Our Previous Samples
Annotated Bibliography on Acute Asthma Management SampleIntroductionSevere acute ...
Annotated Bibliography on Acute Asthma Management Sample
Introduction
Severe acute asthma is a clinical emergency that can easily be managed by various clinical therapies. However, if poorly managed, it can invariably lead to death by cardiorespiratory collapse. Typically, therapeutic management of severe asthma targets to increase air passage through bronchodilators dilation and oxygen supplementation. Ultimately, these therapies should stabilize the patient.
The available treatment options for children with severe acute asthma refractory to SAMA/LAMA combination are limited because the remaining ones are either not safe or are expensive. Nonetheless, the patients must the treated and therefore alternatives such as IV steroids with or without heliox are often used as the most feasible options. Against this backdrop, there are various pieces of research evidence that have confirmed the role of IV methylprednisolone as well as that of heliox in improving severe asthma. However, evidence on the latter is a bit controversial due to its side effects and availability. The current study seeks to unravel the available evidence on the use of IV methylprednisolone or a combination of IV methylprednisolone and heliox in the treatment of severe acute asthma in children between the age of 5-15 years old.
The study takes the form of an annotated bibliography; evaluating the quality of evidence in 8 peer reviewed journal articles. The review will summarize the content of each journal article in terms of its purpose, findings and implications of those findings to the management of severe acute asthma. It is worth noting that all the journal articles have been published within the past five years.
Article 1
Henderson, M. B., Schunk, J. E., Henderson, J. L., Larsen, G. Y., Wilkes, J., & Bratton, S. L.
(2018). An assessment of asthma therapy in the pediatric ICU. Hospital pediatrics, 8(6), 361-367. DOI: https://doi.org/10.1542/hpeds.2017-0003
Henderson et al. (2017) argue that asthma is one of the most common chronic respiratory condition in children affecting millions of children and continues to be a common cause of Intensive Care Unit (ICU) admission. Bearing this in mind, the authors conducted a study on asthma therapy in pediatric ICU, describing asthma management, evaluating practice evaluation, and describing the resource use during asthma management at the pediatric ICU.
Being a retrospective study single-center cohort study, it involved 262 children of age 2 to 18 years in pediatric ICU treated with asthma from 2008 to 201;1 with data collected through intermountain Healthcare Enterprise Data Warehouse. Majority of the participants only received only the first tier of recommended therapy (inhaled short-acting b-agonists, pre-hopsitalization inhaled ipratropium bromide, systemic corticosteroids and oxygen), while 70% of them did not receive any further respiratory support beyond non-breather mask or nasal cannula mask including inhaled nitric oxide, IV b-agonists, intravenous (IV) magnesium sulfate, inhaled heliox. While heliox were rarely used before or after pediatric ICU, no adverse event was reported on its use.
The study results indicated that most of the patients with severe asthma were treated with only the minimum interventions (i.e. first-tier medication, none-breather or nasal canular mask). These treatments minimized the pediatric ICU length of stay and thus reduced expenses involved in asthma care. these findings confirm that heliox can be used as a treatment therapy for asthma in pediatric ICU with no side effects. Its methodology was effective, and the resultant evidence can be useful in comparing the use of heliox versus the use of a combination of heliox and IV methylprednisolone.
However, the fact that this study was a single-hospital cohort study limits the generalization of its findings. Furthermore, the generalization of the study finding is also limited by the fact that it did not consider specific factors such as patient ethnicity, which was not a representative of the US population.
Article 2
Doymaz, S., Ahmed, Y. E., Francois, D., Pinto, R., Gist, R., Steinberg, M., & Giambruno, C.
(2020). Methylprednisolone, dexamethasone or hydrocortisone for acute severe pediatric asthma: does it matter?. Journal of Asthma, 1-10. https://doi.org/10.1080/02770903.2020.1870130
The study by Doymaz et al. (2020) was inspired by the statistics that asthma is a chronic
childhood illness that affects at least 6 million children and by 2017, it was responsible for 863 per every 100,000 deaths in the United States. Furthermore, the authors were motivated by the fact that whereas various intravenous IV corticosteroids are available of the treatment of acute severe asthma, the choice of IV corticosteroids largely depends on physician’s preferences or institution. Against this background, the researchers conducted a study to compare the efficacy of IV methylprednisolone, dexamethasone and hydrocortisone during pediatric ICU admission.
The study took the form of a randomized clinical trial that enrolled patients of 1-12 years old requiring continuous beta-2 agonist treatment.
The randomization was done in three groups: IV Dexamethasone group, IV Hydrocortisone and IV Methylprednisolone. The researchers measured primary outcomes based on durations of beta-2 agonist continuous nebulization treatment. On the other hand, the secondary outcomes were measured by pediatric asthma severity score, maximum dose of beta-2 agonist treatment, need for mechanic ventilation and pediatric ICU and hospital length of stay.
The study findings indicated no difference in efficacy of dexamethasone, hydrocortisone and IV methylprednisolone when used in appropriate doses to treat pediatric asthma. This was demonstrated by a no difference in the various outcome measurements such as B2 agonist maximum dose, pediatric asthma severity score, pediatric ICU length of stay and need for mechanic ventilation. While the generalization of these study findings is affected by the small sample cohort, it produces useful evidence to support the use of IV methylprednisolone in the management of pediatric severe asthma.
Article 3
Fishe, J. N., Gautam, S., Hendry, P., Blake, K. V., & Hendeles, L. (2019a). Emergency medical services administration of systemic corticosteroids for pediatric asthma: A statewide study of emergency department outcomes. Academic Emergency Medicine, 26(5), 549-551. https://doi.org/10.1111/acem.13660
Systemic corticosteroids have always been administered to children with asthma admitted in the emergency department with the aim of reducing their length of stay. However, as per Fishe et al. (2019a), there is a paucity of research examining the improvement effect of corticosteroids on patient outcomes. In response, the researchers conducted a state-wide study to investigate the emergency department outcomes upon the use of corticosteroids on paediatric asthma.
The retrospective observational cohort study relied on patients whose records remained in Florida’s EMS Tracking and Reporting System with information on emergency department’s outcome of patients between 2011 – 2016. The inclusion criteria were children of age 2-18 admitted in the emergency department with respiratory distress, whose acute asthma exacerbation was indicated by their receipt of albuterol. The study found that the administration of IV methylprednisolone was associated with decreased odds of emergency department discharge. Fishe et al. (2019a) attributed these results to a few reasons. For instance, IV methylprednisolone was only reserved for patients with more severe asthma.
The findings of this study are especially useful in understanding not only the effects of IV methylprednisolone as an emergency department intervention for severe asthma in children, but also the role of severity as a factor to consider when using IV methylprednisolone on pediatric asthma. Nonetheless, this study had several methodological limitations that must be pointed out. For instance, the study only focused on one state and this affects its generalizability to other areas of the United States. Furthermore, only on third of the patients had identifiable emergency department outcomes. More importantly, the researchers did not have any prior knowledge of any medications the patients had taken before their arrival at the emergency departments, affecting validity of the study.
Article 4
Fishe, J. N., Palmer, E., Finlay, E., Smotherman, C., Gautam, S., Hendry, P., & Hendeles, L.
(2019). A statewide study of the epidemiology of emergency medical services’ management of pediatric asthma. Pediatric Emergency Care. doi: 10.1097/PEC.0000000000001743
Fishe et al. (2019b) argued that at least ten percent of all pediatric emergency department patients use emergency medical services for transport and prehospital management. While studies show that the most frequently used medication was albuterol, there is a paucity of research evidence on pediatric emergency medical services experiences with respiratory distress or asthma. Therefore, the researchers set out to investigate the relevant clinical, geographic, demographic and characteristics of pediatric asthma treated in the emergency medical services in a state with the fourth-largest pediatric population to examine the current emergency medical services treatment practices.
The retrospective observational cohort study relied on patients whose records remained in Florida’s EMS Tracking and Reporting System with information on emergency department’s outcome of patients between 2011 – 2016. The inclusion criteria were children of age 2-18 admitted in the emergency department with respiratory distress, whose acute asthma exacerbation was indicated by their receipt of albuterol. The study found that in practice, IV methylprednisolone is reserved for the small percent of patients with generally more severe asthma. However, they are more liberally administered in the emergency department because they are of benefit to those with moderate and severe asthma exacerbations.
