Our Previous Samples
“Telenursing and Remote Access Telehealth” (pp. 359–388)Dykes ...
Dykes
READ MORE >>
Discussion: The Application of Data to Problem-Solving NURS 6051 Example Solutio ...
Discussion: The Application of Data to Problem-Solving NURS 6051 Example Solution
For decades, different institutions have been acquiring information and using it to solve various problems. Small businesses, as well as large enterprises, have also been doing the same. In the healthcare sphere, nurses have been using different methods to obtain data, which is then analyzed and later used to find solutions for various problems in the sector. As McConigle and Mastrian (2017) mentioned, the nursing profession is information-intensive. Without collecting relevant data, the nursing sector would be unable to deliver quality services to patients, thereby crippling the entire healthcare realm.
Informatics Clinical Application
While working as a Clinical Nurse Coordinator, sometimes back, data collection was a vital part of my operation. On the 28-bed telemetry floor, I realized that whenever I approached the management without adequate data to support my ideas about solving various problems at the workplace, the concepts would be brushed aside.
However, the administration was always happy to listen to my thoughts on something if my presentation had adequate data to support the concepts. Therefore, no matter how good your thoughts are, they do not mean a lot unless you have gathered enough facts to support them. That is why the data collection and analysis process is vital to the nursing practice realm.
Data helps to support arguments conclusively (Sweeney, 2017). Currently, there is an idea that I am trying to put on the table that involves proving to the management that the facility needs more nurses on the telemetry floor to free-charge nurses for the numerous patient tasks that they handle during the shifts. Charge nurses ensure everything runs smoothly at a medical facility during a certain shift. They assume leadership during the hours that they are in charge.
Their clinical experience ensures that other nurses in the department deliver quality care to the patients. If a nurse fails to deliver, they are supposed to report them to the management. They are also responsible for coming up with work schedules, overseeing discharges and admissions, and helping to check up on patients.
In the 28-bed telemetry floor, charge nurses are too busy to oversee their real duties, primarily because there are not enough nurses in the department. Instead of playing the oversight role, they carry out the usual nursing tasks like administering medicine and checking up on patients occasionally. On a daily basis, the number of RNs versus patients is recorded and computerized. Presently, I have data collected over the previous month.
My preliminary analysis of the data reveals that the number of patients seems to be overwhelming the nurses. Many patients are being admitted to the floor, forcing the charge nurse to leave their actual oversight duties to attend to patients. Things can easily slip out of hand in such scenarios since no one oversees the various patient care processes. I have also been collecting patient feedback during the period, based on which I have concluded that patient satisfaction is dismal whenever the charge nurse is involved in patient care.
Informatic competence helps to alter clinical decisions positively and eventually improve patient outcomes (McConigle & Mastrian, 2017). Data collected over six months will be adequate to fully convince the management of the need for a change at the facility to improve patient outcomes as well as satisfaction.
As the nursing profession evolves, technology is bound to influence patient outcomes significantly (Nagle et al., 2017). The need for EHR competence is also going to rise. EHR makes data collection and analysis easier. As a young practitioner, I plan on becoming familiar with the various technology-based methods of data collection and analysis to improve myself as a nurse and ultimately advance the nursing profession.
Discussion: The Application of Data to Problem-Solving NURS 6051 Week 1 Discussion References
McGonigle, D., & Mastrian, K. G. (2021). Nursing informatics and the foundation of knowledge (4th ed.). Burlington, MA: Jones & Bartlett Learning.
Nagle, L. M., Sermeus, W., Junger, A., & Bloomberg, L. S. (2017). Evolving Role of the Nursing Informatics Specialist. Forecasting Informatics Competencies for Nurses in the Future of Connected Health, 212.
Sweeney, J. (2017). Healthcare informatics. On-Line Journal of Nursing Informatics, 21(1). https://search.proquest.com/indexingvolumeissuelinkhandler/2034896/On+-+Line+Journal+of+Nursing+Informatics/02017Y02Y01$23Feb+2017$3b++Vol.+21+$281$29/21/1;jsessionid=CE90CAE74C27162F08A1240D7D181354.i-0ff9edadb0c803625
Discussion: The Application of Data to Problem-Solving NURS 6051 Week 1 Discussion Instructions
In the modern era, there are few professions that do not to some extent rely on data. Stockbrokers rely on market data to advise clients on financial matters. Meteorologists rely on weather data to forecast weather conditions, while realtors rely on data to advise on the purchase and sale of property. In these and other cases, data not only helps solve problems, but adds to the practitioner’s and the discipline’s body of knowledge
Module 1: What Is Informatics? (Weeks 1-2)
Students will:
- Analyze how data collection and access can be used to derive knowledge in a healthcare setting
- Analyze the role of the nurse leader in using clinical reasoning and judgement in the formation of knowledge
- Explain the role of the nurse as a knowledge worker
- Explain concepts of nursing informatics
- Create infographics related to nursing informatics and the role of the nurse as a knowledge worker
Discussion: The Application of Data to Problem-Solving
In the modern era, there are few professions that do not to some extent rely on data. Stockbrokers rely on market data to advise clients on financial matters. Meteorologists rely on weather data to forecast weather conditions, while realtors rely on data to advise on the purchase and sale of property. In these and other cases, data not only helps solve problems, but adds to the practitioner’s and the discipline’s body of knowledge.
Of course, the nursing profession also relies heavily on data. The field of nursing informatics aims to make sure nurses have access to the appropriate date to solve healthcare problems, make decisions in the interest of patients, and add to knowledge.
In this Discussion, you will consider a scenario that would benefit from access to data and how such access could facilitate both problem-solving and knowledge formation.
To Prepare:
- Reflect on the concepts of informatics and knowledge work as presented in the Resources.
- Consider a hypothetical scenario based on your own healthcare practice or organization that would require or benefit from the access/collection and application of data. Your scenario may involve a patient, staff, or management problem or gap.
By Day 3 of Week 1
Post a description of the focus of your scenario. Describe the data that could be used and how the data might be collected and accessed. What knowledge might be derived from that data? How would a nurse leader use clinical reasoning and judgment in the formation of knowledge from this experience?
Assignment: The Nurse Leader as Knowledge Worker
The term “knowledge worker” was first coined by management consultant and author Peter Drucker in his book, The Landmarks of Tomorrow (1959). Drucker defined knowledge workers as high-level workers who apply theoretical and analytical knowledge, acquired through formal training, to develop products and services. Does this sound familiar?
Nurses are very much knowledge workers. What has changed since Drucker’s time are the ways that knowledge can be acquired. The volume of data that can now be generated and the tools used to access this data have evolved significantly in recent years and helped healthcare professionals (among many others) to assume the role of knowledge worker in new and powerful ways.
In this Assignment, you will consider the evolving role of the nurse leader and how this evolution has led nurse leaders to assume the role of knowledge worker. You will prepare a PowerPoint presentation with an infographic (graphic that visually represents information, data, or knowledge. Infographics are intended to present information quickly and clearly.) to educate others on the role of nurse as knowledge worker.
Reference: Drucker, P. (1959). The landmarks of tomorrow. New York, NY: HarperCollins Publishers.
To Prepare:
- Review the concepts of informatics as presented in the Resources.
- Reflect on the role of a nurse leader as a knowledge worker.
- Consider how knowledge may be informed by data that is collected/accessed.
The Assignment:
- Explain the concept of a knowledge worker.
- Define and explain nursing informatics and highlight the role of a nurse leader as a knowledge worker.
- Include one slide that visually represents the role of a nurse leader as knowledge worker.
- Your PowerPoint should Include the hypothetical scenario you originally shared in the Discussion Forum. Include your examination of the data that you could use, how the data might be accessed/collected, and what knowledge might be derived from that data. Be sure to incorporate feedback received from your colleagues’ responses.
NURS 6051 Module 2: The Role of the Informatics Specialist in Healthcare (Weeks 3-4)
Discussion: Interaction Between Nurse Informaticists and Other Specialists
Nature offers many examples of specialization and collaboration. Ant colonies and bee hives are but two examples of nature’s sophisticated organizations. Each thrives because their members specialize by tasks, divide labor, and collaborate to ensure food, safety, and general well-being of the colony or hive.
Of course, humans don’t fare too badly in this regard either. And healthcare is a great example. As specialists in the collection, access, and application of data, nurse informaticists collaborate with specialists on a regular basis to ensure that appropriate data is available to make decisions and take actions to ensure the general well-being of patients.
In this Discussion, you will reflect on your own observations of and/or experiences with informaticist collaboration. You will also propose strategies for how these collaborative experiences might be improved.
To Prepare:
- Review the Resources and reflect on the evolution of nursing informatics from a science to a nursing specialty.
- Consider your experiences with nurse Informaticists or technology specialists within your healthcare organization.
By Day 3 of Week 3
Post a description of experiences or observations about how nurse informaticists and/or data or technology specialists interact with other professionals within your healthcare organization. Suggest at least one strategy on how these interactions might be improved. Be specific and provide examples. Then, explain the impact you believe the continued evolution of nursing informatics as a specialty and/or the continued emergence of new technologies might have on professional interactions.
By Day 6 of Week 3
Respond to at least two of your colleagues* on two different days, offering one or more additional interaction strategies in support of the examples/observations shared or by offering further insight to the thoughts shared about the future of these interactions.
Assignment: The Impact of Nursing Informatics on Patient Outcomes and Patient Care Efficiencies
In the Discussion for this module, you considered the interaction of nurse informaticists with other specialists to ensure successful care. How is that success determined?
Patient outcomes and the fulfillment of care goals is one of the major ways that healthcare success is measured. Measuring patient outcomes results in the generation of data that can be used to improve results. Nursing informatics can have a significant part in this process and can help to improve outcomes by improving processes, identifying at-risk patients, and enhancing efficiency.
To Prepare:
- Review the concepts of technology application as presented in the Resources.
- Reflect on how emerging technologies such as artificial intelligence may help fortify nursing informatics as a specialty by leading to increased impact on patient outcomes or patient care efficiencies.
The Assignment: (4-5 pages not including the title and reference page)
In a 4- to 5-page project proposal written to the leadership of your healthcare organization, propose a nursing informatics project for your organization that you advocate to improve patient outcomes or patient-care efficiency. Your project proposal should include the following:
- Describe the project you propose.
- Identify the stakeholders impacted by this project.
- Explain the patient outcome(s) or patient-care efficiencies this project is aimed at improving and explain how this improvement would occur. Be specific and provide examples.
- Identify the technologies required to implement this project and explain why.
- Identify the project team (by roles) and explain how you would incorporate the nurse informaticist in the project team.
- Use APA format and include a title page and reference page.
- Use the Safe Assign Drafts to check your match percentage before submitting your work.
