study that directly confirms or link vaccination to autism. On the contrary, the Dr. informed the Smiths’ that there are studies that prove that there is no connection between autism spectrum disorder and vaccination.
Dr. Kerr informed the Smith family that the federal government keeps track of any and all adverse effects that may come from a vaccine. Through the Vaccine Adverse Event Reporting System, the government tracks all vaccines as well as get feedback from people about any incidence from a vaccine. The Dr. explained to the Smiths’ that growing hesitation, opposition and uncertainty about childhood vaccines has created a resurgence of cases of vaccine-preventable diseases and illnesses. In the end, despite Dr. Kerr’s efforts to educate the Smiths’ on the importance of child vaccination. The Smiths’ chose not to vaccinate their daughter.
Ethical Issues in the Case Study
In the case study provided, Dr. Kerr faces a big dilemma after the Smiths’ family refused to vaccinate their daughter. Dr. Kerr knows that the refusal of the Smiths’ to have their daughter Ana vaccinated based on negative rumors is bad for the child. By refusing to have their child vaccinated, the Smiths’ expose their child to dangerous diseases that are easily contained by a simple vaccination process. Refusal to vaccinate Ana exposes her to debilitating illnesses such as measles, mumps, polio, and meningitis.
Measles leads to swelling of the brain that can damage it and result in death while mumps can lead to permanent deafness. On its part, meningitis also leads to deafness and brain damage, while polio leads to permanent paralysis. These are some of the risks that the Smiths’ expose their daughter Ana by refusing to her get vaccinated. The Smiths’ are not only exposing their child to medical implications but also social implications such as exclusion and quarantine during disease outbreaks.
Ethical Decision-Making Model to Analyze the Case Study
Based on the Smith’s case study, moral judgment, moral behavior, and moral awareness are critical components of an ethical decision-making model. Concerning ethical awareness, the doctor, or any other healthcare professional faced with a similar situation must be alive to the existence of a dilemma. Regarding ethical judgment, the doctor must make the right judgments based on the situation at hand (Stenmark, et al., 2021). Ethical behavior is taking the right action to remedy the situation.
Based on the context of the Smiths’ family, it is incumbent upon Dr. Kerr to recognize that the Smiths’ family lack proper information and education regarding child vaccine. The Smiths’ are also not adequately aware of the risks they expose their daughter and other children by refusing to vaccinate Ana. The ethical behavior Dr. Kerr must adopt is to fully convince the Smiths’ to accept to have their daughter Ana vaccinated.
Effective Communication Approach
When she was presented with the problem, Dr. Kerr listened keenly and patiently to the Smiths’ as they narrated their dilemma. She listened all through out to how the Smiths’ arrived at the conclusion not to vaccinate their child Ana. Through active listening, Dr. Kerr was able to get the whole information from the Smiths’ and give them an informed response based on their dilemma.
Apart from keenly listening to the Smiths, Dr. Kerr also restrained herself from forcing or coercing Ana’s parent’s to get her vaccinated. This is a good professional behavior from the doctor because she knows that she has to respect a patient’s/client’s wishes and not imposing her own will on them even if she is right (Rainer et al., 2018).
Forcing or coercing the Smiths’ to have Ana vaccinated would have resulted in the exact opposite of her good intentions. For example, forceful vaccination or vaccinating Ana without her parent’s approval would have made the Smiths’ to lose faith in healthcare. Her approach of offering more information and education on child vaccine was more professional and bound to make the Smiths’ come to reason.
Applying Ethical Principles to Resolve Ethical Dilemma
The principles of autonomy, beneficence, nonmaleficence, and justice are key factors integral to resolving dilemmas when making decisions. Going by the case study of the Smiths’ family, Dr. Kerr clearly applied the principle of autonomy by giving the Smiths’ the opportunity to make their own decision after educating them and informing them of the consequences of not vaccinating their daughter.
Dr. Kerr also shows beneficence when she advises the Smiths to have their daughter vaccinated- her intentions are good for the patient. However, the Smiths’ action of refusing to have their daughter immunized despite having first-hand information from a qualified professional lacks beneficence as this action will harm their daughter. Concerning nonmaleficence, Dr. Kerr did not harm the patient in any way but to offer critical information that could save the life of Ana.