These findings are important to the study of IV methylprednisolone as a treatment therapy for pediatric asthma in the emergency department because it explores the general practice and how IV methylprednisolone is used. However, it has several methodological limitations that limits its generalizability. For instance, the study only focused on one state and this affects its generalizability to other areas of the United States. Furthermore, the EMS Tracking and Reporting System does not distinguish ground versus air transport, and therefore some emergency medical service users might have been omitted.
Article 5
Leung, J. S. (2021). Paediatrics: how to manage acute asthma exacerbations. Drugs in Context,
- 10. doi: 7573/dic.2020-12-7
Leung (2020) considers asthmas one of the most common chronic illnesses in children and a major contributor of child death globally. As such, the researcher conducted a review of literature to investigate the various medications used in treating acute asthma exacerbations and their efficacy. The review presented the evidence in the context of a stepwise management of acute asthma exacerbations and provided several recommendations for practice based on his findings.
The study found that in children, IV methylprednisolone is a recommended oral medication that may however be safe due to concerns associated with vomiting. Furthermore, Leung (2020) observed that there is a paucity of data supporting that IV methylprednisolone can provide additional efficacy benefits over other oral formulas. Furthermore, the study did not find any evidence of increased intramuscular corticosteroids have better benefits that oral corticosteroids.
The findings of this study are useful in having a better understanding of IV methylprednisolone as a corticosteroid used to treat acute asthma exacerbations. It compares IV methylprednisolone with other therapies to give a better comparison of evidence on the treatment of acute asthma exacerbations in children. However, because the study relied on secondary data, the generalizability of study is affected by the literature search and selection bias.
Article 6
Batabyal, R. A., & O’Connell, K. (2018). Improving Management of Severe Asthma: BiPAP and
Beyond. Clinical Pediatric Emergency Medicine, 19(1), 69-75. https://doi.org/10.1016/j.cpem.2018.02.007
Pediatric emergency departments encounter unique challenges with acute asthma exacerbations. Whereas most children respond well to treatments such as systemic corticosteroids, ipratropium, and inhaled ?2-agonists, some children may require adjunct treatments. As such, Batabyal and O’Connell (2018) conducted a literature review study to investigate the various guidelines on the management of severe asthma exacerbations in pediatric emergency departments.
The review covers both the use of heliox as well as the use of Corticosteroids such as IV methylprednisolone. Reviewed evidence indicate that early use of IV methylprednisolone is important and even a slight delay can increase the chances of hospital admission. Another important finding of this review is that whereas one would want to administer more doses of IV methylprednisolone to mitigate inflammation, there is no evidence supporting greater doses of more than 2mg/kg even in the case of acute asthma; and therefore, higher doses is not recommended.
On heliox, the study revealed variable efficacy of heliox as a therapy for acute severe asthma exacerbations among the Pediatric population. However, the reviewed evidence also shows that some guidelines (e.g. NAEPP) recommend the administration of inhaled beta agonists with heliox in patients whose asthma exacerbations is life threatening. Similarly, as per Batabyal and O’Connell (2018), the GINA guidelines recommend heliox for acute severe asthma for patients who do not respond to conventional treatment.
Practice guidelines are integral part of evidence-based practice because they reveal the generally accepted practices backed by evidence. As such, the study by Batabyal and O’Connell (2018) is useful in studying the use of IV methylprednisolone and or heliox in the management of acute severe asthma in children because it compares various guidelines on the same. However, the study is limited by the fact that it relies on secondary material, which is susceptible to selection and inclusion bias.
Article 7
Indinnimeo, L., Chiappini, E., & Del Giudice, M. M. (2018). Guideline on management of the
acute asthma attack in children by Italian Society of Pediatrics. Italian Journal of Pediatrics, 44(1), 1-10. https://doi.org/10.1186/s13052-018-0481-1
Indinnimeo et al. (2018) opined that it is important to deliver appropriate care to children with asthma considering its life-threatening risk and its high prevalence on children. In the spirit of evidence-based practice, they conducted a study to guide the management of asthma attack in children. The study relied on Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. They also conducted a literature search on Cochrane library to retrieve Italian journal articles on children of age 2 years and above.
One of the most relevant recommendation given by Indinnimeo et al. (2018) is that heloix can be given to children with life-threatening asthma attack, especially for those not responding to alternative treatment. The study further explained that heloix can improve ventilation and reduce respiratory failure in patients experiencing airway obstruction. This study gives important insights that are useful in answering some of the background questions of the study such as those concerning the therapeutic options of severe asthma.
Article 8
Seliem, W., & Sultan, A. M. (2018). Heliox delivered by high flow nasal cannula improves
oxygenation in infants with respiratory syncytial virus acute bronchiolitis?. Jornal de Pediatria, 94, 56-61. https://doi.org/10.1016/j.jped.2017.04.004
The study by Seliem & Sultan (2018) evaluates how heliox delivered through high flow nasal canula can improve oxygenation in children with respiratory syncytial virus acute bronchitis/asthma. It took the design of a randomized control trial that included 48 patients. The treatment group received heliox (70:30) while the control group received air-oxygen mixture through high flow nasal cannula at 8 L per minute continuously for 24 hours. After two hours of treatment with heliox, the treatment group registered a more significant improvement compared to the control group of 98.3% versus 92.9% respectively.
Seliem & Sultan (2017) concluded that transient improvement of oxygenation can be achieved in children with respiratory syncytial virus acute bronchitis if heliox is used so that other therapeutic agents can find more time to work on the disease and resolve it naturally. However, this study has a few limitations. First, the randomization was not blinded due to an existing discrepancy between the delivery systems of both gases. Furthermore, the small sample size hindered discrimination between clinical phenotypes based on chest radiology.
References
- Batabyal, R. A., & O’Connell, K. (2018). Improving Management of Severe Asthma: BiPAP and Beyond. Clinical Pediatric Emergency Medicine, 19(1), 69-75. https://doi.org/10.1016/j.cpem.2018.02.007
- Doymaz, S., Ahmed, Y. E., Francois, D., Pinto, R., Gist, R., Steinberg, M., & Giambruno, C. (2020). Methylprednisolone, dexamethasone or hydrocortisone for acute severe pediatric asthma: does it matter?. Journal of Asthma, 1-10. https://doi.org/10.1080/02770903.2020.1870130
- Fishe, J. N., Gautam, S., Hendry, P., Blake, K. V., & Hendeles, L. (2019a). Emergency medical services administration of systemic corticosteroids for pediatric asthma: A statewide study of emergency department outcomes. Academic Emergency Medicine, 26(5), 549-551. https://doi.org/10.1111/acem.13660
- Fishe, J. N., Palmer, E., Finlay, E., Smotherman, C., Gautam, S., Hendry, P., & Hendeles, L. (2019b). A statewide study of the epidemiology of emergency medical services’ management of pediatric asthma. Pediatric emergency care. doi: 10.1097/PEC.0000000000001743
- Henderson, M. B., Schunk, J. E., Henderson, J. L., Larsen, G. Y., Wilkes, J., & Bratton, S. L. (2018). An assessment of asthma therapy in the pediatric ICU. Hospital pediatrics, 8(6), 361-367. DOI: https://doi.org/10.1542/hpeds.2017-0003
- Indinnimeo, L., Chiappini, E., & Del Giudice, M. M. (2018). Guideline on management of the acute asthma attack in children by Italian Society of Pediatrics. Italian Journal of Pediatrics, 44(1), 1-10. https://doi.org/10.1186/s13052-018-0481-1
- Leung, J. S. (2021). Paediatrics: how to manage acute asthma exacerbations. Drugs in Context, 10. doi: 10.7573/dic.2020-12-7
- Seliem, W., & Sultan, A. M. (2018). Heliox delivered by high flow nasal cannula improves oxygenation in infants with respiratory syncytial virus acute bronchiolitis?. Jornal de pediatria, 94, 56-61. https://doi.org/10.1016/j.jped.2017.04.004
READ MORE >>
Ankle Pain Discussion ResponsesDiscussion ResponsesHello Olugemo, I have gone th ...