Learning Resources
McGonigle, D., & Mastrian, K. G. (2021). Nursing informatics and the foundation of knowledge (4th ed.). Burlington, MA: Jones & Bartlett Learning.
- Chapter 25, “The Art of Caring in Technology-Laden Environments” (pp. 525–535)
- Chapter 26, “Nursing Informatics and the Foundation of Knowledge” (pp. 537–551)
Mosier, S., Roberts, W. D., & Englebright, J. (2019). A Systems-Level Method for Developing Nursing Informatics Solutions: The Role of Executive Leadership. JONA: The Journal of Nursing Administration, 49(11), 543-548.
Ng, Y. C., Alexander, S., & Frith, K. H. (2018). Integration of Mobile Health Applications in Health Information Technology Initiatives: Expanding Opportunities for Nurse Participation in Population Health. CIN: Computers, Informatics, Nursing, 36(5), 209-213.
Sipes, C. (2016). Project management: Essential skill of nurse informaticists. Studies in Health Technology and Informatics, 225, 252-256.
The Impact of Nursing Informatics on Patient Outcomes and Patient Care Efficiencies Example Solution
The ultimate goal of every healthcare practice is to provide the best services to the patients. These goals are gauged and reflected in the quality of the health care services. Patient care efficiency and safety are two elements of quality in healthcare. The role of healthcare technology in improving patient care efficiency, timeliness, and outcomes cannot be overemphasized (Agency for Healthcare Research and Quality, 2021).
In the medical and surgical units in healthcare delivery, bed-bound patients require timely monitoring to reduce their risks of pressure sores and venous thromboembolism. Turning of patients and change of positions are some of the nursing interventions used on bedbound patients to prevent hospital-acquired pressure injuries (HAPI) (Pickham et al., 2018).
Regular turning every two hours in the inpatient units requires proper scheduling. Using nursing informatics can make this process easier, timely, and safe. This paper aims to describe a project proposal to utilize nursing informatics to prevent hospital-acquired pressure injuries through regular turning.
The Project
This project will employ the use of electronic health records and wearable device technology to monitor and implement their nursing plan. In an inpatient unit, different patients require different recurrent interventions to maintain their health and improve recovery. The project will require that nurses coordinate with other healthcare professionals through the institution’s electronic health record system to make decisions and plan care.
In this project, bedbound patients will be monitored remotely through the use of healthcare technologies technology. Patients who cannot ambulate or are not physically active because they are mentally or physically debilitated in the two inpatient units will be identified by the shift nurses and monitored through the electronic health records systems. The nurse will explain the role of technology to patients or their families.
Because different patients will have different schedules for turning, the technology will alert the shift nurses through the electronic health records system. The monitoring will take place at the nurse’s station. The patient will have a sensor technology that will be connected to the EHR through the institution’s local area network (LAN). During that shift, the nursing staff will then implement the two-hourly turning plans after the alert reminder by the system.
Stakeholders
This project will involve various stakeholders involved in direct and indirect patient care. The project will require input from the charge nurses of the two units. The charge nurses will offer the necessary leadership strategies to ensure their shift nurses work as a team to achieve patient care goals. The nurse informaticist will be needed for the success of the project’s technological and care delivery aspects.
The informaticist will ensure the planning for compatibility and usability of the system are given priority for efficiency of use. This project will also impact the patients and their families as they are the immediate recipients of care in the institution. Their feedback and participation will be crucial determinants of the project’s success and the care delivered.
The institution’s procurement officers and accountants will also be impacted because of the need for their services during the purchase and implementation of the technologies. This project will also impact physicians and surgeons because they will be required to prescribe turning and ambulation for these patients and follow them up.
Patient Outcomes and Care Efficiencies
Efficiency in any process is a measurable outcome. The nurses’ input and the output of the care are essential elements of the efficiency of the care delivery. The cost and time spent in providing the care should be commensurate with the cost and time incurred by the patient during this care process. This project will reduce the time spent on physical monitoring of patients requiring two-hour turning (Pickham et al., 2018; Pickham et al., 2018).
The project will personalize the time for the patient’s two-hourly turning and center the schedule around the patient’s needs. Therefore, the project will enhance patient-centered care by avoiding the generalization of nursing plans for all patients in the unit. The alerts from this new system of planning will reduce the risks of medical errors by ensuring that the patient receives nursing care in time without fail.
This new clinical decision support system will minimize errors due to omission because, at the same time, the nurse will be performing the two-hour turning, they will also have the opportunity to check physically on the patient through physical examination. The sensor technology will be able to alert the system on extra findings such as vital signs.
Required Technology
The project will require two technological systems interconnected through the institution’s networks and alert system. Sensory technology will be enabled through a wearable device that will detect lateral and vertical motion of the patient’s body and monitor the duration of inactivity (Renganathan et al., 2019). Duration of inactivity exceeding two hours will be provided an alert to the nurse at the station for prompt action.
By monitoring the patient self turns and nurses turning, this technology will reduce the time the patient spends in inactivity (Schutt et al., 2018). The electronic health records will ensure that the patient data and records of interventions, inclusion physical turning, are available efficiently to every nurse attending to these patients at any time of the day.
Therefore, computer systems will have constant connectivity, and a network will be required to implement this project. The entire clinical decision support system (CDSS) will require portable computers and tablets for easier access anywhere in the unit.
Project Team
The project team will consist of a project manager, the two charge nurses in the medical and surgical units, the institution’s procurement officer, and the nurse manager. The project manager will be a nurse informaticist who will coordinate all project activities. The charge nurses will offer collaborative communication between nurses and other team members and provide timely feedback on the progress and usability of the system.
The procurement officer will be involved in the financial planning and purchase of additional technology to support the EHR. The nurse manager will offer the administrative support and approval of the institution’s administration before implementing the project and oversee that the legal aspects of the project are maintained.
Conclusion
The care of bedbound patients will be made better through this new system of alert system and monitoring. This project aims at improving patient care outcomes and efficiency through a clinical decision support system. The CDSS will include sensory technology using a wearable device and connected to the EHR that will provide a time alert for two-hourly turning for each bedbound patient. The technology will reduce the time spent monitoring these patients and improve monitoring efficiency. The project team will consist of a nurse informaticist as the project manager, charge nurses, and nurse manager.
References
Agency for Healthcare Research and Quality. (2021, October). Quality and patient safety resources. Ahrq.Gov. https://www.ahrq.gov/patient-safety/resources/index.html
Pickham, D., Berte, N., Pihulic, M., Valdez, A., Mayer, B., & Desai, M. (2018). Effect of a wearable patient sensor on care delivery for preventing pressure injuries in acutely ill adults: A pragmatic randomized clinical trial (LS-HAPI study). International Journal of Nursing Studies, 80, 12–19. https://doi.org/10.1016/j.ijnurstu.2017.12.012
Renganathan, B. S., Nagaiyan, S., Preejith, S. P., Gopal, S., Mitra, S., & Sivaprakasam, M. (2019). Effectiveness of a continuous patient position monitoring system in improving hospital turn protocol compliance in an ICU: A multiphase multisite study in India. Journal of the Intensive Care Society, 20(4), 309–315. https://doi.org/10.1177/1751143718804682
Schutt, S. C., Tarver, C., & Pezzani, M. (2018). Pilot study: Assessing the effect of continual position monitoring technology on compliance with patient turning protocols. Nursing Open, 5(1), 21–28. https://doi.org/10.1002/nop2.105
Sharp, C. A., Schulz Moore, J. S., & McLaws, M.-L. (2019). Two-hourly repositioning for prevention of pressure ulcers in the elderly: Patient safety or elder abuse? Journal of Bioethical Inquiry, 16(1), 17–34. https://doi.org/10.1007/s11673-018-9892-3
NURS 6051 Module 3: Data-Information-Knowledge-Wisdom (DIKW) (Week 5)
Discussion: Big Data Risks and Rewards
When you wake in the morning, you may reach for your cell phone to reply to a few texts or email messages that you missed overnight. On your drive to work, you may stop to refuel your car. Upon your arrival, you might swipe a key card at the door to gain entrance to the facility. And before finally reaching your workstation, you may stop by the cafeteria to purchase a coffee.
From the moment you wake, you are in fact a data-generation machine. Each use of your phone, every transaction you make using a debit or credit card, even your entrance to your place of work, creates data. It begs the question: How much data do you generate each day? Many studies have been conducted on this, and the numbers are staggering: Estimates suggest that nearly 1 million bytes of data are generated every second for every person on earth.
As the volume of data increases, information professionals have looked for ways to use big data—large, complex sets of data that require specialized approaches to use effectively. Big data has the potential for significant rewards—and significant risks—to healthcare. In this Discussion, you will consider these risks and rewards.
To Prepare:
- Review the Resources and reflect on the web article Big Data Means Big Potential, Challenges for Nurse Execs.
- Reflect on your own experience with complex health information access and management and consider potential challenges and risks you may have experienced or observed.
By Day 3 of Week 5
Post a description of at least one potential benefit of using big data as part of a clinical system and explain why. Then, describe at least one potential challenge or risk of using big data as part of a clinical system and explain why. Propose at least one strategy you have experienced, observed, or researched that may effectively mitigate the challenges or risks of using big data you described. Be specific and provide examples.
By Day 6 of Week 5
Respond to at least two of your colleagues* on two different days by offering one or more additional mitigation strategies or further insight into your colleagues’ assessment of big data opportunities and risks.
NURS 6051 Module 4: Technologies Supporting Applied Practice and Optimal Patient Outcomes (Weeks 6-8)
Discussion: Healthcare Information Technology Trends
Throughout history, technological advancements have appeared for one purpose before finding applications elsewhere that lead to spikes in its usage and development. The internet, for example, was originally developed to share research before becoming a staple of work and entertainment.
But technology—new and repurposed—will undoubtedly continue to be a driver of healthcare information. Informaticists often stay tuned to trends to monitor what the next new technology will be or how the next new idea for applying existing technology can benefit outcomes.
In this Discussion, you will reflect on your healthcare organization’s use of technology and offer a technology trend you observe in your environment.
To Prepare:
- Reflect on the Resources related to digital information tools and technologies.
- Consider your healthcare organization’s use of healthcare technologies to manage and distribute information.
- Reflect on current and potential future trends, such as use of social media and mobile applications/telehealth, Internet of Things (IoT)-enabled asset tracking, or expert systems/artificial intelligence, and how they may impact nursing practice and healthcare delivery.
By Day 3 of Week 6
Post a brief description of general healthcare technology trends, particularly related to data/information you have observed in use in your healthcare organization or nursing practice. Describe any potential challenges or risks that may be inherent in the technologies associated with these trends you described.
Then, describe at least one potential benefit and one potential risk associated with data safety, legislation, and patient care for the technologies you described.