Conclusion
Healthcare professionals face situations of ethical dilemmas every day in their work. It is the responsibility of these healthcare professionals to know and understand the core principles of decision-making. Having understood the core principles of decision-making, the healthcare professionals must use them and apply them in making-critical decisions based on the conditions and situations faced by their patients/clients. The solutions offered must respect and observe the principles of autonomy, justice beneficence, and nonmaleficence.
References
Rainer, J., Schneider, J. K., & Lorenz, R. A. (2018). Ethical dilemmas in nursing: An integrative review. Journal of Clinical Nursing, 27(19-20), 3446-3461.
Stenmark, C. K., Redfearn, R. A., & Kreitler, C. M. (2021). Self-efficacy and ethical decision-making. Ethics & Behavior, 31(5), 301-320.
NHS-FPX4000 Assessment 1 Developing a Health Care Perspective
Develop a solution to a specific ethical dilemma faced by a health care professional by applying ethical principles. Describe the issues and a possible solution in a 3-5-page paper.
Introduction
Whether you are a nurse, a public health professional, a health care administrator, or in another role in the health care field, you must base your decisions on a set of ethical principles and values. Your decisions must be fair, equitable, and defensible. Each discipline has established a professional code of ethics to guide ethical behavior. In this assessment, you will practice working through an ethical dilemma as described in a case study. Your practice will help you develop a method for formulating ethical decisions.
Also Read:
NHS-FPX4000 Assessment 2
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
- Competency 1: Apply information literacy and library research skills to obtain scholarly information in the field of health care.
- Apply academic peer-reviewed journal articles relevant to an ethical problem or issue as evidence to support an analysis of the case.
- Competency 3: Apply ethical principles and academic standards to the study of health care.
- Summarize the facts in a case study and use the three components of an ethical decision-making model to analyze an ethical problem or issue and the factors that contributed to it.
- Discuss the effectiveness of the communication approaches present in a case study.
- Discuss the effectiveness of the approach used by a professional to deal with problems or issues involving ethical practice in a case study.
- Apply ethical principles to a possible solution to an ethical problem or issue described in a case study.
- Competency 4: Write for a specific audience, in appropriate tone and style, in accordance with Capella’s writing standards.
- Write clearly and logically, with correct use of spelling, grammar, punctuation, and mechanics.
- Write following APA style for in-text citations, quotes, and references.
NHS-FPX4000 Assessment 1 Developing a Health Care Perspective Instructions
Note: The requirements outlined below correspond to the grading criteria in the scoring guide. At a minimum, be sure to address each point. In addition, you are encouraged to review the performance-level descriptions for each criterion to see how your work will be assessed.
For this assessment, develop a solution to a specific ethical dilemma faced by a health care professional. In your assessment:
- Access the Ethical Case Studies media piece to review the case studies you will be using for this assessment.
- Select the case most closely related to your area of interest and use it to complete the assessment.
- Note: The case study may not supply all of the information you need. In such cases, you should consider a variety of possibilities and infer potential conclusions. However, please be sure to identify any assumptions or speculations you make.
- Include the selected case study in your reference list, using proper APA Style and Format.
- Select the case most closely related to your area of interest and use it to complete the assessment.
- Summarize the facts in a case study and use the three components of an ethical decision-making model to analyze an ethical problem or issue and the factors that contributed to it.
- Identify which case study you selected and briefly summarize the facts surrounding it. Identify the problem or issue that presents an ethical dilemma or challenge and describe that dilemma or challenge.
- Identify who is involved or affected by the ethical problem or issue.
- Access the Ethical Decision-Making Model media piece and use the three components of the ethical decision-making model (moral awareness, moral judgment, and ethical behavior) to analyze the ethical issues.
- Apply the three components outlined in the Ethical Decision-Making Model media.
- Analyze the factors that contributed to the ethical problem or issue identified in the case study.
- Describe the factors that contributed to the problem or issue and explain how they contributed.
- Apply academic peer-reviewed journal articles relevant to an ethical problem or issue as evidence to support an analysis of the case.
- In addition to the readings provided, use the Capella library to locate at least one academic peer-reviewed journal article relevant to the problem or issue that you can use to support your analysis of the situation. The How Do I Find Peer-Reviewed Articles? library guide will help you locate appropriate references.
- Cite and apply key principles from the journal article as evidence to support your critical thinking and analysis of the ethical problem or issue.
- Review the Think Critically About Source Quality
- Assess the credibility of the information source.
- Assess the relevance of the information source.