Ankle Pain Discussion Responses
Discussion Responses
Hello Olugemo, I have gone through your post on ankle pain concerning your case study of F. F., a 46-year-old female who presented with bilateral ankle pains and here are responses. You explored the ankle pain very well in your history but don’t you think knowing if the pain is radiating, its relieving factors and the timing (if it is constant or intermittent) would have been an important part of your pain history. Still in your history it would be of significance to rule out history of complicating conditions of ankle injury such as diabetes, arthritis and connective tissue disorders.
Your evaluation of the patient in terms of physical assessment was well done as it confirmed that the right ankle was severely injured compared to the left. The presence of ecchymosis and a higher pain grading scale on the right all support this. The ankle is prone to injury because of its complexity. The injuries range from ankle ligament injuries to fractures to fracture subluxation and dislocation. Grade I and II ankle injuries cause stretching or microscopic tears of the stabilizing ligaments while Grade III ankle sprain may interfere with syndesmotic structures. Moreover, the highest energy incidents may disrupt the tendons and cause fractures. With ankle sprain the most commonly involved structure is anterior talofibular ligament and or calcaneofibular ligament (Melanson & Shuman, 2020).
Information about the diagnostic tests such as the need for X-ray and specific evaluations for ankle injury were well captured. In addition, it would have been necessary to do a Kleiger test to rule out injury to the deltoid ligament (Larkins, Baker & Baker J., 2020) and inversion stress maneuver to assess the integrity of calcaneofibular ligament. Am also in agreement with your assessment differential diagnosis as F.F is likely to have bilateral lateral ankle sprains based on her presentation, Further, it appears that her ankles were forcefully rolled out of their normal position during the exercise, hence stretching them. Generally, your diagnostic formulation was fine all the way from history to differential diagnosis. Thank you.
References.
- Larkins, L. W., Baker, R. T., & Baker, J. G. (2020). Physical examination of the ankle: A review of the original orthopedic special test description and scientific validity of common tests for ankle examination. Archives of Rehabilitation Research and Clinical Translation, 2(3), 100072. https://doi.org/10.1016/j.arrct.2020.100072
- Melanson, S. W., & Shuman, V. L. (2020). Acute ankle sprain. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK459212/
READ MORE >>
Application of Theory Paper NR501Application of Theory Paper NR501Guidelines &am ...
Application of Theory Paper NR501
Application of Theory Paper NR501
Guidelines & Scoring Rubric
Purpose:
The purpose of this assignment is to synthesize one strategy for the application of a specific nursing theory to resolving a problem or issue of nursing practice in nursing leadership, nursing education, nursing informatics, or health policy.
Course Outcomes
Through this assignment, a student will demonstrate the ability to:
(CO#1) Analyze theories from nursing and relevant fields with respect to their components, relationships among the components, logic of the propositions, comprehensiveness, and utility to advanced nursing. (PO1)
(CO#3) Communicate the analysis of and proposed strategies for the use of a theory in nursing practice. (PO3, 7, 10)
(CO#4) Demonstrate logical and creative thinking in the analysis and application of a theory to nursing practice. (PO4, 7)
Due Date: Sunday 11:59 PM MT at the end of Week 6
Total Points Possible: 325
Also Read:
Chamberlain NR501 Jean Watsons Theory of Human Caring Presentation
Requirements:
Description of the Assignment:
Content
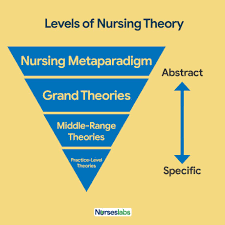
- Introduction to the paper includes a few general statements on the idea of nursing theory being applied to solve problems/issues in nursing practice, regardless of the specialty area of practice. For example, why would one pick a nursing theory to solve a practice problem? Would a grand, middle-range, or practice theory be best? Does the writer have any experience in using nursing theory this way? In addition, a brief one-paragraph summary of a specific nursing theory and information on the sections of the paper are provided. The selected nursing theory can be a grand theory, a middle-range theory, or a practice theory.
- Description of the problem/issue for which strategies will be developed. The problem to be resolved must be in nursing leadership, nursing education, nursing informatics, or health policy. Scholarly evidence (in the form of a literature review) supporting the issue is included. The problem/issue could be local to one’s specific practice setting. For example, the setting might be a nursing unit, a nursing-education program, an informatics department, or a health-policy unit of a consulting firm. The problem/issue needs to be something that a nursing theory can impact, whether it solves the actual problem/issue or enables people affected by the problem/issue to deal with it. It is best if the problem/issue is from real life – something the writer of the paper has dealt with or is currently engaged in.
Some examples (these are fictitious examples)
- A nursing unit has experienced rapid turnover of professional staff, including several nurse managers. A new nurse manager from outside of the nursing unit is appointed.
- Informatics nurse specialists face a lot of resistance from all healthcare professionals to implementation of a computer-based order entry program. The implementation date will not be changed.
- A nurse educator is assigned to take over a large class of undergraduate nursing students, with a mix of young adults and adults returning for a second degree. The subject is difficult, students have not been doing well, and frustration and tempers are impeding group work.
- A health-policy nurse specialist works for a consulting firm that lobbies on behalf of many healthcare professions. Within the specialist’s work unit, there is much debate over the pros and cons of various policies being proposed for attention in the coming year.
- Applying concepts and principles from the selected theory, one strategy for resolving the identified issue is described in depth. Details on how the theory would be applied are included (consider: who, what, when, where, and how). Rationales for the strategy as well as evidence from scholarly literature are included. One ethical and/or legal aspect of the strategy is discussed. Expected outcome(s) from implementing the strategy are proposed.
- Concluding statements include new knowledge about applying nursing theory gained by writing the paper
Format and Special Instructions
- Paper length: 6 pages minimum; 8 pages maximum, excluding title page and reference page. Points will be deducted for not meeting these requirements.
- The textbook required for this course may not be used as a reference for this assignment.
- A minimum of 3 scholarly references are used. References must be current – no older than 5 years, unless a valid rationale is provided. Consult with the course instructor about using an older source.
- Title page, body of paper, and reference page(s) must be in APA format as presented in the 6th edition of the manual
- Ideas and information from readings and other sources must be cited and cited correctly.
- Grammar, spelling, punctuation, and citations are consistent with formal academic writing as presented in the 6th edition of the APA manual
References
Carper, B.A. (1978). Fundamental patterns of knowing in nursing. Retrieved 8 September 2019 from
https://www.google.co.ke/url?sa=t&source=web&rct=j&url=https://pdfs.semanticscholar.org/8871/eb88fb06168bb31e20e9c54e57920e575a47.pdf&ved=2ahUKEwje0JrqscHkAhVClFwKHYXzAgsQFjAQegQICRAB&usg=AOvVaw0CEuuz-eqnIwVMqcmUI55E
Haswell, N. (2019). The four ethical principles and their application in aesthetic practice. Journal of Aesthetic Nursing, 8(4), 177-179. Doi: 10.12968/joan.2019.8.4.177
Schmidt, L.A., Nelson, D. & Godfrey, L. (2003). A clinical ladder program based on Carper’s fundamental patterns of knowing in nursing. JONA, 33(3), 146-152. Doi: 10.1097/00005110-200303000-00005
Quaglietti, S., Blum, L. & Ellis, V. (2004). The role of the adult nurse practitioner in palliative care. Journal of Hospice and Palliative Nursing, 6(4), 209-214. Doi: 10.1097/00129191-200410000-00009
Directions and Grading Criteria
CategoryPoints%DescriptionIntroduction6019Introduction to the paper includes all of the following:· General statements on the idea of nursing theory being applied to solve problems/ issues in nursing practice, regardless of the specialty area of practice.
· A brief one-paragraph summary of a specific nursing theory
· Information on the sections of the paper
Problem/ Issue8526The problem/issue is substantively discussed.
The problem is clearly in nursing leadership, nursing education, nursing informatics, or health policy.
Scholarly evidence supporting the issue is included.