Next, explain which healthcare technology trends you believe are most promising for impacting healthcare technology in nursing practice and explain why. Describe whether this promise will contribute to improvements in patient care outcomes, efficiencies, or data management. Be specific and provide examples.
By Day 6 of Week 6
Respond to at least two of your colleagues* on two different days, offering additional/alternative ideas regarding opportunities and risks related to the observations shared.
Assignment: Literature Review: The Use of Clinical Systems to Improve Outcomes and Efficiencies
New technology—and the application of existing technology—only appears in healthcare settings after careful and significant research. The stakes are high, and new clinical systems need to offer evidence of positive impact on outcomes or efficiencies.
Nurse informaticists and healthcare leaders formulate clinical system strategies. As these strategies are often based on technology trends, informaticists and others have then benefited from consulting existing research to inform their thinking.
In this Assignment, you will review existing research focused on the application of clinical systems. After reviewing, you will summarize your findings.
To Prepare:
- Review the Resources and reflect on the impact of clinical systems on outcomes and efficiencies within the context of nursing practice and healthcare delivery.
- Conduct a search for recent (within the last 5 years) research focused on the application of clinical systems. The research should provide evidence to support the use of one type of clinical system to improve outcomes and/or efficiencies, such as “the use of personal health records or portals to support patients newly diagnosed with diabetes.”
- Identify and select 4 peer-reviewed research articles from your research.
- For information about annotated bibliographies, visit https://academicguides.waldenu.edu/writingcenter/assignments/annotatedbibliographies
The Assignment: (4-5 pages not including the title and reference page)
In a 4- to 5-page paper, synthesize the peer-reviewed research you reviewed. Format your Assignment as an Annotated Bibliography. Be sure to address the following:
- Identify the 4 peer-reviewed research articles you reviewed, citing each in APA format.
- Include an introduction explaining the purpose of the paper.
- Summarize each study, explaining the improvement to outcomes, efficiencies, and lessons learned from the application of the clinical system each peer-reviewed article described. Be specific and provide examples.
- In your conclusion, synthesize the findings from the 4 peer-reviewed research articles.
- Use APA format and include a title page.
- Use the Safe Assign Drafts to check your match percentage before submitting your work.
Learning Resources
McGonigle, D., & Mastrian, K. G. (2021). Nursing informatics and the foundation of knowledge (4th ed.). Burlington, MA: Jones & Bartlett Learning.
- Cha
READ MORE >>
Discussion: specific evidence-based practice proposal topicORDER HERE FOR ORIGIN ...
Discussion: specific evidence-based practice proposal topic
ORDER HERE FOR ORIGINAL, ORDER THROUGH BOUTESSAY ON Discussion: specific evidence-based practice proposal topic
Identify a specific evidence-based practice proposal topic for a capstone project. Consider the clinical environment in which you are working or have recently worked.
project.docxUnformatted Attachment Preview
Capstone Project Topic Selection and Approval In collaboration with your approved course mentor, you will identify a specific evidence-based practice proposal topic for the capstone project. Consider the clinical environment in which you are working or have recently worked.The capstone project topic can be a clinical practice problem, an organizational issue, a quality improvement suggestion, a leadership initiative, or an educational need appropriate to your area of interest and your practice immersion (practicum) setting.Examples of the integration of community health, leadership, and EBP can be found on the “Educational and Community-Based Programs” page of the Healthy People 2020 website. Write a 500-750 word description of your proposed capstone project topic.Make sure to include the following: 1. The problem, issue, suggestion, initiative, or educational need that will be the focus of the project2. The setting or context in which the problem, issue, suggestion, initiative, or educational need can be observed.3. A description providing a high level of detail regarding the problem, issue, suggestion, initiative, or educational need.4. Impact of the problem, issue, suggestion, initiative, or educational need on the work environment, the quality of care provided by staff, and patient outcomes.5. Significance of the problem, issue, suggestion, initiative, or educational need and its implications to nursing.6. A proposed solution to the identified project topic. You are required to retrieve and assess a minimum of 8 peer-reviewed articles. Plan your time accordingly to complete this assignment. Prepare this assignment according to the guidelines in the APA Style Guide in the Student Success Center.An abstract is not required. You are required to submit this assignment to LopesWrite. Please refer to the directions in the Student Success CenterDiscussion: specific evidence-based practice proposal topic Instructions
You must proofread your paper. But do not strictly rely on your computer’s spell-checker and grammar-checker; failure to do so indicates a lack of effort on your part and you can expect your grade to suffer accordingly. Papers with numerous misspelled words and grammatical mistakes will be penalized.
Read over your paper – in silence and then aloud – before handing it in and make corrections as necessary. Often it is advantageous to have a friend proofread your paper for obvious errors. Handwritten corrections are preferable to uncorrected mistakes.
Use a standard 10 to 12 point (10 to 12 characters per inch) typeface. Smaller or compressed type and papers with small margins or single-spacing are hard to read. It is better to let your essay run over the recommended number of pages than to try to compress it into fewer pages.
Likewise, large type, large margins, large indentations, triple-spacing, increased leading (space between lines), increased kerning (space between letters), and any other such attempts at “padding” to increase the length of a paper are unacceptable, wasteful of trees, and will not fool your professor.
The paper must be neatly formatted, double-spaced with a one-inch margin on the top, bottom, and sides of each page. When submitting hard copy, be sure to use white paper and print out using dark ink. If it is hard to read your essay, it will also be hard to follow your argument.
ADDITIONAL INSTRUCTIONS FOR THE CLASS
Discussion Questions (DQ)
- Initial responses to the DQ should address all components of the questions asked, include a minimum of one scholarly source, and be at least 250 words.
- Successful responses are substantive (i.e., add something new to the discussion, engage others in the discussion, well-developed idea) and include at least one scholarly source.
- One or two sentence responses, simple statements of agreement or “good post,” and responses that are off-topic will not count as substantive. Substantive responses should be at least 150 words.
- I encourage you to incorporate the readings from the week (as applicable) into your responses.
Weekly Participation
- Your initial responses to the mandatory DQ do not count toward participation and are graded separately.
- In addition to the DQ responses, you must post at least one reply to peers (or me) on three separate days, for a total of three replies.
- Participation posts do not require a scholarly source/citation (unless you cite someone else’s work).
- Part of your weekly participation includes viewing the weekly announcement and attesting to watching it in the comments. These announcements are made to ensure you understand everything that is due during the week.
APA Format and Writing Quality
- Familiarize yourself with APA format and practice using it correctly. It is used for most writing assignments for your degree. Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for APA paper templates, citation examples, tips, etc. Points will be deducted for poor use of APA format or absence of APA format (if required).
- Cite all sources of information! When in doubt, cite the source. Paraphrasing also requires a citation.
- I highly recommend using the APA Publication Manual, 6th edition.
Use of Direct Quotes
- I discourage overutilization of direct quotes in DQs and assignments at the Masters’ level and deduct points accordingly.
- As Masters’ level students, it is important that you be able to critically analyze and interpret information from journal articles and other resources. Simply restating someone else’s words does not demonstrate an understanding of the content or critical analysis of the content.
- It is best to paraphrase content and cite your source.
LopesWrite Policy
- For assignments that need to be submitted to LopesWrite, please be sure you have received your report and Similarity Index (SI) percentage BEFORE you do a “final submit” to me.
- Once you have received your report, please review it. This report will show you grammatical, punctuation, and spelling errors that can easily be fixed. Take the extra few minutes to review instead of getting counted off for these mistakes.
- Review your similarities. Did you forget to cite something? Did you not paraphrase well enough? Is your paper made up of someone else’s thoughts more than your own?
- Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for tips on improving your paper and SI score.
Late Policy
- The university’s policy on late assignments is 10% penalty PER DAY LATE. This also applies to late DQ replies.
- Please communicate with me if you anticipate having to submit an assignment late. I am happy to be flexible, with advance notice. We may be able to work out an extension based on extenuating circumstances.
- If you do not communicate with me before submitting an assignment late, the GCU late policy will be in effect.
- I do not accept assignments that are two or more weeks late unless we have worked out an extension.
- As per policy, no assignments are accepted after the last day of class. Any assignment submitted after midnight on the last day of class will not be accepted for grading.
Communication
Communication is so very important. There are multiple ways to communicate with me:
- Questions to Instructor Forum: This is a great place to ask course content or assignment questions. If you have a question, there is a good chance one of your peers does as well. This is a public forum for the class.
- Individual Forum: This is a private forum to ask me questions or send me messages. This will be checked at least once every 24 hours.
READ MORE >>
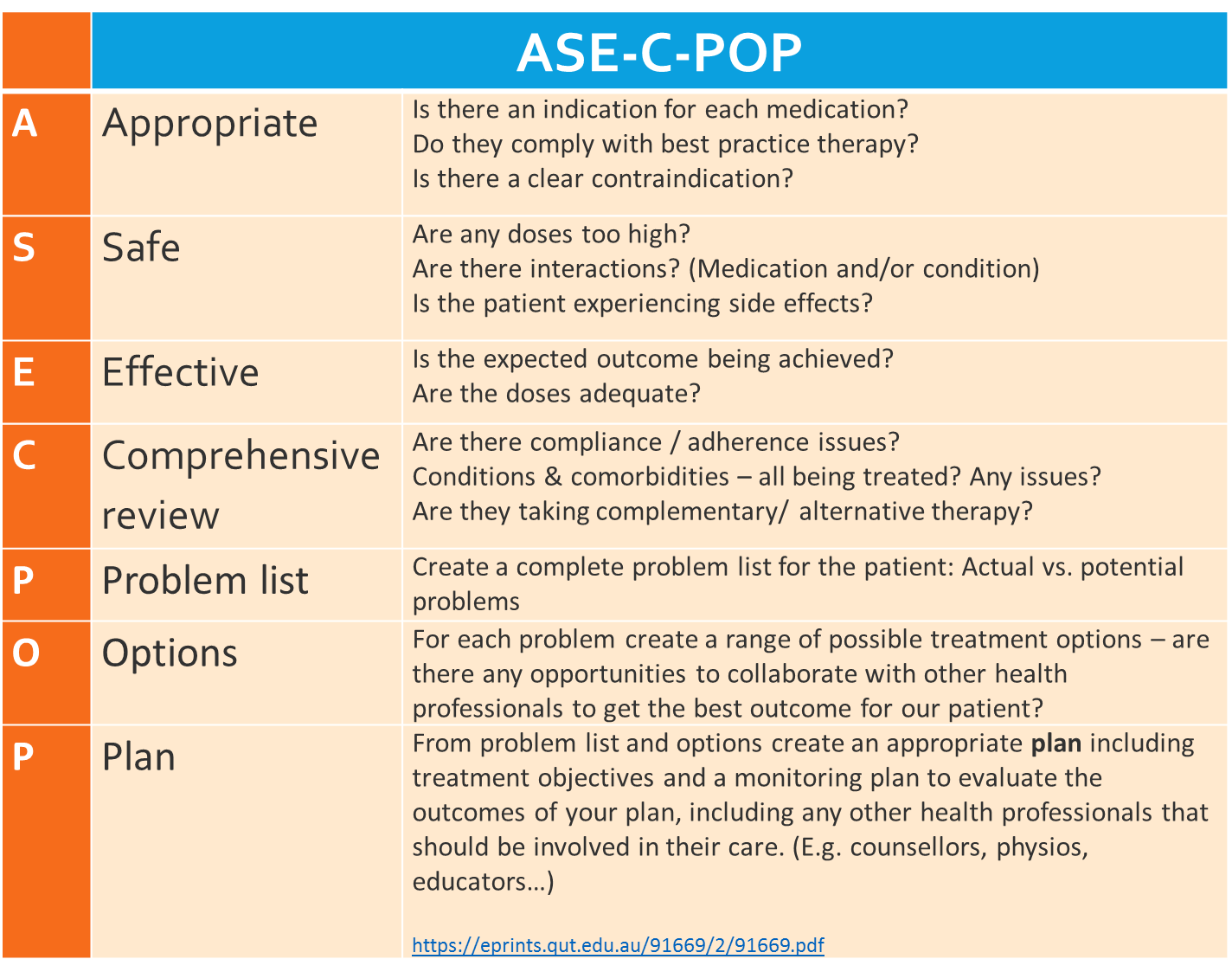
Discussion Using the ASE-C-POP frameworkDiscussion Using the ASE-C-POP framework ...