- In addition to the readings provided, use the Capella library to locate at least one academic peer-reviewed journal article relevant to the problem or issue that you can use to support your analysis of the situation. The How Do I Find Peer-Reviewed Articles? library guide will help you locate appropriate references.
- Discuss the effectiveness of the communication approaches present in a case study.
- Describe how the health care professional in the case study communicated with others.
- Assess instances where the professional communicated effectively or ineffectively.
- Explain which communication approaches should be used and which ones should be avoided.
- Describe the consequences of using effective and non-effective communication approaches.
- Discuss the effectiveness of the approach used by a professional to deal with problems or issues involving ethical practice in a case study.
- Describe the actions taken in response to the ethical dilemma or issue presented in the case study.
- Summarize how well the professional managed professional responsibilities and priorities to resolve the problem or issue in the case.
- Discuss the key lessons this case provides for health care professionals.
- Apply ethical principles to a possible solution to an ethical problem or issue described in a case study.
- Describe the proposed solution.
- Discuss how the approach makes this professional more effective or less effective in building relationships across disciplines within his or her organization.
- Discuss how likely it is the proposed solution will foster professional collaboration.
- Write clearly and logically, with correct use of spelling, grammar, punctuation, and mechanics.
- Apply the principles of effective composition.
- Determine the proper application of the rules of grammar and mechanics.
- Write using APA style for in-text citations, quotes, and references.
- Determine the proper application of APA formatting requirements and scholarly writing standards.
- Integrate information from outside sources into academic writing by appropriately quoting, paraphrasing, and summarizing, following APA style
NHS-FPX4000 Assessment 2 Capella
SOCRATIC PROBLEM SOLVING APPROACH https://campus.capella.edu/web/critical-thinking/b…
Create a 3-5-page annotated bibliography and summary based on your research related to best practices addressing a current health care problem or issue of interest to you.
In your professional life you will need to find credible evidence to support your decisions and your plans of action. You will want to keep abreast of best practices to help your organization adapt to the ever-changing health care environment.
Being adept at research will help you find the information you need. For this assessment, you will select and research a current health care problem or issue faced by a health care organization.
Demonstration of Proficiency
Instructions
Note: The requirements outlined below correspond to the grading criteria in the scoring guide. At a minimum, be sure to address each point. In addition, you are encouraged to review the performance level descriptions for each criterion to see how your work will be assessed.
For this assessment, you will research best practices related to a current health care problem. Your selected problem or issue will be utilized again in Assessment 3. To explore your chosen topic, you should use the first two steps of the Socratic Problem-Solving Approach to aid your critical thinking.
- View the Assessment Topic Areas| Transcript media piece and select one of the health care problems or issues in the media piece to research. Write a brief overview of the selected topic. In your overview:
- Describe the health care problem or issue.
- Describe your interest in the topic.
- Describe any professional experience you have with this topic.
- Conduct a search for scholarly or academic peer-reviewed literature related to the topic and describe the criteria you used to search for articles, including the names of the databases you used.
- You will want to access the applicable Undergraduate Library Research Guide related to your degree (found at the NHS Learner Success Lab) for tips to help you in your search.
- Use keywords related to the health care problem or issue you are researching to select relevant articles.
- Assess the credibility of the information sources you find.
- Determine if the source is from an academic peer-reviewed journal.
- Determine if the publication is current.
- Determine if information in the academic peer-reviewed journal article is still relevant.
- Select four current scholarly or academic peer-reviewed journal articles published during the past three to five years that relate to your topic.
- Explain the relevance of the information sources.
- Describe how the health care problem or issue is addressed in each source.
- Discuss what kind of contribution each source provides on your selected topic.
- Analyze the scholarly literature or academic peer-reviewed journal articles using the annotated bibliography organizational format.
- The purpose of an annotated bibliography is to document a list of references along with key information about each one. The detail about the reference is the annotation. Developing this annotated bibliography will create a foundation of knowledge about the selected topic.
- List the full reference for the source in APA format (author, date, title, publisher, et cetera) and use APA format for the annotated bibliography.
- Make sure the references are listed in alphabetical order, are double-spaced, and use hanging indents.
- Follow the reference with the annotation.
- In your annotation:
- Identify the purpose of the article.
- Summarize the source:
- What are the main arguments?
- What topics are covered?
- Include the conclusions and findings of the article.