Strategy10030All of the following are present:
· One strategy for resolving the identified issue is discussed substantively
·;
· Rationale(s) for the strategy are evident
· Evidence from the scholarly literature supports the discussion
· At least one ethical and/or legal aspect of the strategy is discussed.
Conclusion4013Concluding paragraph(s) clearly show new knowledge about applying nursing theory gained from writing this paperPaper Requirements103All of the following requirements are met:
Paper meets length requirements
Minimum of 3 scholarly references
Textbook not used as a reference
References are current – within a 5-year time frame unless a valid rationale is provided for use of older references
APA Format103Title page, body of paper, and reference page must follow APA guidelines as found in the 6th edition of the manual. This includes the use of headings for each section or topic of the paper.Citations in Text103Ideas and information that come from readings must be cited and referenced correctly.Writing Mechanics103Rules of grammar, spelling, word usage, and punctuation are followed and consistent with formal written work as found in the 6th edition of the APA manual.Total 325100A quality assignment will meet or exceed all of the above requirements.
Grading Rubric
Assignment CriteriaA(100 – 92%)
Outstanding or highest level of performance
B(91-84%)
Very good or high level of performance
C(83-76%)
Competent or satisfactory level of performance
F(75-0%)
Poor or failing or unsatisfactory level of performance
ContentPossible Points = 285 Points
Introduction60-56 Points55-50 Points49-46 Points45-0 PointsIntroduction to the paper includes all of the following:
· General statements on the idea of nursing theory being applied to solve problems/ issues in nursing practice, regardless of the specialty area of practice.
· A brief one-paragraph summary of a specific nursing theory
· Information on the sections of the paper
Introduction to the paper includes only 2 of the following:· General statements on the idea of nursing theory being applied to solve problems/issues in nursing practice, regardless of the specialty area of practice.
· A brief one-paragraph summary of a specific nursing theory
· Information on the sections of the paper
Introduction to the paper includes only 1 of the following:· General statements on the idea of nursing theory being applied to solve problems/issues in nursing practice, regardless of the specialty area of practice.
· A brief one-paragraph summary of a specific nursing theory
· Information on the sections of the paper.
Introduction to the paper includes none of the following:· General statements on the idea of nursing theory being applied to solve problems/issues in nursing practice, regardless of the specialty area of practice.
· A brief one-paragraph summary of a specific nursing theory
· Information on the sections of the paper
Problem/Issue85-78 Points77-71 Points70-65 Points64-0 PointsThe problem/issue is substantively discussed.
The problem is clearly in nursing leadership, nursing education, nursing informatics, or health policy.
Scholarly evidence supporting the issue is included.
The problem/issue is superficially discussed.
The problem is clearly in nursing leadership, nursing education, nursing informatics, or health policy.
Scholarly evidence supporting the issue is included
The problem/issue is superficially discussed.
· It is not clear if the problem belongs to nursing leadership, nursing education, nursing informatics, or health policy
OR
· Scholarly evidence supporting the issue is not included
The problem/issue is superficially discussed.
· It is not clear if the problem belongs to nursing leadership, nursing education, nursing informatics, or health policy
AND
· Scholarly evidence supporting the issue is not included
Strategy100-92 Points91-84 Points83-76 Points75-0 PointsAll of the following are present:
· One strategy for resolving the identified issue is discussed substantively
·;
· Rationale(s) for the strategy are evident
· Evidence from the scholarly literature supports the discussion
· At least one ethical and/or legal aspect of the strategy is discussed.
Only 4 of the following are present:
· One strategy for resolving the identified issue is discussed substantively
· Concepts and principles from the selected nursing theory are clearly applied
· Rationale(s) for the strategy are evident
· Evidence from the scholarly literature supports the discussion
· At least one ethical and/or legal aspect of the strategy is discussed
Only 3 of the following are present:
· One strategy for resolving the identified issue is discussed substantively
· Concepts and principles from the selected nursing theory are clearly applied
· Rationale(s) for the strategy are evident
· Evidence from the scholarly literature supports the discussion
· At least one ethical and/or legal aspect of the strategy is discussed
2 or fewer of the following are present:
· One strategy for resolving the identified issue is discussed substantively
· Concepts and principles from the selected nursing theory are clearly applied
· Rationale(s) for the strategy are evident
· Evidence from the scholarly literature supports the discussion
· At least one ethical and/or legal aspect of the strategy is discussed
Conclusion40-37 Points 33-30 Points29-0 PointsConcluding paragraph(s) clearly show new knowledge about applying nursing theory gained from writing this paperNAConcluding paragraph(s) does not clearly show new knowledge about applying nursing theory gained from writing this paper
Concluding paragraph(s) are missing
Content Subtotal _____of 285 pointsFormat
Possible Points = 40 Points
Paper Requirements10-9 Points8 Points7 Points6-0 PointsAll of the following requirements are met:
Paper meets length requirements
Minimum of 3 scholarly references
Textbook not used as a reference
References are current – within a 5-year time frame unless a valid rationale is provided for use of older references
Only 2 of the following requirements are met:
Paper meets length requirements
Minimum of 3 scholarly references
Textbook not used as a reference
References are current – within the 5-year time frame unless a valid rationale is provided for use of older references
Only 1 of the following requirements is met:
Paper meets length requirements
Minimum of 3 scholarly references
Textbook not used as a reference
References are current – within the 5-year time frame unless a valid rationale is provided for use of older references
None of the following requirements are met:
Paper meets length requirements
Minimum of 3 scholarly references
Textbook not used as a reference
References are current – within the 5-year time frame unless a valid rationale is provided for use of older references
APA Format10-9 Points8 Points7 Points6-0 PointsThere are 0 – 2 APA format errors in the text, title page and reference page(s)There are 3 – 5 APA format errors in the text, title page and/or reference page(s)There are 6 – 8 APA format errors in the title page, running head, or reference page (s).There are 9 or more APA format errors in the title page, running head, or reference pages(s).Citations10-9 Points8 Points7 Points6-0 PointsThere are 0-2 errors in the citation of ideas and information
There are 3-5 errors in the citation of ideas and informationThere are 6 – 8 errors in the citation of ideas and informationThere are 9 or more errors in the citation of ideas and informationWriting Quality10-9 Points8 Points7 Points6-0 Points0 – 2 errors or exceptions to the rules of grammar, spelling, word usage, punctuation and formal written work as presented in the 6th edition of the APA manual3 – 5 errors or exceptions to the rules of grammar, spelling, word usage, punctuation and formal written work as presented in the 6th edition of the APA manual6 – 9 errors or exceptions to the rules of grammar, spelling, word usage, punctuation and formal written work as presented in the 6th edition of the APA manual10 or more exceptions to the rules of grammar, spelling, word usage, punctuation and formal written work as presented in the 6th edition of the APA manualFormat Subtotal_____of 40 pointsTotal Points _____of 325 points
READ MORE >>
Antisocial Personality Disorder Study GuideAntisocial Personality DisorderIntrod ...
Antisocial Personality Disorder Study Guide
Antisocial Personality Disorder
Introduction
The Diagnostic and Statistical Manual of Mental Disorders (DSM 5) classifies the ten personality disorders into three clusters: A, B and C. Antisocial personality disorder lies within cluster B, besides histrionic, narcissistic and borderline personality disorders (American Psychiatric Association, 2013). Class B disorders are characterized by unpredictable, emotional and dramatic interactions between the individual and other persons. The clinical features include a pervasive pattern of disregard for and violation of the rights of other persons, beginning from above the age of fifteen years. The individual performs acts that serve as grounds for arrest by resisting social norms pertaining to expected lawful behavior. They may also engage in repeated lying, acts of deception and using aliases or conning others for monetary gain or pleasure. Other features include impulsivity/failure to plan, aggressiveness and irritability, often involving assaults and physical fights and consistent irresponsibility marked by failure to maintain reliable work behavior or honest monetary obligations. The person may also exhibit lack of remorse, indifference or rationalize hurting or mistreating other individuals. The person should be at least eighteen years old and the disorder’s onset should be before fifteen years whereas the antisocial behavior ought not to be exclusively within schizophrenia or bipolar disorder.