Discussion Using the ASE-C-POP framework
Discussion Using the ASE-C-POP framework
PATIENT CASE STUDY:
You will research and identify any actual/potential medication issues and create a plan to solve these issues using the ASE-C-POP framework. It is suggested you read the following article, as it will assist you in understanding the aspects of this framework:
https://qut.rl.talis.com/items/2DADDE09-B143-78C6-2FD0-54275D2C0DA6.html?referrer=%2Fsections%2FF9931B3E-072E-4248-1099-3E5A6A9E027D.html%3Fembed%3Dtrue%23item-2DADDE09-B143-78C6-2FD0-54275D2C0DA6
Also, see the next page for further guidelines on what ASE-C-POP headings refer to:
ORDER THROUGH BOUTESSAY
You must proofread your paper. But do not strictly rely on your computer’s spell-checker and grammar-checker; failure to do so indicates a lack of effort on your part and you can expect your grade to suffer accordingly. Papers with numerous misspelled words and grammatical mistakes will be penalized.
Read over your paper – in silence and then aloud – before handing it in and make corrections as necessary. Often it is advantageous to have a friend proofread your paper for obvious errors. Handwritten corrections are preferable to uncorrected mistakes.
Use a standard 10 to 12-point (10 to 12 characters per inch) typeface. Smaller or compressed type and papers with small margins or single-spacing are hard to read. It is better to let your essay run over the recommended number of pages than to try to compress it into fewer pages.
Likewise, large type, large margins, large indentations, triple-spacing, increased leading (space between lines), increased kerning (space between letters), and any other such attempts at “padding” to increase the length of a paper are unacceptable, wasteful of trees, and will not fool your professor.
The paper must be neatly formatted, double-spaced with a one-inch margin on the top, bottom, and sides of each page. When submitting hard copy, be sure to use white paper and print out using dark ink. If it is hard to read your essay, it will also be hard to follow your argument.
ADDITIONAL INSTRUCTIONS FOR THE CLASS
Discussion Questions (DQ)
Initial responses to the DQ should address all components of the questions asked, include a minimum of one scholarly source, and be at least 250 words.
Successful responses are substantive (i.e., add something new to the discussion, engage others in the discussion, well-developed idea) and include at least one scholarly source.
One or two sentence responses, simple statements of agreement or “good post,” and responses that are off-topic will not count as substantive. Substantive responses should be at least 150 words.
I encourage you to incorporate the readings from the week (as applicable) into your responses.
Weekly Participation
Your initial responses to the mandatory DQ do not count toward participation and are graded separately.
In addition to the DQ responses, you must post at least one reply to peers (or me) on three separate days, for a total of three replies.
Participation posts do not require a scholarly source/citation (unless you cite someone else’s work).
Part of your weekly participation includes viewing the weekly announcement and attesting to watching it in the comments. These announcements are made to ensure you understand everything that is due during the week.
APA Format and Writing Quality
Familiarize yourself with APA format and practice using it correctly. It is used for most writing assignments for your degree. Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for APA paper templates, citation examples, tips, etc. Points will be deducted for poor use of APA format or absence of APA format (if required).
Cite all sources of information! When in doubt, cite the source. Paraphrasing also requires a citation.
I highly recommend using the APA Publication Manual, 6th edition.
Use of Direct Quotes
I discourage overutilization of direct quotes in DQs and assignments at the Masters’ level and deduct points accordingly.
As Masters’ level students, it is important that you be able to critically analyze and interpret information from journal articles and other resources. Simply restating someone else’s words does not demonstrate an understanding of the content or critical analysis of the content.
It is best to paraphrase content and cite your source.
LopesWrite Policy
For assignments that need to be submitted to LopesWrite, please be sure you have received your report and Similarity Index (SI) percentage BEFORE you do a “final submit” to me.
Once you have received your report, please review it. This report will show you grammatical, punctuation, and spelling errors that can easily be fixed. Take the extra few minutes to review instead of getting counted off for these mistakes.
Review your similarities. Did you forget to cite something? Did you not paraphrase well enough? Is your paper made up of someone else’s thoughts more than your own?
Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for tips on improving your paper and SI score.
Late Policy
The university’s policy on late assignments is 10% penalty PER DAY LATE. This also applies to late DQ replies.
Please communicate with me if you anticipate having to submit an assignment late. I am happy to be flexible, with advance notice. We may be able to work out an extension based on extenuating circumstances.
If you do not communicate with me before submitting an assignment late, the GCU late policy will be in effect.
I do not accept assignments that are two or more weeks late unless we have worked out an extension.
As per policy, no assignments are accepted after the last day of class. Any assignment submitted after midnight on the last day of class will not be accepted for grading.
Communication
Communication is so very important. There are multiple ways to communicate with me:
Questions to Instructor Forum: This is a great place to ask course content or assignment questions. If you have a question, there is a good chance one of your peers does as well. This is a public forum for the class.
Individual Forum: This is a private forum to ask me questions or send me messages. This will be checked at least once every 24 hours.
READ MORE >>
BUS411 UNIT 3 DISCUSSION- Virginia Mason HospitalORDER NOW FOR PLAGIARISM FREE N ...
BUS411 UNIT 3 DISCUSSION- Virginia Mason Hospital
ORDER NOW FOR PLAGIARISM FREE NURSING PAPERS ON DISCUSSION- Virginia Mason Hospital
Virginia Mason Hospital
Review the closing case on Virginia Mason Hospital at the end of Chapter 4 in your textbook. Post your answers to the following questions on the discussion board. (At least one substantive paragraph on each question required, plus at least two comments on classmates’ posts. Copy each question with your answer.) DISCUSSION- Virginia Mason Hospital
- What do you think were the underlying reasons for the performance problems that Virginia Mason Hospital was encountering in the early 2000s?
- Which of the four building blocks of competitive advantage did lean production techniques help improve at Virginia Mason? DISCUSSION- Virginia Mason Hospital
- What do you think was the key to the apparently successful implementation of lean production techniques at Virginia Mason?
- Lean production was developed at a manufacturing firm, Toyota, yet it is being applied in this case at a hospital. What does that tell you about the nature of the lean production philosophy for performance improvement?
You must proofread your paper. But do not strictly rely on your computer’s spell-checker and grammar-checker; failure to do so indicates a lack of effort on your part and you can expect your grade to suffer accordingly DISCUSSION- Virginia Mason Hospital.
Papers with numerous misspelled words and grammatical mistakes will be penalized. Read over your paper – in silence and then aloud – before handing it in and make corrections as necessary. Often it is advantageous to have a friend proofread your paper for obvious errors. Handwritten corrections are preferable to uncorrected mistakes.
Use a standard 10 to 12 point (10 to 12 characters per inch) typeface. Smaller or compressed type and papers with small margins or single-spacing are hard to read. It is better to let your essay run over the recommended number of pages than to try to compress it into fewer pages DISCUSSION- Virginia Mason Hospital.
Likewise, large type, large margins, large indentations, triple-spacing, increased leading (space between lines), increased kerning (space between letters), and any other such attempts at “padding” to increase the length of a paper are unacceptable, wasteful of trees, and will not fool your professor.
The paper must be neatly formatted, double-spaced with a one-inch margin on the top, bottom, and sides of each page. When submitting hard copy, be sure to use white paper and print out using dark ink. If it is hard to read your essay, it will also be hard to follow your argument DISCUSSION- Virginia Mason Hospital.
ADDITIONAL INSTRUCTIONS FOR THE CLASS
Discussion Questions (DQ)
Initial responses to the DQ should address all components of the questions asked, include a minimum of one scholarly source, and be at least 250 words.
Successful responses are substantive (i.e., add something new to the discussion, engage others in the discussion, well-developed idea) and include at least one scholarly source.
One or two sentence responses, simple statements of agreement or “good post,” and responses that are off-topic will not count as substantive. Substantive responses should be at least 150 words.
I encourage you to incorporate the readings from the week (as applicable) into your responses.
Weekly Participation
Your initial responses to the mandatory DQ do not count toward participation and are graded separately.
In addition to the DQ responses, you must post at least one reply to peers (or me) on three separate days, for a total of three replies.
Participation posts do not require a scholarly source/citation (unless you cite someone else’s work).
Part of your weekly participation includes viewing the weekly announcement and attesting to watching it in the comments. These announcements are made to ensure you understand everything that is due during the week DISCUSSION- Virginia Mason Hospital.
APA Format and Writing Quality
Familiarize yourself with APA format and practice using it correctly. It is used for most writing assignments for your degree. Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for APA paper templates, citation examples, tips, etc. Points will be deducted for poor use of APA format or absence of APA format (if required).
Cite all sources of information! When in doubt, cite the source. Paraphrasing also requires a citation.
I highly recommend using the APA Publication Manual, 6th edition DISCUSSION- Virginia Mason Hospital.
Use of Direct Quotes
I discourage overutilization of direct quotes in DQs and assignments at the Masters’ level and deduct points accordingly.
As Masters’ level students, it is important that you be able to critically analyze and interpret information from journal articles and other resources.
Simply restating someone else’s words does not demonstrate an understanding of the content or critical analysis of the content.