- Write your annotation in a paragraph form. The annotation should be approximately 150 words (1 to 3 paragraphs) in length.
- In a separate paragraph or two at the end of the paper, summarize what you learned from your research.
- List the main points you learned from your research.
- Summarize the main contributions of the sources you chose and how they enhanced your knowledge about the topic.
Example Assessment: You may use the following to give you an idea of what a Proficient or higher rating on the scoring guide would look like:
- Assessment 2 Example [PDF].
Additional Requirements
- Length: At least 3–5 typed, double-spaced pages, not including the title page and reference page.
- Font and font size: Times New Roman, 12 point.
- APA Template: Use the APA template linked in the resources. Use the APA Style Paper Template [DOCX] as the paper format and the APA Style Paper Tutorial [DOCX] for guidance.
- Written communication: Write clearly and logically, with correct use of spelling, grammar, punctuation, and mechanics.
- Content: Provide a title page and reference page following APA style.
- References: Use at least four scholarly or academic peer-reviewed journal articles.
- APA format: Follow current APA guidelines for in-text citation of outside sources in the body of your paper and also on the reference page.
Note: Review the Applying Research Skills Scoring Guide for the grading criteria applied to this assessment.
NHS-FPX4000 Assessment 2 Topic Areas
Selecting a topic for your written assessments can be challenging, but it’s important to make a thoughtful choice.
Choose a topic area of interest to you from the topic suggestions in this media piece. You will use this topic to complete Assessments 2 and 3. Be sure to select a topic that will be manageable for a written assessment.
To explore the chosen topic, you should use the Socratic Problem-Solving Approach, focusing on the sections specifically called out in the assessment guidelines.
NHS-FPX4000 Topic 1: Limited Access to Healthcare
Short Description:
Consumers face barriers to healthcare access for assorted reasons. For example: due to geographic location, provider availability, transportation issues and mobility.
Potential Intervention Approaches:
- Healthcare information online
- Telemedicine
- In–home healthcare services
Keywords for Articles:
online health information seeking, health care access, health information systems, consumer health information, chronic disease, health information search, health seeking behavior, rural nursing
references:
Bhandari, N. (2014). Seeking health information online: does limited healthcare access matter? Journal of the American Medical Informatics Association: JAMIA (1067-5027), 21 (6), p. 1113. https://www-ncbi-nlm-nih-gov.library.capella.edu/pmc/articles/PMC4215038/
Lee, K., Hoti, K., Hughes, J. D., & Emmerton, L. (2014). Dr Google and the Consumer: A Qualitative Study Exploring the Navigational Needs and Online Health Information-Seeking Behaviors of Consumers with Chronic Health Conditions. Journal of Medical Internet Research, 16(12), e262. http://doi.org.library.capella.edu/10.2196/jmir.3706
Ware, P., Bartlett, S. J., Paré, G., Symeonidis, I., Tannenbaum, C., Bartlett, G., … Ahmed, S. (2017). Using eHealth Technologies: Interests, Preferences, and Concerns of Older Adults. Interactive Journal of Medical Research, 6(1), e3. http://doi.org.library.capella.edu/10.2196/ijmr.4447
Pratt, D. (2015). Telehealth and telemedicine. Albany Law Journal of Science & Technology. (1059-4280), 25 (3), p. 495. http://www.lexisnexis.com.library.capella.edu/hottopics/lnacademic/?shr=t&csi=148364&sr=TITLE(%22Telehealth+telemedicine+in+2015%22)+and+date+is+2015
Topic 2: Healthcare Disparities
Short Description:
In 2010, the Federal Department of Human and Health Service (DHHS) launched the Healthy People 2020 goals to include a goal to eliminate health inequality/disparity.
Healthy People 2020 defines a health disparity as “a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage.
Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; gender; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity;
geographic location; or other characteristics historically linked to discrimination or exclusion” (Office of Disease Prevention and Health Promotion, 2017, p.1).