Figure 1: DSM 5 Criteria for Classifying Personality Disorders
Differential Diagnoses
Paraphilias, Posttraumatic Stress Disorder, Schizophrenia, Schizoaffective disorder, Schizophreniform disorder, Social phobia, Alcoholism, Anxiety Disorders, Brief Psychotic Disorder, Bulimia Nervosa, Depression, Dissociative Disorders, Ganser Syndrome, Illness Anxiety Disorder (also known as hypochondriasis), Marrow Failure Syndromes.
Figure 2: Differential Diagnoses of Antisocial Personality Disorder
Epidemiology
The lifetime prevalence of ASPD is estimated at 1 to 4 % within the general population. Males have a likelihood of thrice to five times of being diagnosed with ASPD than females, having incidences of 6 % and 2 % respectively. Reliable studies reveal decreasing prevalence rates with increasing age, attributable to personality trait changes with age and increasing mortality with individuals having the antisocial personality disorder. Cultural considerations for personality disorders are founded on the social-historical concepts of personality, developmental processes and neurobiology. Western cultures encouraging individualism and independence may be reflected in self-reported psychological stress among persons endeavoring to establish a “goodness of fit” between their style and the immediate society.
Psychotherapy is the mainstream treatment for antisocial personality disorder. The therapist focuses on changing the patient’s thinking process (cognitive therapy) and encouraging socially acceptable behavior (behavioral therapy). Family therapy increases the understanding among family members of the person with the condition whereas group therapy should be coutured to meet the needs of individuals with the disorder. Group therapy encourages the person to share his/her experience with other persons having the disorder. Medication is helpful in stabilizing mood swings or treating the distressing symptoms such as impulsivity and violent aggressiveness. Alcohol dependence is managed with nortriptyline whereas bromocriptine and nortriptyline manage anxiety. Phenytoin may decrease the frequency and intensity of impulsive acts. Figure 2: Therapy modalities for ASPD
The prognosis for ASPD is often poor. Persons with antisocial personality disorder have higher risk for substance abuse, besides higher likelihood of being imprisoned for criminal acts. They also have higher likelihood to die via violence. Since they rarely seek medical attention independently, the legal system is the main body availing treatment to them.
The diagnosis of ASPD depends primarily on complete medical history and physical evaluation. No specific laboratory tests may diagnose any personality disorder, although the doctor may use blood tests, X-rays of the chest and abdomen; and CT-scan of the head to rule out physical illnesses that could have caused the symptoms.
Co morbidities of ASPD include other mental disorders, particularly schizophrenia. ASPD manifests symptoms suggestive of psychosis and propensity for violence. Nonetheless the violence is to lesser extremes than in schizophrenia and occurs only during a manic episode, marked with agitated behavior.
The ethical and legal considerations pertaining to ASPD arises first from the fact that the DSM criteria centers on the criminal and antisocial behavior instead of the underlying interpersonal deficits and personality structure. The conflict centers on whether the persons have medical conditions or intentionally engage in social rule breaking without remorse (Yakeley and Williams, 2018). The medical and legal disciplines are often in dilemma whether the individuals ought to be punished for their criminal acts or treated with moral re-education.
Patient education should include increasing awareness of the condition to the individual. The person should also be directed to see the detrimental effects of their irresponsible acts. Also the therapist should direct them to envisage the benefits of socially acceptable behavior (Skodol, 2020). They could be encouraged to seek employment opportunities, pay bills and loans on time and provide child support.
References
- American Psychiatric Association (2013). DSM 5. American Psychiatric Association, 70.
- Fisher KA, Hany M. Antisocial Personality Disorder. [Updated 2020 Dec 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546673/
- Khalifa, N., Duggan, C., Stoffers, J., Huband, N., Völlm, B. A., Ferriter, M., & Lieb, K. (2010). Pharmacological interventions for antisocial personality disorder. The Cochrane database of systematic reviews, (8), CD007667. https://doi.org/10.1002/14651858.CD007667.pub2
- Mulder, R. (2017) Cultural Aspects of Personality Disorder. The Oxford Handbook of Personality Disorders. Retrieved from doi 10.1093/oxfordhb/9780199735013.013.0013
- Skodol, A. (2020) Antisocial Personality Disorder. University of Arizona College of Medicine. Retrieved from https://www.msdmanuals.com/home/mental-health-disorders/personality-disorders/antisocial-personality-disorder
- Yakeley, J., & Williams, A. (2018). Antisocial personality disorder: New directions. Advances in Psychiatric Treatment, 20(2), 132-143. doi:10.1192/apt.bp.113.011205
READ MORE >>
Applying Duck’s Change Curve Model NUR699NUR 699 GC Week 5 Assignment 1 Evide ...
Applying Duck’s Change Curve Model NUR699
NUR 699 GC Week 5 Assignment 1 Evidence-Based Practice Proposal – Section E: Change Model
Details for Applying Duck’s Change Curve Model NUR699:
In 500-750 words (not including the title page and reference page), apply a change model to the implementation plan. Include the following:
- Roger’s diffusion of innovation theory is a particularly good theoretical framework to apply to an EBP project. However, students may also choose to use change models, such as Duck’s change curve model or the transtheoretical model of behavioral change. Other conceptual models presented, such as a utilization model (Stetler’s model) and EBP models (the Iowa model and ARCC model), can also be used as a framework for applying your evidence-based intervention in clinical practice.
- Apply one of the above models and carry your implementation through each of the stages, phases, or steps identified in the chosen model.
- In addition, create a conceptual model of the project. Although you will not be submitting the conceptual model you designed in Topic 5 with the narrative, the conceptual model should be placed in the appendices for the final paper.

Prepare this assignment according to the APA guidelines found in the APA Style Guide, located in the Student Success Center. An abstract is not required.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to Turnitin. Please refer to the directions in the Student Success Center.
Upon receiving feedback from the instructor, refine “Section E: Change Model” for your final submission. This will be a continuous process throughout the course for each section.
ORDER INSTRUCTIONS-COMPLIANT NURSING PAPERS
Also Read:
IDS 400 The Four General Education Lenses
BIO 111 – Genetics of Corn Experiment 1 A Monohybrid Cross
Borderline Personality Disorder (BPD)
POST HSV 400 discussions
Subsystem: Safety & Transportation Paper
NU621 Unit 8 Reflection Paper
READ MORE >>
Article Critique Sample PaperCritiquing a research article permits healthcare pr ...
Article Critique Sample Paper
Critiquing a research article permits healthcare providers to gather the necessary evidence-based knowledge to utilize in clinical practice to improve the general quality of patient care. This comprehensive process necessitates a nurse to carefully go through the article and intensively analyze it. The purpose of this piece of paper is to critically appraise the Effect of Intentional Nursing Rounds Based on the Care Model on Patient’s Perceived Nursing Quality and their Satisfaction with Nursing Services’ report.
Introduction and Identification of the Problem
After extensive review of The Effect of Intentional Nursing Rounds Based on the Care Model on Patient’s Perceived Nursing Quality and their Satisfaction with Nursing Services’ report, the report was well written with minimal grammatical errors. The well-structured introductory section attains the attention of the reader or rather makes the subject area interesting. It further explains the key concepts of the research and the background of the study (Cathala & Moorley, 2018).
The introduction further elaborates on the details mentioned in the abstract and what to foresee in the manuscript. The purpose of this study is well outlined. For instance, this study examined the effects of intentional nursing rounds based on the care model on patients’ perceived nursing quality and their satisfaction with nursing services (Shin & Park, 2018). This problem statement purposefully introduces and orients the reader to the significance of the topic under study.
Aside from the purpose of the study, the researchers in this report also highlight two alternative hypotheses that were subjected to validation. The first hypothesis stated that the interventional group under intentional nursing rounds would demonstrate a significant level of perceived nursing quality when compared to the control group without rounding services (Shin & Park, 2018). Secondly, the interventional cohort under intentional nursing rounds would demonstrate a higher level of satisfaction with nursing services than the control group without rounding service (Shin & Park, 2018). The roles of hypotheses in research are overwhelming.
They describe the exploration in concrete terms, provide the backbone of evidence to ascertain the validity of research as well as assisting in data analysis to assess the reliability and validity of the study (Vance et al., 2013). Likewise, hypotheses emphasize the validity and scientific attribute of research methodologies by linking the underlying theoretical basis and the specific research problem in addition to furnishing the researchers with distinct clarifications and restatements of the research problem.