It is best to paraphrase content and cite your source. DISCUSSION- Virginia Mason Hospital
LopesWrite Policy
For assignments that need to be submitted to LopesWrite, please be sure you have received your report and Similarity Index (SI) percentage BEFORE you do a “final submit” to me.
Once you have received your report, please review it. This report will show you grammatical, punctuation, and spelling errors that can easily be fixed. Take the extra few minutes to review instead of getting counted off for these mistakes DISCUSSION- Virginia Mason Hospital.
Review your similarities. Did you forget to cite something? Did you not paraphrase well enough? Is your paper made up of someone else’s thoughts more than your own?
Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for tips on improving your paper and SI score.
Late Policy
The university’s policy on late assignments is 10% penalty PER DAY LATE. This also applies to late DQ replies.
Please communicate with me if you anticipate having to submit an assignment late. I am happy to be flexible, with advance notice. We may be able to work out an extension based on extenuating circumstances.
If you do not communicate with me before submitting an assignment late, the GCU late policy will be in effect DISCUSSION- Virginia Mason Hospital.
I do not accept assignments that are two or more weeks late unless we have worked out an extension.
As per policy, no assignments are accepted after the last day of class. Any assignment submitted after midnight on the last day of class will not be accepted for grading.
Communication
Communication is so very important. There are multiple ways to communicate with me:
Questions to Instructor Forum: This is a great place to ask course content or assignment questions. If you have a question, there is a good chance one of your peers does as well. This is a public forum for the class.
DISCUSSION- Virginia Mason Hospital
Individual Forum: This is a private forum to ask me questions or send me messages. This will be checked at least once every 24 hours.
READ MORE >>
Discussions Hanging with Hailey Case StudyDiscussions Hanging with Hailey Case S ...
Discussions Hanging with Hailey Case Study
Discussions Hanging with Hailey Case Study
Each DQ question needs a reference and it must be citied in citation.
Watch the “Getting Back to Shakopee” video or the “Hanging with Hailey” case study video located in the Topic 5 folder in MindTap. After viewing the video, address the following:Discussions: “Hanging with Hailey” Case Study Discussions Hanging with Hailey Case Study
According to Chapter 8 in the textbook, assessment is used to gather information to create a coherent picture of the client. Identify how the client in the selected video is functioning within the various types in intrapersonal systems. Explain why it is important for a case manager to interpret the meaning of various client functions when developing a treatment plan.
What is one thing you know about Assessment?
Now that you have created the scenario for your hypothetical “client” for the intake interview assignment due in Topic 7, explain how you developed the scenario for your hypothetical “client.” What is the presenting problem and the current level of functioning? Was the client referred or seeking treatment on their own? Why is it important to know this information? Propose some engagement strategies you plan to use in your questioning techniques. Discussions Hanging with Hailey Case Study
SOC 449 Week 1 Social Phenomena Sample Essay
A social phenomenon can be defined as behavior that influences or is influenced by a client. When dealing with a client it is important to understand their behavior and why they are behaving like that. In this essay, the social phenomenons apparent in the video, “Home for the Holidays” will be explained.
As well as theories a social worker needs to be familiar with in order to help a client in their situation. This essay will also include the ways a social worker can use the theories to help the client work through their social phenomena and identify the appropriate principles that align with ethical practice in the video “Home for the Holidays”. Discussions Hanging with Hailey Case Study
Social Phenomenons that were apparent and presented to the social worker, in this case, were the couple trying to figure out where they should spend the holidays at. Ana doesn’t feel comfortable at Jackie’s house because she feels Jackie’s family isn’t as welcome of the fact they are gay. Ana asks why should she have to compromise herself for Jackie’s family. Discussions Hanging with Hailey Case Study
Jackie’s behavior towards going home is a little selfish because she doesn’t want her family to kick her out because she is gay. However, Ana is trying to explain to Jackie that if she talks to her family about being gay they are more likely to be more open to the idea of them as a couple Discussions Hanging with Hailey Case Study.
A social worker should be familiar with the psychosocial theory, systems theory, Pargament’s theory of religious coping, and lastly be comfortable with the ecological systems model. The psychosocial theory, “focuses on the ways that individuals are shaped by and react to their social environment” (Campbellsville, 2019). This theory can help the client work through their social phenomenas by showing them the social environment is having a negative or positive effect on their behavior and how they are being shaped.
An example from the video can be when Jackie is talking about the environment she grew up in and Ana points out how she is so much like her family. She is like her family because she grew up surrounded by them. Systems theory, “states that behavior is influenced by a variety of factors that work together as a system” (Campbellsville, 2019). This theory can be used by the social worker to figure out the factors that are working together to influence the client’s behavior Discussions Hanging with Hailey Case Study.
Pargament’s theory of religious coping may be another theory a social worker should be familiar with as it might help people who are dealing with tough issues find their answers in religion. This theory has five major functions, “to discover meaning, to garner control, to acquire comfort by virtue of closeness to God, to achieve closeness with others and to transform life” (Xi, 2016). Lastly, it may be helpful for a social worker to understand a client’s ecological systems model.
This model makes, “a close conceptual fit with the “person-in-environment” perspective that dominated social work…” (Hepworth, Rooney, Rooney, & Strom-Godfried, 2016). By using the ecological systems model the social worker will be able to understand the client’s background and their surrounding environment.
The NASW Code of Ethics, “is intended to serve as a guide to the everyday professional conduct of social workers” (NASW, 2020). There are six values in the NASW Code of Ethics which include, service, social justice, dignity and worth of a person, importance of human relationship, integrity and, competence Discussions Hanging with Hailey Case Study. In this video “Home for the Holidays”, the principles that align with ethical practice in this case study include service, social justice, the importance of human relationship, and integrity.
The first service is important in this case because a social worker’s primary goal is to help people in need and address any social problems they are dealing with. Next social justice is important in this case because the couple is part of a discriminated group Discussions Hanging with Hailey Case Study. This case also aligns with the principle of the importance of human relationships. The couple was sacrificing their relationship for other relationships, causing a weak relationship between Ana and Jackie.
The social worker was able to see that and thought of ways to help make their relationship stronger. Lastly, integrity, the social worker behaved in a trustworthy manner and communicated openly to the clients about what would and wouldn’t be shared Discussions Hanging with Hailey Case Study.
Social workers need to be able to identify how social contractions influence a client’s life. Each client will have different ways of expressing social phenomenas happening in their life and it is important to understand their behavior and why they are behaving like that.
Discussions Hanging with Hailey Case Study References
- Campbellsville. (2019, July 29). 5 Social Work Theories That Inform Practice. Retrieved from https://online.campbellsville.edu/social-work/social-work-theories/
- Hepworth, D. H., Rooney, R. H., Rooney, G. D., & Strom-Godfried, K. (2016). Direct social work practice: Theory and skills (10th ed.). Boston, MA: Cengage. ISBN-13: 9781305833803.URL:http://www.gcumedia.com/digital-resources/cengage/2016/direct-social-work-practice_theory-and-skills_ebook_10e.php
- NASW. (2020). About. Retrieved from https://www.socialworkers.org/about/ethics/code-of-ethics/code-of-ethics-english
- Xu, J. (2016). Pargament’s theory of religious coping: Implications for spiritually sensitive social work practice. British Journal of Social Work, 46(5), 1394–1410. https://doi-org.lopes.idm.oclc.org/10.1093/bjsw/bcv080
Discussions Hanging with Hailey Case Study
READ MORE >>
SOC 449 Week 1 Discussions Working with Yan Ping Paper GCUDiscussions Working wi ...
SOC 449 Week 1 Discussions Working with Yan Ping Paper GCU
Discussions Working with Yan Ping Paper
Access and view the “Working with Yan Ping” video located in the Topic 1 folder in MindTap. After you view the video, complete the following: Discussions Working with Yan Ping Paper
In your response, explain the following from the video:
- Presented problem
- Identified problem
- Social Phenomena present
- Cultural issues introduced
- What might be a possible solution to the identified problem using practice theories and interventions? Social work requires ethical and professional behavior. Explain if the social worker in this video displayed ethical behavior. Provide an example of both: ethical and professional behavior Discussions Working with Yan Ping Paper.
Read the case example on page 25 in Chapter 2 of the textbook. Identify the phases of the helping process in this particular case study. Explain if the case worker followed the helping process sufficiently or if an element within a phase was missing. What were the different approaches between the two social workers and why? Discussions Working with Yan Ping Paper
ORDER COMPREHENSIVE SOLUTION PAPERS ON Discussions: “Working with Yan Ping” Paper
SOC 449 Week 1 Social Phenomena Sample Essay
A social phenomenon can be defined as behavior that influences or is influenced by a client. When dealing with a client it is important to understand their behavior and why they are behaving like that. In this essay, the social phenomenons apparent in the video, “Home for the Holidays” will be explained.
As well as theories a social worker needs to be familiar with in order to help a client in their situation. This essay will also include the ways a social worker can use the theories to help the client work through their social phenomena and identify the appropriate principles that align with ethical practice in the video “Home for the Holidays”. Discussions Working with Yan Ping Paper
Social Phenomenons that were apparent and presented to the social worker, in this case, were the couple trying to figure out where they should spend the holidays at. Ana doesn’t feel comfortable at Jackie’s house because she feels Jackie’s family isn’t as welcome of the fact they are gay. Ana asks why should she have to compromise herself for Jackie’s family.
Jackie’s behavior towards going home is a little selfish because she doesn’t want her family to kick her out because she is gay. However, Ana is trying to explain to Jackie that if she talks to her family about being gay they are more likely to be more open to the idea of them as a couple Discussions Working with Yan Ping Paper.
A social worker should be familiar with the psychosocial theory, systems theory, Pargament’s theory of religious coping, and lastly be comfortable with the ecological systems model. The psychosocial theory, “focuses on the ways that individuals are shaped by and react to their social environment” (Campbellsville, 2019).
This theory can help the client work through their social phenomenas by showing them the social environment is having a negative or positive effect on their behavior and how they are being shaped. An example from the video can be when Jackie is talking about the environment she grew up in and Ana points out how she is so much like her family.
She is like her family because she grew up surrounded by them. Systems theory, “states that behavior is influenced by a variety of factors that work together as a system” (Campbellsville, 2019). This theory can be used by the social worker to figure out the factors that are working together to influence the client’s behavior Discussions Working with Yan Ping Paper.
Pargament’s theory of religious coping may be another theory a social worker should be familiar with as it might help people who are dealing with tough issues find their answers in religion. This theory has five major functions, “to discover meaning, to garner control, to acquire comfort by virtue of closeness to God, to achieve closeness with others and to transform life” (Xi, 2016).