Potential Intervention Approaches:
- Federal goals
- Community health improvement plans
- Patient advocacy efforts
- “Triple Aim” for populations
Keywords for Articles:
health disparities, community health assessment, community health improvement plan, strategic planning, local health departments, health inequities
References:
Office of Disease Prevention and Health Promotion. (2017). Disparities. Retrieved from https://www.healthypeople.gov/2020/about/foundation-health-measures/disparities
Shah G.H., & Sheahan J.P. (2016). Local health departments’ activities to address health disparities and inequities: Are we moving in the right direction? International Journal of Environmental Research and Public Health. 2016; 13(1):44. http://www.mdpi.com/1660-4601/13/1/44
Institute for Healthcare Improvement. (2017). Triple Aim for Populations. http://www.ihi.org/Topics/TripleAim/Pages/Overview.aspx
NHS-FPX4000 Assessment 2 Topic 3: Medication Errors
Short Description:
A medication error is a preventable adverse effect of a patient taking the wrong medication or dosage, whether or not it is evident or harmful to the patient. Medication errors can be a source of serious patient harm, including death.
Potential Intervention Approaches:
- Medical staff education
- Packaging improvements
- Patient medication safety training
Keywords for Articles:
medication administration, medication errors, medication safety
References:

Cohen, M. (2016). Medication errors (miscellaneous). Nursing. 46(2):72, February 2016. DOI: 10.1097/01.NURSE.0000476239.09094.06
Institute for Healthcare Improvement. (2017). Improve Core Processes for Administering Medications. http://www.ihi.org/resources/Pages/Changes/ImproveCoreProcessesforAdministeringMedications.aspx
Agency for Healthcare Research and Quality. (2012). Table 6: Categories of Medication Error Classification. http://www.ahrq.gov/professionals/quality-patient-safety/patient-safety-resources/resources/match/matchtab6.html
Schmidt, K., Taylor, A., & Pearson, A. (2017). Reduction of medication errors: A unique approach. Journal of Nursing Care Quality. 32(2), April/June 2017, 150–156.
NHS-FPX4000 Assessment 2 Topic 4: Healthcare System Errors
Short Description:
The health care system in the United States has been the subject of much debate as experts try to determine the best way to deliver high-quality care.
In Crossing the Quality Chasm, the Institute of Medicine (2001) called for the redesign of health care delivery systems and their external environments to promote care that is safe, effective, patient-centered, timely, efficient, and equitable.
Potential Intervention Approaches:
- Systemwide transformation
- Process redesign
- Electronic health records
Keywords for Articles:
multi-stakeholder collaboration, healthcare system redesign
References:
Institute of Medicine (US) Committee on Quality of Health Care in America. (2001). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US).Agency for Healthcare Research and Quality.
(2017). Hospitals and Health Systems. http://www.ahrq.gov/professionals/systems/index.html
Roberts, B. (2017). Relationship-based care: The institute of medicine’s core competencies in action. Creative Nursing, 05/2016, 22(2).
Credits
- Subject Matter Expert: Joan Vermillion
- Interactive Design: Lori Olson
- Media Instructional Design: Felicity Pearson
- Instructional Design: Celina Byers
- Project Manager: Alan Campbell
Resources: Research and Annotated Bibliographies
Top of Form
Bottom of Form
Content
- How do you approach a problem or issue within your organization? How often do you need credible information to solve a personal or professional problem? Credible information is information that is trustworthy.
- One of the best sources for credible information is the professional literature of the field you are studying; in your case, health care.
- Professional literature is research that has been written and reviewed by other people in your field.
The following resources can help you as you complete your research and seek out professional literature on a health care topic.
- Gennaro, S. (2016). Why write? Journal of Nursing Scholarship, 48(2), 117.
- National Institutes of Health, U.S. National Library of Medicine. (2017). Evidence-based practice and health technology assessment. Retrieved from https://www.nlm.nih.gov/hsrinfo/evidence_based_practice.html
- Rollins, J. A. (2017). Healthcare: It’s “so complicated.” Pediatric Nursing, 43(2), 58, 102.
Each of the following Research Guides is written with a specific program in mind. The one for your program can provide insights about researching topics related to your field.
- Nursing (BSN) Library Research Guide.
- Public Health Undergraduate Library Research Guide.
- Health Care Administration Undergraduate Library Research Guide.
The following resources provide specific information about annotated bibliographies.
- What Not To Do: Source Material for the Annotated Bibliography | Transcript.
- Sample Annotated Bibliography [PDF].
NHS-FPX4000 Assessment 3 Analyzing a Current Healthcare Problem or Issue Instructions
- Write a 4-6 page analysis of a current problem or issue in health care, including a proposed solution and possible ethical implications.
Introduction
In your health care career, you will be confronted with many problems that dema
READ MORE >>