Literature Review Analysis
The logical flow of any research must include the literature review part. A literature review serves multiple functions. To begin, it is ordinarily the initial step of clarifying the intention of any research. This part further facilitates the development of clear comprehension of the research topic by both the researchers and the readers (Cathala & Moorley, 2018). Additionally, discerning existing conceptual framework approaches to the study topic and refining the research topic can only be practical via the literature review. Lastly, the literature review mitigates the burden of readers unfamiliar with the topic experience striving to understand the rationale of the study.
Consequently, this section of the research must be well written to fulfill its purpose. Looking at the literature review section of this study, several key deductions can be outlined. Firstly, the articles referenced in this article are not current since principally most of them are older than five years probably due to the time the study was conducted. Nevertheless, most of the references used are peer-reviewed journal articles that are relevant to the topic under investigation. The articles summarize what is already known about the research topic and highlight the available gaps such as few pieces of research on intentional rounding reported in the literature in Korea as well as the need to view patients’ satisfaction from the patients’ angle (Shin & Park, 2018). Finally, the report’s literature review outlines the critical contribution to new knowledge that this study will add. For instance, the study will emphasize intentional rounds that would draw patient-oriented nursing care with the identification of the patients’ needs.
Participants, Sampling Issues, and Study Setting Analysis
Participants utilized in the study were patients from two general surgical wards in a large metropolitan teaching hospital in Korea. To qualify as a participant, one had to understand the survey questions without any difficulty in communication. Similarly, the participant had to be an adult Korean-speaking patient admitted to the surgical unit. However, the exclusion criteria included those patients transferred during research duration, those who were discharged as well as those who lost their lives during the research period (Shin & Park, 2018). The sampling was non-probability sampling as it followed the admission register. Ratelle et al. (2019) describe this type of sampling as non-random as not all members of the population have an equal chance of being selected as participants. This type of sampling is mostly utilized by researchers where it is difficult to procure a random sample due to time and cost considerations. The sample is therefore not a true representation of the general population.
Out of the 155 participants assessed for eligibility, 152 were recruited. Initially, there was an equivalent allocation of participants across the experimental and the control group. Subsequently, six from the experimental group discontinued intervention while one from the control group discontinued the intervention leaving a total analyzable sample of 145. The study setting where data collection took place was in two orthopedic wards of a metropolitan teaching hospital in Korea. Data from this setting was collected at different times. The data for the control group that was under conventional rounding was collected from subjects admitted between November 1, 2015, and March 25, 2016. The data from the experimental group under intentional nursing was collected from subjects admitted between April 1, 2016, and October 25, 2016.
Ethical Considerations
Ethical issues in medical explorations involving human subjects have been in existence since taking roots in 1964 through the Declaration of Helsinki issued by the World Medical Association. This particular declaration outlined two fundamental ethical issues; informed consent and ethical approval (Wu et al., 2019). Informed consent is an interactive process by which the researchers educate the participants about the research, benefits, and risks of the study before asking the participants to voluntarily and willingly consent to the study. On the other hand, ethical approval out to be done by the ethics approval committee after a detailed and careful viewing of the appropriateness of the study design (Wu et al., 2019). Besides, it is stipulated that all research articles involving human subjects should essentially submit their report on ethical approval and informed consent prior to their publication.
Following an in-depth review of the research. It is crystal clear that the researchers of the article abided by the elements of ethical considerations in research. For instance, the study was undertaken after receiving approval from the Institutional Review Board of Bundang CHA Hospital (Approval No. 2015-11-198-002). In addition, all participants signed a written consent form after being enlightened about study goals, data collection, and confidentiality of the procedures as well as the freedom to walk out of the research process (Shin & Park, 2018). Subsequently, the rights of the participants were safeguarded in this exploration.
Research Design, variables, and Methodology Analysis
Study design refers to the methodology utilized to investigate the research problem in question (Ratelle et al., 2019). Study variables on the other hand refer to a person, thing, place, or phenomenon that the research attempts to measure (Ratelle et al., 2019). The two types of variables greatly deployed in research are dependent and independent variables. The dependent variable just as the name suggests is contemplated to change on manipulation of the independent variable. It is the presumed effect (Ratelle et al., 2019). Meanwhile, the independent variable is the presumed cause and is the stable variable that the investigators navigate.
With that background in mind, in-depth scanning of this article reveals an experimental research design. This quasi-experimental included a non-equivalent and non-synchronized control group. According to Ratelle et al. (2019), quasi-experimental study designs feature both control and intervention groups but do not provide for random assignment of the treatment group. Similarly, in this research, the control and treatment groups were assigned according to the admission register. A quasi-experimental design is best suitable when a cause-effect relationship is desired to be established with a feasible introduction of experimental stimuli but randomization is impractical or unethical.
The dependent variables in this study were patient’s perceived quality of nursing and patient’s satisfaction with nursing services. According to Shin and Park (2018), these variables referred to how patients felt about the nursing care they received and the degree of subjectively perceived satisfaction between patients’ expectation of nursing service and actual service provided respectively. Nonetheless, the independent variables were the conventional nursing rounds and intentional nursing rounds given to the control and treatment groups respectively.
Data Analysis and Results
Data analysis entailed an initial identification of homogeneity of participants’ baseline variables and characteristics between control and experimental groups using descriptive statistics, chi-square tests, Fisher’s exact test, and independent T-test. This was followed by the assessment of the impact of intentional rounding utilizing the difference-in-indifference method to analyze alterations in patients’ perceived nursing quality and their satisfaction with nursing service. Finally, the mean and the standard deviation of the intervention group were used as measures of the effect size of this study.
The results of this study supported both hypotheses. For instance, in testing the first hypothesis, it was discovered that the experimental group’s perceived nursing quality level was 0.85 points higher than that of the control group (p =.041) while in the second, it revealed that the level of satisfaction with nursing services from the experimental group was 8.28 points higher than that of the control group (p < .001). In terms of the hierarchy of evidence, this study is at level III (Drisko & Grady, 2019). The nursing theory used in this study is Swanson’s caring model.
The Swanson theory of caring is based on the five fundamental principles including maintaining belief, knowing, being with, doing for, and empowering (Shin & Park, 2018). The study limitations for this study included lack of representation of the patients’ perceived nursing quality and their satisfaction of general patients and at the general level because the study was conducted for patients at a metropolitan teaching hospital to ensure homogeneity. Similarly, the effect of intentional rounding cannot be fully generalized in the clinical setting since the study was conducted in only two surgical units.
Implications for Nursing Practice
As the nursing practice shifts focus to patient-centered care, patients’ experiences become key. The findings of this result influence the nursing practice by advocating for the establishment of intentional rounding to replace conventional rounding. According to this study, this structured nursing system looks after patients at fixed time intervals to assess and manage patients’ basic needs. The nurses are always available to be with and take care of their patients. Subsequently, this type of nursing is perceived as high quality with increased levels of patients satisfaction. It is therefore imperative that nurse leaders should try to adopt such kind of nursing care.
Arguably, this type of care requires manpower in terms of the nursing staff to be available at patients’ disposal. Nurse leaders in their policy making, should advocate for enough staff in healthcare facilities to spearhead the shifting of nursing care from conventional rounding to intentional rounds. Shin and Park (2018) further outline that the findings of their research should form the backbone for further research to systematically improve future nursing practice to eventually increase patients’ safety, nursing needs, nurses’ performance ability, and communication ability, as well as patients’ satisfaction.
Conclusion
Appraising a research article is an elemental skill that all nurses should have to guide their clinical practice. Likewise, nurses should synthesize evidence-based knowledge as well as areas that require future research to help shape and shift the future nursing practice to align with the ever-growing and dynamic healthcare needs.