Lastly, it may be helpful for a social worker to understand a client’s ecological systems model. This model makes, “a close conceptual fit with the “person-in-environment” perspective that dominated social work…” (Hepworth, Rooney, Rooney, & Strom-Godfried, 2016) Discussions Working with Yan Ping Paper. By using the ecological systems model the social worker will be able to understand the client’s background and their surrounding environment.
The NASW Code of Ethics, “is intended to serve as a guide to the everyday professional conduct of social workers” (NASW, 2020). There are six values in the NASW Code of Ethics which include, service, social justice, dignity and worth of a person, importance of human relationship, integrity and, competence.
In this video “Home for the Holidays”, the principles that align with ethical practice in this case study include service, social justice, the importance of human relationship, and integrity. The first service is important in this case because a social worker’s primary goal is to help people in need and address any social problems they are dealing with.
Next social justice is important in this case because the couple is part of a discriminated group. This case also aligns with the principle of the importance of human relationships Discussions Working with Yan Ping Paper. The couple was sacrificing their relationship for other relationships, causing a weak relationship between Ana and Jackie.
The social worker was able to see that and thought of ways to help make their relationship stronger. Lastly, integrity, the social worker behaved in a trustworthy manner and communicated openly to the clients about what would and wouldn’t be shared.
Social workers need to be able to identify how social contractions influence a client’s life. Each client will have different ways of expressing social phenomenas happening in their life and it is important to understand their behavior and why they are behaving like that.
References on Discussions Working with Yan Ping Paper
- Campbellsville. (2019, July 29). 5 Social Work Theories That Inform Practice. Retrieved from https://online.campbellsville.edu/social-work/social-work-theories/
- Hepworth, D. H., Rooney, R. H., Rooney, G. D., & Strom-Godfried, K. (2016). Direct social work practice: Theory and skills (10th ed.). Boston, MA: Cengage. ISBN-13: 9781305833803.URL:http://www.gcumedia.com/digital-resources/cengage/2016/direct-social-work-practice_theory-and-skills_ebook_10e.php
- NASW. (2020). About. Retrieved from https://www.socialworkers.org/about/ethics/code-of-ethics/code-of-ethics-english
- Xu, J. (2016). Pargament’s theory of religious coping: Implications for spiritually sensitive social work practice. British Journal of Social Work, 46(5), 1394–1410. https://doi-org.lopes.idm.oclc.org/10.1093/bjsw/bcv080
Also Read:
HLT 306V Advanced Patient Care
Assignment Disseminating EBP
Assignment – Workplace Safety Initiative Proposal
Assessment Tool Worksheet Assignment Paper
Assignment Clarifying Research
READ MORE >>
Disruptive Innovation Transforms an Existing MarketDisruptive Innovation Transfo ...
Disruptive Innovation Transforms an Existing Market
Disruptive Innovation Transforms an Existing Market
Jessica has been a nurse practitioner for nearly two decades. She has been providing primary care services to home-bound and home-limited patients since 2013 with an organization known as MD2U in Evansville, Indiana. In viewing the documentary, The Invisible Patient, Jessica presented herself as a disruptive innovator.
According to Hamric, Hanson, Tracy, & O’Grady, “disruptive innovation transforms an existing market or creates a new market by making processes simpler and improving access” (2014). Jessica took pride in caring for individuals in the community facing challenges. In viewing the documentary, I saw many of them live in difficult situations. For many reasons, some cannot travel to see a clinician at a doctor’s office. They all had multiple chronic conditions, and all faced some form of poverty.
Jessica mentioned several times that only a handful of people are currently reviving primary health care in their homes. Jessica’s background was in renal and telemetry medicine at Yale New Haven Hospital. Before joining MD2U, she cared for the adult and geriatric population with dementia. She also spent a decade in traditional family practice before branching out.
If Jessica did not provide her services, many patients would have frequent hospital admissions or require long-term or skilled rehab services. During the documentary, Jessica displayed respect and empathy for her patients while delivering high-quality patient-centered care. Per Jessica, her services are also more cost-efficient for the patients, especially since they are on a fixed income.
The ethical dilemma that stuck with me most while watching the documentary was Jessica’s care for the 34-year male Roger Brown. He was diagnosed with muscular dystrophy at four years old. “Muscular dystrophy is a group of diseases that cause progressive weakness and loss of muscular mass” (“Muscular dystrophy,” 2018). According to “Muscular Dystrophy,” the genes are abnormal and mutate, interfering with the production of proteins needed to form healthy muscle (2018).
This disease is very common in young males. There is no cure, but medications and therapy can help manage symptoms and slow the course of the disease. The normal life expectancy is approximately twenty years; Roger exceeded this. Symptoms may include “frequent falls, waddling gait, walking on the toes, large calf muscles, muscle pain/stiffness and respiratory complications” (“Muscular dystrophy,” 2018).
The ethical dilemma faced here was informed consent, “Concerns that patients and their families have not been fully informed about there treatment or clinical prognosis is a common ethical concern for nurses” (“Muscular dystrophy,” 2018).
Patients often feel more comfortable asking a nurse to decipher what their doctor says because of comprehension, especially with end-of-life decision-making. In one part of the documentary, Jessica is faced with discussing end-of-life care with Roger and his mom due to the progression of his disease especially impacting his respiratory status.
Jessica’s conflict was Rogers’s age. Normally treating a person of his age, you would take aggressive measures. But regarding Rogers’s health, his EF is 20%, and he has fluid buildup, heart failure, kidney stones, and generalized pain.
He had multiple co-morbidities, and Jessica knew if his heart stopped beating, performing CPR to prolong his life would cause more harm to him. At first, Roger wanted to continue aggressive measures to continue his life if he could.
Jessica had to find another approach to assist Roger and his mother in understanding the progression of his disease. She helped him understand that he wasn’t getting better regardless of his treatment.
Aggressive measures and hospice/palliative care services are two different treatments. Jessica had difficulty discussing this because she knew Rogers’s time was near. She did a great job explaining to Roger and his mother what would happen once he transitioned.
Many people face difficult decisions regarding code status, hospice, and palliative care services in their lifetime. The end of life should be a smooth transition, but it is often difficult because people find it hard to accept.
ORDER THROUGH BOUTESSAY
One important factor that affects ethical decision-making is your belief system (Hamric, Hanson, Tracy, & O’Grady, 2014). Your life experiences may change your values Hamric, Hanson, Tracy, & O’Grady, 2014). My personal beliefs are in line with Jessica with this ethical dilemma. I feel that end-of-life patients should have pain and symptoms management.
I would also assist the patient and family through the dying and death process, so the anxiety and fear can be decreased, as Jessica did. Advocacy for the patient is key to me. Effective communication should occur for a person to give great end-of-life care appropriately.
Becoming an adult gerontology nurse practitioner, I will be the spokesperson for my patient and honor their rights and give them dignity. I will ensure my patients are informed on what advance directives and living wills are in case they ever cannot make a sound decision, and I wouldn’t want to put that burden on their loved ones.
Everyone should honor a patient’s wishes as it is not causing any harm. The tales will be eliminated through education on end-of-life, DNR, palliative care services, hospice services, and advance directives, and anxiety/fear will be decreased (Hamric, Hanson, Tracy, & O’Grady, 2014).
One mechanism to overcome barriers is recognizing patients’ needs and making
patients and families aware of additional services such as palliative care. It is for patients with life-threatening illnesses. “Patient have better quality of life and live longer and cost the health system less” with palliative care services (Perrin & Kazonowski, 2015). Barriers to palliative care consultation for patients in critical care include misunderstanding.
Some feel that palliative care undermines the focus on saving the patient’s life. Providers often have difficulty determining when critically ill patients are approaching the end of life, causing patients to die in pain.
According to Perrin & Kazonowski, palliative care is an approach that improves the quality of life of patients and their families facing problems associated with wildlife-threatening illnesses (2015). APNs can emphasize to families that symptom management care to the patient can improve a patient’s outcome.
When the dying process is detected earlier, comfort-focused treatment goals are initiated sooner. When appropriate, patients are moved to lower-intensity care sites (Perrin & Kazonowski, 2015). The length of stay in the intensive care unit decreases (Perrin & Kazonowski, 2015). The cost of care is reduced because realistic goals are established. Staff would receive support for patients and families.
The need for repeat admission could be reduced because treatment goals have been clarified. And lastly, with palliative care, the patient and families would have continuity of care with familiar faces because they would be followed from the hospital to skilled/long-term care or home.
READ MORE >>
Diversity and Health Assessments NURS 6512 Week 2 Example 1Enhancing Cultural Co ...
Diversity and Health Assessments NURS 6512 Week 2 Example 1
Enhancing Cultural Competence in Health Assessment
Cultural competence is a crucial aspect of nursing practice, especially in health assessments. Functional assessments and cultural and diversity awareness play a critical role in health assessments, contributing to the delivery of effective and patient-centered care. Understanding the significance of these elements is essential for healthcare professionals, particularly nurses. Functional assessments go beyond traditional medical evaluations, focusing on a patient’s ability to perform activities of daily living (Ball et al., 2018). This includes assessing mobility, self-care, communication, and cognitive functions.
Understanding a patient’s functional status provides a holistic perspective on their health and helps identify areas requiring intervention or support. Incorporating cultural and diversity awareness ensures that healthcare providers recognize the influence of cultural, spiritual, and lifestyle factors on an individual’s health. This holistic understanding allows for more accurate health assessments that consider the whole person within their cultural context.
Issues in Health Assessments
As a nurse, I have encountered various instances where the diversity of patients has played a crucial role in healthcare delivery. It is importance to recognize and address diversity issues in health assessments. These issues encompass socioeconomic, spiritual, lifestyle, and cultural factors, emphasizing the need for personalized and culturally sensitive care.
Considering Paloma Hernandez, a 26-year-old Spanish-speaking patient, several specific factors must be taken into account. Socioeconomically, her ability to access healthcare and afford medications might be influenced. Spiritually, cultural beliefs may impact her understanding of illness and treatment (Ball et al., 2018). Lifestyle factors, including diet and daily habits, could contribute to her abdominal pain.
Building a Culturally Sensitive Health History
To develop a health history for Paloma, sensitivity to her background, lifestyle, and culture is paramount. The five targeted questions that I would ask to gather comprehensive information and assess potential health risks are:
- Cultural and Spiritual Beliefs:
Can you share any cultural or spiritual beliefs that influence how you perceive your current health condition? This may include any home remedies or traditional practices you follow.
- Diet and Lifestyle:
Could you describe your typical daily diet and any specific cultural preferences in your food choices? Additionally, are there any lifestyle factors, such as work or daily activities, that might contribute to your abdominal pain?
- Family Involvement:
In your culture, how involved is the family in health-related decisions? Do you typically rely on family members for support or assistance with healthcare matters?
- Communication Preferences:
Considering the language barrier during the first visit, I want to ensure effective communication. Is there a preferred language for our interactions, and would you like any family member, like your daughter, to be involved in translation?
- Financial Considerations:
I understand that healthcare costs can be a concern. Are there any financial challenges or constraints that may impact your ability to follow through with recommended treatments or medications?
Challenges and Strategies for Communication
Language barriers between healthcare providers and patients can impede effective communication. To overcome this, implementing professional interpreters is a crucial strategy. By ensuring accurate transmission of information, professional interpreters enable a clearer understanding of the patient’s health concerns and treatment options. This approach fosters effective communication and helps build trust between the healthcare provider and the patient.
Variations in cultural norms may lead to misunderstandings or discomfort during communication. Nurses should engage in regular cultural sensitivity training. This equips them with the skills to navigate diverse communication styles, fostering mutual understanding and trust. By being aware of and respecting cultural differences, healthcare providers can create a more inclusive and patient-centered communication environment (Dains et al., 2019).
Differences in health literacy levels impact the patient’s comprehension of medical information. To empower patients with varying health literacy levels, nurses can provide written materials in the patient’s preferred language and use visual aids. This promotes health literacy, enabling patients to actively engage in their care and make informed decisions about their health.
Family involvement expectations differ across cultures, influencing decision-making processes. Respecting and incorporating cultural norms related to family involvement in healthcare discussions is a critical strategy. This ensures holistic care planning and decision-making, recognizing the importance of family dynamics in the patient’s healthcare journey.
Strategies for Effective Cross-Cultural Communication
Nurses can prioritize culturally sensitive questions during health assessments to gather pertinent information. This approach acknowledges the influence of cultural factors on health and provides a comprehensive understanding of the patient’s background (Dains et al., 2019). By tailoring assessments to the patient’s cultural context, nurses can better address the patient’s unique healthcare needs.
Utilizing active listening techniques and employing open-ended questions are effective communication strategies. These techniques encourage patients to share their perspectives and concerns, facilitating a deeper understanding of their unique cultural context (Coleman, 2019). By actively engaging with patients and allowing them to express themselves, nurses can build trust and enhance communication.
Paying attention to non-verbal cues, including body language and facial expressions, is crucial in cross-cultural communication. Interpreting non-verbal cues enhances the nurse’s ability to gauge the patient’s comfort levels and emotional state. This contributes to a more empathetic and patient-centered interaction, bridging the gap created by language and cultural differences.
Engaging in ongoing cultural competence training and self-reflection is a continuous and essential process. Continuous learning and self-awareness foster cultural competence, enabling nurses to adapt their practices to meet the evolving needs of diverse patient populations (Coleman, 2019). By embracing cultural competence as a lifelong commitment, healthcare providers can contribute to a more inclusive and equitable healthcare environment.
Conclusion
Cultural competence is integral to providing patient-centered care, particularly in health assessments. The case study of Paloma Hernandez emphasizes the importance of understanding cultural nuances, acknowledging diversity, and employing effective communication strategies. By incorporating targeted questions and employing culturally sensitive approaches, nurses can enhance their ability to assess and address the health needs of patients from diverse backgrounds.
Diversity and Health Assessments NURS 6512 References
Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2018). Seidel’s Guide to Physical Examination: An interprofessional approach. Mosby. https://www.amazon.com/Seidels-Guide-Physical-Examination-Interprofessional/dp/0323481957
Coleman, D. E. (2019). Evidence based nursing practice: The challenges of health care and cultural diversity. Journal of Hospital Librarianship, 19(4), 330–338. https://doi.org/10.1080/15323269.2019.1661734
Dains, J. E., Baumann, L. C., & Scheibel, P. (2019). Advanced Health Assessment and Clinical Diagnosis in Primary Care (6th ed.). Mosby. https://www.amazon.com/Advanced-Assessment-Clinical-Diagnosis-Primary-ebook/dp/B07M6FWXB3
Also read:
Assessment of Nutrition in Children NURS 6512
NURS 6512 Lab Assignment: Assessing the Abdomen Sample Paper
NURS 6512 Discussion: Assessing Musculoskeletal Pain Discussion Paper
NURS 6512 Assessment Tools and Diagnostic Tests in Adults and Children Case
DIVERSITY AND HEALTH ASSESSMENTS NURS 6512 WEEK 2 INSTRUCTIONS
 May 2012, Alice Randall wrote an article for The New York Times on the cultural factors that encouraged black women to maintain a weight above what is considered healthy. Randall explained—from her observations and her personal experience as a black woman—that many African-American communities and cultures consider women who are overweight to be more beautiful and desirable than women at a healthier weight. As she put it, “Many black women are fat because we want to be” (Randall, 2012).
May 2012, Alice Randall wrote an article for The New York Times on the cultural factors that encouraged black women to maintain a weight above what is considered healthy. Randall explained—from her observations and her personal experience as a black woman—that many African-American communities and cultures consider women who are overweight to be more beautiful and desirable than women at a healthier weight. As she put it, “Many black women are fat because we want to be” (Randall, 2012).
Randall’s statements sparked a great deal of controversy and debate; however, they emphasize an underlying reality in the healthcare field: different populations, cultures, and groups have diverse beliefs and practices that impact their health. Nurses and healthcare professionals should be aware of this reality and adapt their health assessment techniques and recommendations to accommodate diversity.
In this Discussion, you will consider different socioeconomic, spiritual, lifestyle, and other cultural factors that should be taken into considerations when building a health history for patients with diverse backgrounds. Your Instructor will assign a case study to you for this Discussion.
To prepare for Diversity and Health Assessments NURS 6512:
- Reflect on your experiences as a nurse and on the information provided in this week’s Learning Resources on diversity issues in health assessments.
- By Day 1 of this week, you will be assigned a case study by your Instructor. Note: Please see the “Course Announcements” section of the classroom for your case study assignment.
- Reflect on the specific socioeconomic, spiritual, lifestyle, and other cultural factors related to the health of the patient assigned to you.
- Consider how you would build a health history for the patient. What questions would you ask, and how would you frame them to be sensitive to the patient’s background, lifestyle, and culture? Develop five targeted questions you would ask the patient to build his or her health history and to assess his or her health risks.
- Think about the challenges associated with communicating with patients from a variety of specific populations. What strategies can you as a nurse employ to be sensitive to different cultural factors while gathering the pertinent information?
BY DAY 3 OF WEEK 2
Post an explanation of the specific socioeconomic, spiritual, lifestyle, and other cultural factors associated with the patient you were assigned. Explain the issues that you would need to be sensitive to when interacting with the patient, and why. Provide at least five targeted questions you would ask the patient to build his or her health history and to assess his or her health risks.
Note: For this Discussion, you are required to complete your initial post before you will be able to view and respond to your colleagues’ postings. Begin by clicking on the Reply button to complete your initial post. Remember, once you click on Post Reply, you cannot delete or edit your own posts and you cannot post anonymously. Please check your post carefully before clicking on Post Reply!
Read a selection of your colleagues’ responses.
BY DAY 6 OF WEEK 2
Respond on or before Day 6 on 2 different days to at least two of your colleagues who were assigned a different patient than you. Critique your colleague’s targeted questions, and explain how the patient might interpret these questions. Explain whether any of the questions would apply to your patient, and why.
LEARNING RESOURCES
Required Readings
- Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2023). Seidel’s guide to physical examination: An interprofessional approach (10th ed.). St. Louis, MO: Elsevier Mosby.
- Chapter 1, “Cultural Competency”
This chapter highlights the importance of cultural awareness when conducting health assessments. The authors explore the impact of culture on health beliefs and practices.
- Chapter 1, “Cultural Competency”
- Dains, J. E., Baumann, L. C., & Scheibel, P. (2019). Advanced health assessment and clinical diagnosis in primary care (6th ed.). St. Louis, MO: Elsevier Mosby.
Credit Line: Advanced Health Assessment and Clinical Diagnosis in Primary Care, 6th Edition by Dains, J.E., Baumann, L. C., & Scheibel, P. Copyright 2019 by Mosby. Reprinted by permission of Mosby via the Copyright Clearance Center.- Chapter 2, “Evidenced-Based Clinical Practice Guidelines”
- Centers for Disease Control and Prevention. (2020, October 21). Cultural competence in health and human servicesLinks to an external site.. Retrieved from https://npin.cdc.gov/pages/cultural-competence
This website discusses cultural competence as defined by the Centers for Disease Control and Prevention (CDC). Understanding the difference between cultural competence, awareness, and sensitivity can be obtained on this website. - United States Department of Human & Health Services. Office of Minority Health. (n.d.). A physician’s practical guide to culturally competent careLinks to an external site.. Retrieved June 10, 2019, from https://cccm.thinkculturalhealth.hhs.gov/
From the Office of Minority Health, this website offers CME and CEU credit and equips healthcare professionals with awareness, knowledge, and skills to better treat the increasingly diverse U.S. population they serve. - Coleman, D. E. (2019). Evidence based nursing practice: The challenges of health care and cultural diversityLinks to an external site.. Journal of Hospital Librarianship, 19(4), 330–338. https://doi.org/10.1080/15323269.2019.1661734
- Young, S., & Guo, K. L. (2016). Cultural diversity trainingLinks to an external site.. The Health Care Manager, 35(2), 94–102. https://doi.org/10.1097/hcm.0000000000000100
Required Media
Module 2 Introduction
Dr. Tara Harris reviews the overall expectations for Module 2. Consider how you will manage your time as you review your media and Learning Resources for your Discussion, Case Study Lab Assignment, and your DCE Assignment (3m).
TARA HARRIS: Hello. This is Dr. Harris. I’m your coordinator for Advanced Health Assessment. Today we will discuss Module 2, which includes both week 2 and 3. During these two weeks, we will discuss functional assessments and assessment diagnostic tools. You have several required readings and articles within this module. You also have a required media video, which will assist you in learning how to take a health history.
Your first Shadow Health overview should be conducted during this time. You will also be able to complete the lab components within Shadow Health. During week 2, your discussion board initial post is due by day 3, and your final responses are due by day 6. You should also began working on your overview of Shadow Health Clinical Experience. During week 3, you have
several assignments.
Assignment 1 is a case study assignment that will be assigned by your instructor. You will need to write three to four pages within this assignment, and this does not include your title and your reference page. This assignment is due for submission by day 6 of week 3.
Your assignment 2 during week 3 will be your first Shadow Health history assessment. Please review the guidelines for this assignment. Please review your grade and rubric. Please start reviewing Shadow Health so that you are familiar with what you need to do to pass the assignment. So during week 4, this is when your health history is due. Please complete the orientation and all the requirements for this assignment.