References
- Cathala, X., & Moorley, C. (2018). How to appraise quantitative research. Evidence-Based Nursing, 21(4), 99–101. https://doi.org/10.1136/eb-2018-102996
- Drisko, J. W., & Grady, M. D. (2019). Step 3 of EBP: Part 1—evaluating research designs. In Essential Clinical Social Work Series (pp. 107–122). Springer International Publishing. https://doi.org/10.1007/978-3-030-15224-6_6
- Ratelle, J. T., Sawatsky, A. P., & Beckman, T. J. (2019). Quantitative research methods in medical education. Anesthesiology, 131(1), 23–35. https://doi.org/10.1097/ALN.0000000000002727
- Shin, N., & Park, J. (2018). The effect of intentional nursing rounds based on the care model on patients’ perceived nursing quality and their satisfaction with nursing services. Asian Nursing Research, 12(3), 203–208. https://doi.org/10.1016/j.anr.2018.08.003
- Wu, Y., Howarth, M., Zhou, C., Hu, M., & Cong, W. (2019). Reporting of ethical approval and informed consent in clinical research published in leading nursing journals: a retrospective observational study. BMC Medical Ethics, 20(1), 94. https://doi.org/10.1186/s12910-019-0431-5
READ MORE >>
Article Critique Pay for Performance Sample PaperArticle Critique: Pay for Perfo ...
Article Critique Pay for Performance Sample Paper
Article Critique: Pay for Performance
Healthcare providers utilize research for a variety of health reasons including but not limited to making clinical decisions, improving the quality of patient care, and formulation of healthcare policies. This evidence-based practice is highly recommended because of its overwhelming value in improving the quality of patient care. Consequently, it is elemental for nurses to develop skills for filtering and determining which research articles to deploy best hence critiquing a research article is a crucial skill to gather evidence-based research. The purpose of this piece of writing is to appraise the Challenges of Implementing Pay for Performance Plan in the Views of Nurses Working in Hospitals Affiliated to Mashhad University of Medical Sciences, a Qualitative Study Report by Rasi et al. (2018).
After going through the Challenges of Implementing the Pay for Performance (PFP) Plan in the Views of Nurses Working in Hospitals Affiliated to Mashhad University of Medical Sciences, a Qualitative Study Report, it is crystal clear that the exploration was well written with the slightest grammatical errors. To begin with, the title is a correct description of the research and informative as it gives a glance at the key concepts as well as stating the variables and methods of the research. The author of the article has further logically organized the research by describing the abstract exhaustively. The abstract is a mirror image of the report and clearly outlines the background, purpose of the study, methods, results, and conclusions (Moorley & Cathala, 2019). After reviewing the report, it is evident that the research is logical as it has followed all the steps of research. For example, the authors provided a comprehensive introduction, significant literature review, sound data collection, and an in-depth discussion.
Similarly, the introduction section of the article was well structured as it gains the attention of the reader or rather makes the subject area interesting. Additionally, it defines the key concepts of the research such as nurse, hospital, human resource, and pay for performance (Rasi et al., 2018). The introduction also makes the purpose of the article clear. However, this being a qualitative study, it didn’t seek to test a hypothesis. Moorley and Cathala (2019) recommend a statement of the purpose of the study that incorporates the research statement. For instance, in this article, Rasi and associates (2018) aimed at exploring the challenges of the PFP plan in the views of nurses working in hospitals affiliated to Mashhad University of Medical Sciences, Iran.
The theoretical framework of this research was effectively structured. The authors begin by reviewing the challenges facing the human resource department and the impact of the value-based payment systems and comparing them to the results of various studies globally. The theoretical framework subsequently narrows down to a specific variable and defines this variable based on the distinct standpoint of nurses.
After a deep review of the research, the literature review is comprehensive and extensive. The authors have incorporated evidence and important findings from previous studies that relate to the topic of interest. The references used are a concoction of both current and old sources. Similarly, the lion’s share of these references is primary hence show a wide range of discrepancies. Nevertheless, the literature review elaborates the context of the study by expounding on value-based payment systems through the integration of both old and recent studies.
The methodology section was sound. The authors used a qualitative research approach to address the research objectives. The study setting is well highlighted and the type of sampling technique, as well as the sample size, are clearly indicated. Rasi et al. (2018) set forth an apparent inclusion criterion which consisted of nurses with at least 10 years of working experience. The methods of data collection were also pinpointed and data were collected until saturation as recommended (Moorley & Cathala, 2019). Additionally, ethical issues such as informed consent and data confidentiality were confronted in this report. The data collected was analyzed using content analysis which is one of the recommended styles of analyzing qualitative data. The issues concerning reliability, accuracy, precision, and consolidation of data were taken care of via the triangulation method. This methodology is therefore sound and replicable.
The findings of this report were well presented in tables and figures. The themes analyzed were clearly linked to the data that was collected and the information found in the literature review. The discussion section was comprehensive. The authors contextualize their study by relating the research findings to findings of other studies across the globe. The findings of this research strongly connect with research objectives and aims and are supported with literature. However, the research fails to indicate the limitations encountered in the study. The study recommends proper planning before the implementation of pay for performance plan to avoid the challenges associated with this payment system.
Level of Evidence
The level of evidence is based on the methodological quality of design, validity, and applicability to patient care. In terms of the hierarchy of evidence, qualitative studies usually fall short of quantitative studies. For instance, this being a single qualitative study, it can be ranked at level VI in terms of evidence (Astroth, 2018). However, Astroth (2018) proposes a critical analysis and scoring of individual qualitative study across five parameters namely; descriptive vividness, methodological congruence, analytical preciseness, theoretical connectedness, and heuristic relevance. The legend for this scoring scale is designated QI to QIII based on the percentage criteria score. This report can be ranked QII and it meets 50% to 74% of all the criteria (Astroth, 2018).
Decide if the Study is Applicable to your Practice
Value-based payment systems such as pay for performance are beginning to take roots in human resource management. The benefits of these payment mechanisms are overwhelming. Hermer et al. (2018), in their work, discovered that resident and nursing homes that adopted pay for performance plans had significant improvement in patient care quality as it became safe and patient centered. Similarly, Mathes et al. (2019) in their exploration concluded that pay for performance in hospitals was associated with efficiency in the running of the hospital facilities and equity in the allocation of healthcare resources. In terms of cost and staffing, pay for performance is associated with an overall reduction in healthcare costs and increased job satisfaction respectively.
These overwhelming benefits of the PFP plan can only be achieved with solid planning and execution of the program. This entire study applies to my practice as the findings of this research give a glimpse of future nursing practice. That as current and future nursing leaders along with the stakeholders and policymakers, we should be able to critically evaluate a program such as PFP, taking into account the advantages and the challenges of its execution. Consequently, such in-depth reviews will result in the development of laws and guidelines that will aim at controlling the challenges while enjoying the benefits of the program.
Conclusion
Appraisal of research is vital for shaping the future of the nursing practice. Policymakers and stakeholders should extensively evaluate available information to guide their decision-making. Value-based payment systems such as pay for performance significantly improves the quality of patient care, job satisfaction and reduces overall healthcare costs. Nonetheless, careful planning and implementation are central to relish these benefits.
References
- Astroth, K. S. (2018). Focusing on the fundamentals: Reading qualitative research with a critical eye. Nephrology Nursing Journal: Journal of the American Nephrology Nurses Association, 45(4), 381–348.
- Hermer, L., Cornelison, L., Kaup, M. L., Poey, J. L., Drake, P. N., Stone, R. I., & Doll, G. A. (2018). Person-centered care as facilitated by Kansas’ PEAK 2.0 Medicaid pay-for-performance program and nursing home resident clinical outcomes. Innovation in Aging, 2(3), igy033. https://doi.org/10.1093/geroni/igy033
- Mathes, T., Pieper, D., Morche, J., Polus, S., Jaschinski, T., & Eikermann, M. (2019). Pay for performance for hospitals. Cochrane Database of Systematic Reviews, 7, CD011156. https://doi.org/10.1002/14651858.CD011156.pub2
- Moorley, C., & Cathala, X. (2019). How to appraise qualitative research. Evidence-Based Nursing, 22(1), 10–13. https://doi.org/10.1136/ebnurs-2018-103044
- Rasi, V., Maleki, M. R., Yarmohammadian, M. H., Reyhani Yasavoli, A., & Doosty, F. (2018). Challenges of implementing pay-for-performance plan in the views of nurses working in hospitals affiliated to Mashhad university of medical sciences: A qualitative study. Modern Care Journal, 15(4), e87007. https://dx.doi.org/10.5812/modernc.87007
READ MORE >>
When emergency situations arise, first responders rush to provide critical aid. ...