As mentioned earlier, please review your grade and rubric. Remember, you must also document within Shadow Health as part of your grade. We are requiring that you document your information or your provider note on a Word document and submit that. Please also remember that your digital clinical score that you submit via the lab pass is not your final score. Your final grade will be composed of two components, your digital clinical score, as well as your documentation.
You must pass this assignment with a total score of 80% or more in order to pass this course. You will not be allowed any more attempts after day 7. The late policy will apply for any late submissions. Please reach out to your instructor if you need any clarity, concerns, or further discussion. Thank you.
Functional Assessments and Cultural and Diversity Awareness in Health Assessment – Week 2 (10m)
DR. LACHANDA BROWN: Hello, everyone, and welcome to Advance Health Assessment. I’m Dr. LaChanda Brown, and I’m one of the contributing faculty members in the course. For week two, we will focus on functional assessments with cultural diversity awareness. By the end of the week, you should be able to analyze diversity considerations in health assessments and apply concept theories and principles as it relates to cultural diversity in health assessment.
So what is diversity in health care and why is it so important? As a health care provider, we should be diverse, if not more diverse than the patient’s base they are treating. This helps to ensure that no matter what, no matter who walks in that door, we can effectively communicate with them and better serve their needs. We can do this be being cultural sensitive. So what is cultural sensitivity and why is it important?
Cultural sensitivity is being aware that there are cultural differences and similarities between people without assigning them a value. There’s no right or wrong, there is no better or worse, and there is no positive or negative. Again, this allows us to be able to function in other cultures, being able to understand or try to relate to being able to be that detective as previously mentioned in week one to find the correct answers, to try to solve their health problem, or help to treat their problem.
Also being culturally diverse. Cultural diversity is about appreciating that the individuals
and society are made up of different groups. That have different interests, skills, talents. It also means that being culturally diverse is being aware that there are different religious beliefs other than yourself. You may not accept those. Different sexual orientations other than yourself, but you respect that. You may not have the same belief, but you respect that, and you are non-biased for us with treatment of that patient.
So with that being said, there is always some risk of problems if there is not diversity in healthcare. And one of the issues is communication breakdown. Oftentimes, we may have individuals that may come into our practice that may have a language barrier, a different philosophy, or different cultural norms. Trying to be able to communicate, to fully communicate the needs or the issues of that patient is very important.
Also being aware of sometimes people can have lack of healthcare diversity, or you can have
limited perspectives. You may have never been around someone that may speak a different language or may have a different sexual preference or a different religious belief. And again, being able to be aware that even though this is something that you’re not familiar with, being able to try and come up with the best plan for that patient and being non-biased.
By being culturally sensitive, it provides patient-desired care, provides empowerment of the patient. The patient is aware that you are sensitive to their needs, which gives them the ability to be able to communicate and relate what is going on with them to provide better health care. I’ve also attached a video, Understanding Cultural Diversity in Healthcare- the four C’s.
Please take a look at this video. It has some very important tips on how to understand cultural diversity. So again, for this week’s assignment, you will have a case study. With that case
study, you’re going to reflect on your experience as a nurse on the information that was provided in this week’s learning resource on diversity in health issues.
Please be aware of the socioeconomic, spiritual lifestyles and other cultural factors that may be considered. Consider how you will build a health history. Again, like we discussed previously in week one, what other concepts that you need to build a good health history? What type of questions you would ask? Think about challenges, sparse with communication, and ways that you can help to relieve those communication barriers.
So again, I want to still reiterate Shadow Health assignment. Shadow health– please purchase as soon as possible. You do not have an assignment due this week for Shadow Health, but I would suggest to go ahead and practice on Shadow Health. Please get familiar with the areas in Shadow Health. If you haven’t purchased it, like I said before, you can purchase it through Walden bookstore only. You will receive an email– a confirmation
email with a code.
You do not need a PIN number from your instructor for access in Shadow Health. There is also a Shadow Health video. Just information about Shadow Health and navigation. Also attached is the Shadow Health IT. If you ever have any issues with logging in or not being able to access Shadow Health, you can click on this link and it should connect you to Shadow Health. There’s a number as well as a website to be able to contact. And then just tips for us
with Shadow Health success, starting on day one and getting familiar with Shadow Health accessing it, and just getting in the mode of Shadow Health practicing.
I cannot stress that enough. Practice, practice, practice on Shadow Health. You must have at least an 80% on Shadow Health, on all your Shadow Health, which is a combination of your DCE score as well as your documentation notes. And on those links, it will tell you about how to document. You want to be aware of the documentation that is essential. What is subjective
versus objective data? Subjective is what the patient states, what is going on with them.
Objective data is what you see or what you hear, your physical examination. So you want to
make sure that you know what is going on with your patient as far as with Shadow
Health and as far as how to document Shadow Health. Again, you must have
a 80% total combined score in Shadow Health, which is a combination of your DC score list where’s your documentation notes. And there is a link on here that can tell you how to document in your notes in Shadow Health. Again, you will start working in Shadow Health in week three.
Your first assignment is not due until week four for Shadow Health, Tina Jones. But, like I stated previously, get started with Shadow Health as soon as possible. Do not wait till
the last minute. You can practice in Shadow Health as many times as you like on up
until day seven. After day seven, you will not be able to access and it would be counted off as
late, unless you have an excuse and you previously discussed it with your instructor. But please get started on Shadow Health and get familiar. Watch the video, be aware of the IT, successful tips, and documentation tutorial. Thank you.
- Walden University. (n.d.). Instructor feedback
Diversity and Health Assessments NURS 6512 – Enhancing Cultural Competence in Health Assessment Example 2
Diversity and Health Assessment
Individuals from racial and ethnic minority groups may speak English “less well” or “not at all” and are thus classified as Limited English Proficient (LEP). Because of their limited ability to communicate their health information, ethnic minorities are vulnerable to significant health disparities. As a result, healthcare providers must be culturally competent to care for such individuals. Paloma’s case, a 26-year-old Spanish-speaking female patient who presented to the clinic for the second time in two days with abdominal pain, demonstrates the cultural influence on health. An in-depth discussion of the socioeconomic, spiritual, lifestyle, and other cultural factors influencing the patient’s health is provided below.
Socioeconomic, Spiritual, Lifestyle, and Other Cultural Factors affecting the Patient’s Health Status
An individual’s socioeconomic status influences their ability to access and use healthcare services. Poverty, health insurance, education, and employment are all important socioeconomic factors influencing Hispanic health. One in every four Hispanics in the United States lives below the poverty line (CDC, 2020). Furthermore, approximately one-third of Hispanic immigrants who have been in the United States for more than ten years had a college degree in 2018 (Noe-Bustamante, 2020). As a result, only a few people, including Paloma, have the financial means to access healthcare services.
Spiritual beliefs also influence an individual’s health status. The majority of Hispanics are Christian Catholics who seek comfort and relief from life’s stresses through prayer (Johnson & Farquharson, 2019). They believe in praying to God or having faith as a coping strategy when they are sick. This, along with seeking medical attention, may help Paloma heal. In terms of lifestyle, both Hispanic men and women report a lower prevalence of regular physical activity (41.9%, 40.5%) than their non-Hispanic counterparts (52.3, 49.6), making them vulnerable to a variety of chronic illnesses (Bantham et al., 2021).
Furthermore, in 2020, 8.0% of Hispanic adults in the United States smoked cigarettes (CDC, 2022), and it is estimated that 9.5% will have alcohol dependence at some point in their lives (National Institute of Health, 2021); these are risk behaviors that increase the individual’s risk of developing chronic illnesses. As a result, for Paloma to maintain a healthy lifestyle, she should be advised on healthy lifestyle changes. Language is a potent cultural determinant of health as well. Language influences both how a patient communicates and how a clinician perceives health information (Dains et al., 2015; Melton et al., 2014). Being an LEP, she is accompanied by her younger bilingual daughter; however, this proxy reporting of symptoms may not depict the true illness of the patient and may explain why she visits the hospital twice in two days for the same illness.
Sensitive Issues while interacting with the Patient
The patient has been to the clinic two days in a row with similar complaints. She is accompanied by her younger bilingual daughter, who may not fully comprehend all of the details of her illness. One might wonder why the patient is not with an older person, such as her husband or older children, who appear to have a better perception of health. This patient may have marital problems or some form of discord, which a clinician should be aware of to design appropriate, helpful interventions. She was also discharged on Omeprazole but was told she could get it over the counter.
Could the patient afford the medication? This could explain why she is seeking care on the second day with worsening symptoms. Poverty rates among Hispanics in the United States are staggering, with one in every four living in poverty (CDC, 2020); this may explain Paloma’s inability to afford the drugs. In addition, I would be cautious about the language I use when addressing the patient. Park et al. (2018) recommend using simple pleasantries, clear explanations, and active listening when speaking with LEP individuals to build a bond with them. While history taking is an important aspect of health assessment, the clinician must understand the patient’s situation outside of the hospital to understand the nature of the patient’s illnesses.
Targeted Questions to build the Health History and to Assess Health Risks
- You state that you have abdominal pain; when was the onset?
- In which part of the abdomen is the pain located?
- What is the character of the pain, and are there aggravating or relieving factors?
- How severe is the pain, and does it occur at different times?
- Have you ever had peptic ulcer treatment?
- Do you consume alcoholic beverages or smoke cigarettes?
- Have you recently received NSAID therapy?
- Has any member of your family ever had an abdominal malignancy?
Conclusion
History taking and physical examination are critical assessment steps in healthcare. A clinician gains essential information from the history and physical examination that aids in making a diagnosis and, consequently, designing an appropriate treatment plan. However, challenges such as language barriers may arise during the initial patient assessment, resulting in a suboptimal assessment and treatment. Paloma, for example, is Spanish-speaking and comes in the company of her bilingual-speaking younger daughter. To solve the medical problems of LEP patients, clinicians may resort to alternatives such as enlisting the assistance of a translator.
Diversity and Health Assessments NURS 6512 References
Bantham, A., Taverno Ross, S. E., Sebastião, E., & Hall, G. (2021). Overcoming barriers to physical activity in underserved populations. Progress in Cardiovascular Diseases, 64, 64–71. https://doi.org/10.1016/j.pcad.2020.11.002
Centers for Disease Control and Prevention. (2020, January 3). Hispanic health. Centers for Disease Control and Prevention. https://www.cdc.gov/vitalsigns/hispanic-health/index.html
Centers for Disease Control and Prevention. (2022, August 9). Burden of cigarette use in the U.s. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/campaign/tips/resources/data/cigarette-smoking-in-united-states.html
Dains, J. E., Baumann, L. C., & Scheibel, P. (2019). Advanced Health Assessment & Clinical Diagnosis in Primary Care-E-Book. Elsevier Health Sciences. https://www.uk.elsevierhealth.com/advanced-health-assessment-clinical-diagnosis-in-primary
READ MORE >>