When emergency situations arise, first responders rush to provide critical aid. But in the complex landscape of healthcare roles, there is debate about whether registered nurses should be categorized among these frontline heroes.
This article will examine what constitutes a first responder, how nurses fit into the picture, their authorized roles in mass casualty incidents, and other critical considerations around categorizing these healthcare professionals.
Who Are Considered First Responders?
First responders are specially trained personnel who are among the first to arrive and assist at the scene of an emergency. They must stabilize dangerous situations, triage patients, and provide pre-hospital care to victims before they can receive definitive treatment at a hospital.
The Department of Homeland Security officially designates the following groups as first responders:
- Firefighters
- Police Officers
- EMTs
- Paramedics
These professions all undergo rigorous training to prepare them for diverse emergencies. Whether a cardiac arrest, car accident, or crime is unfolding – first responders must take command of chaotic scenes using their expertise.
Characteristics of First Responders
While titles may vary, some universal characteristics apply to certified first responders across fields:
Immediate Response
First responders are dispatched to crisis sites via 9-1-1 calls through public safety access points. First responders are equipped for the fastest possible response times for critical injuries where minutes make the difference between life and death.
Specialized Training
To qualify, extensive education in emergency medicine, assessment, and field treatment is required. Ongoing skills training and evaluations keep first responders sharp and ready to intervene across heterogeneous incidents.
Scene Assessment
A huge part of a first responder’s duties includes quick analysis of emergency scenes to determine the mechanism of injury or nature of the illness. This allows them to accurately triage patients and determine transport priorities if multiple victims are involved.
Pre-Hospital Care
Whether through CPR, bandaging wounds, administering oxygen, or even helping deliver babies – first responders initiate urgent care using specialized techniques and equipment at the scene. This aims to stabilize and improve outcomes before the patient arrives at the ER.
What Is a Frontline Worker in Healthcare?
Frontline workers in healthcare refer to the staff who engage directly with patients to provide care. They assume higher physical and psychological risk as the first point of contact with those seeking treatment.
Common frontline healthcare worker roles include:
- Nurses
- Emergency Medical Technicians
- Medical Assistants
- Physicians
- Home Health Aides
- Phlebotomists
These jobs usually require and exceed varying levels of medical education and credentials to practice. But what they share is working face-to-face with the injured, the sick, and the vulnerable day in and day out – especially when crises like pandemics transpire.
Comparing Key Duties: Nurses vs EMTs
Both nurses and EMTs undisputedly function as indispensable frontline healthcare workers. But there are also roles and capabilities worth contrasting:
TABLE
NursesEMTsSettingNurses typically provide care to admitted patients within hospitals.EMTs operate in the field, responding urgently to emergencies via 9-1-1 dispatch.ScopeRegistered nurses treat health conditions, operate equipment, administer medications, and coordinate care plans under a wider patient care umbrella.EMTs specifically focus on emergency response – assessing scenes, triaging severity, and initiating urgent treatment.TrainingNurses complete more advanced education culminating in RN licensure granting broader practice rights in healthcare settings after the emergency phase. EMT programs are shorter since skills concentrate on stabilization and transport instead of ongoing care.SpecializationThe RN license allows general nursing practice, but nurses can also gain additional credentials in focused areas like pediatrics, oncology, or surgery. EMTs can fill different designated roles like wildland firefighters or tactical paramedics.While both dispatcher roles involve urgent facets of medicine, EMTs focus on emergency response and stabilization until the patient can receive comprehensive hospital care from nurses and physicians. Both demonstrate selflessness and compassion that make them indispensable frontline healthcare heroes.
When are Nurses First Responders?
Clearly, an ability to make rapid, lifesaving decisions under pressure in many situations defines first responders. But where exactly do nurses fit in?
Nurses are essential healthcare professionals who provide around-the-clock patient care in medical settings after hospital transport. They assist physicians in developing treatment plans, communicating with families, operating complex equipment, and much more.
With advanced education in anatomy, pathophysiology, pharmacology, and disease management, there is no doubt nurses have expertise that allows them to function in crises. However, pre-hospital emergency care in the field is not a standard or defining duty of registered nurses.
Compare this to EMTs who specifically train in and are certified to diagnose, treat, and transport critical patients under fire-department or ambulance jurisdiction before they ever reach the ER doors.
Are Nurses First Responders in a Mass Casualty Incident?
While the nurse’s role is typically after the emergency phase, things get more complex in special situations:
Mass Casualty Events
In the case of a disastrous mass casualty scenario where the victims far outnumber existing first responders, emergency operation plans tap into expanded medical resources. Off-duty EMTs may be called in, while on-site nurses at nearby hospitals may deploy to the field as reinforcements.
In such dire scenarios, nurses serve as emergency triage volunteers functioning in a first responder capacity. It becomes all hands on deck. So, context matters when distinguishing nurses as first responders.
Good Samaritan Aid
Another example where ER nurses potentially act as first responders involves sudden emergencies unfolding in public places. If a nurse witnesses a person collapse nearby due to sudden cardiac arrest or choking, for example – legal and ethical codes require they render reasonable emergency aid within their qualifications.
This is no different than if an off-duty doctor or firefighter notices a traumatic health crisis arise away from their professional jurisdiction. Any medically qualified individual is bound to vital good Samaritan laws.
Can Nurses Help in an Emergency Situation?
Absolutely. Apart from specific on-site disasters where emergency agencies require all qualified backup, nurses can still provide essential aid without identifying as first responders. Here are some examples:
- Calling 9-11 at accidents when people are injured or in medical distress.
- Volunteering and maintaining certification in CPR/AED administration to help resuscitate cardiac arrest sufferers.
- Applying pressure on heavily bleeding wounds or using tourniquets before paramedics arrive.
- Assisting choking victims at restaurants using abdominal thrusts if trained.
- Offering overdose victims basic help if opioid reversal agents like Narcan are available.
- Sharing critical medical history with paramedics reaching emergencies.
During catastrophes like the COVID-19 pandemic, nurses undoubtedly served at the frontlines right alongside first responders. And they will continue filling such desperate societal needs as they arise.
But nursing fundamentally deals with patient care, communication, critical thinking, and education – not emergency response. This helps delineate nurses from emergency medical technicians under normal non-disaster circumstances.
First Responder and Healthcare Worker Discounts
The distinction gets muddled around first responder discounts and recognition. For example, the American Nurses Association successfully lobbied for the Emergency Responder Act to include registered nurses for benefits like federal retirement credit during COVID-19.
And many businesses extend discounts broadly to all hospital staff or frontline workers – whether emergency responders or not. Appreciating nurses for their sacrifice makes sense generally.
But most formal first responder acknowledgment initiatives strictly define the term to honor only personnel operating under those crisis-response roles day-to-day. Blurring professional boundaries too much can undermine nurses’ specialized expertise and scope.
Why is precise language important here? Beyond mere titles or discounts, appropriate professional boundaries in medicine impact:
- Public understanding in emergencies.
- Workplace laws, pay, insurance considerations.
- Operating authority in crises.
- Safety and capabilities around skills/training.
For these reasons and more, correctly distinguishing nurses from emergency medical services (EMS) personnel as first responders carries real relevance.
Summary: Are Nurses First Responders?
First responders assume specialized duties to respond urgently to medical crises in the field using autonomous judgment. Though absolutely essential healthcare professionals, nurses are not trained or necessarily certified first responders under normal circumstances.
However, standard emergency services may incorporate registered nurses to help fill the gaps. Good Samaritan laws ethically obligate any healthcare practitioner to assist in public medical emergencies, too. In the end, roles around emergency response versus ongoing care, are important to differentiate – even if we equally honor all those who sacrifice to save lives.
READ MORE >>
3M6 Assignment PLG – BSHCA – 4 5 RN-BSN – 1 ...
M6 Assignment PLG – BSHCA – 4
READ MORE >>
relevant or academic; Meets the minimum number of required citations in assignm ...
READ MORE >>
