Our Previous Samples
Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Refle ...
Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Reflection Video Example 1
Collaboration and Leadership Reflection
Hello everyone, my name is ………. And I will be presenting my perspective on interprofessional leadership and collaboration within the nursing practice space. Interprofessional collaboration encompasses an array of healthcare specialists with discrete skills, talents, and expertise to participate in patient care (Hlongwa & Rispel, 2021). Interprofessional collaboration is often used as a method of solving numerous healthcare problems and complex issues.
Interprofessional collaboration in healthcare has been associated with enormous benefits, including a reduction in medical errors, improvement of patient care and outcomes, rapid initiation of treatment, reduction of healthcare inefficiencies and costs, and improvement in staff relationships and job satisfaction (Hlongwa & Rispel, 2021).
However, effective collaboration necessitates effective leadership to influence and communicate change. This video will reflect on an interdisciplinary collaboration I engaged in, noting how it was successful and unsuccessful, the relationship between poor collaboration and management of human and financial resources, and leadership and collaboration strategies that can enhance the achievement of goals.
As a registered nurse working in preventive medicine, It was noted that there was an increase in hospitalization and morbidity related to sexually transmitted diseases and tuberculosis. Sexually transmitted diseases were mainly prevalent in adolescents and young adults, while tuberculosis spanned across all age groups but largely affected middle-aged to older adults. These conditions sounded an alarm as both conditions are preventable.
Consequently, an interprofessional collaboration team was formed that consisted of physicians, nurses, pharmacists, nutritionists, and community health workers to address these concerns. This team of specialists had several meetings and formulated a comprehensive individualized care management plan. This care plan was drafted following a series of conversations with the affected patients, and it consisted of patient education, active surveillance, and follow-up. The implementation of the care plan resulted in a significant reduction in cases of sexually transmitted diseases and TB as well as their related morbidity. Similarly, a significant reduction in healthcare costs was observed.
As part of this team, several factors contributed to the success. First was the selection of an appropriate team leader. A physician was selected who communicated the vision and the change initiative. The physician was effective as he had a vast background knowledge regarding sexually transmitted diseases and tuberculosis. As an effective leader, the physician spearheaded all functions of the team and ensured that all members of the interprofessional collaboration team were motivated and committed to change. Secondly is careful planning. The interprofessional team knew that the prosperity of this initiative was largely dependent on understanding and eliminating the initiating, precipitating, and maintaining factors.
For instance, sexually transmitted among adolescents is a public health concern and is usually a result of risky sexual behaviors precipitated by factors such as drug and alcohol abuse, social media, and peer pressure. Consequently, patient education was directed toward these factors. Additionally, the team communicated effectively. According to Schimith et al. (2021), effective communication is critical for any teamwork as it builds trust and ensures cohesiveness. Furthermore, the involvement of patients in decision-making led to the development of a change initiative that was vastly accepted, which increased the success of the team. Finally, the team deployed delegation of duties, reducing workload and encouraging all team members to remain positive and motivated.
However, the interprofessional team failed in some aspects. For instance, some team members failed to create a good rapport with patients and, therefore, could not truly identify and elicit information regarding the presence of sexually transmitted diseases in some adolescents. Similarly, some interprofessional collaboration team members initially misdiagnosed patients with TB as pneumonia patients due to similar presentation and failure to elicit comprehensive history, which delayed the initiation of treatment and increased the chances of spreading the infection. Finally, a lack of proper documentation was also observed, leading to a loss of follow-up. Consequently, the outcomes of the interprofessional collaboration could have been much better had the aforementioned weaknesses addressed.
Regarding the scenario in the Vila Health Activity, penurious and ineffective communication between the IT management and the nurses who were the utilizers of the computer system Healthix is evident. For example, nurses lament the program’s impervious nature and user unfriendliness. Furthermore, the recruitment of a coach is still ineffective as the medical staff still had trouble using the system following the completion of the course. This scenario is a true manifestation of the baseless allocation of human resources and financial mismanagement as a result of ineffective communication. Likewise, poor communication results in frustration, stress, mistrust, absenteeism, mistrust, and decreased productivity of the employees, hence unsuitable utilization of human resources (Wieke et al., 2021). Finally, poor communication precipitates poor decision-making and legal wrangles that may result in a waste of finances.
Leadership Strategies
Leadership strategies are crucial for the prosperity of any interprofessional collaboration. All leaders must enhance collaboration to achieve the most favorable outcomes in the healthcare industry. Numerous leadership strategies have been highlighted in the literature. Nevertheless, effective communication and teamwork are among the most vital leadership strategies that foster interprofessional collaboration. Schimith et al. (2021) define the role of effective communication as essential to building trust, a central prerequisite for all members of the interdisciplinary team.
Interdisciplinary teams consist of diverse individuals with abundant tasks and attributes; hence effective communication ensures the provision of comprehensive care and care coordination. For instance, research by Schimith et al. (2021) identified interprofessional communication as the key to interprofessional collaboration and effective care coordination in healthcare. Meanwhile, teamwork is a critical strategy for fostering interdisciplinary collaboration.
According to Skyberg and Innvaer (2020), most patients have different needs, which can only be accomplished comprehensively by a collection of talents and skills from heterogeneous healthcare providers. Finally, being open to change and innovation is a vital leadership strategy that stretches interprofessional collaboration. The Healthcare industry is ever-growing and dynamic, characterized by widespread research and innovative ideas from several stakeholders.
Additionally, change and innovation are fundamental to evidence-based practice and quality patient care. Therefore, leaders must identify problematic areas and encourage change to enhance the cohesiveness as well as the efficiency of their followers. Consequently, in an endeavor to enhance interdisciplinary collaboration, leaders must champion effective communication, teamwork, change, and innovation.
Collaboration Strategies
Leadership and collaboration strategies are more often than not difficult to separate. Collaboration intersects different individuals to function cohesively toward the attainment of a shared goal. This process entails strategies such as shared decision-making, delegation, and encouraging feedback. Shared decision-making enhances collaboration as team members feel and own the decisions made (Elwyn, 2021). Additionally, collaborative teams are composed of various individuals with different skills, backgrounds, talents, and knowledge.
Consequently, shared decision-making offers a structured way of incorporating evidence, values, and preferences (Elwyn, 2021). According to Elwyn (2021), this process supports conversations leading to informed decisions that are congruent with what matters most to patients and team members. On the other hand, delegation is the act of empowering one to act for another (Beckett et al., 2021). Beckett et al. (2021) highlight that delegation enhances collaboration only when principled. Elemental principles of the nursing delegation include the right person, the right task, the right circumstance, the right communication, and the right supervision.
Delegation ensures that healthcare professionals are not overwhelmed with tasks as they practice in areas of their expertise. In a study by Wagner (2018), delegation considerably contributed to collaboration, patient satisfaction, job satisfaction, and enhanced patient outcomes. According to Ramani et al. (2019), interdisciplinary collaboration is a vigorous process that is vulnerable to change periodically due to the variety of members. Consequently, incessantly seeking opinions and feedback from team members is cardinal to effective collaboration. Ramani et al. (2019) further encourage team leaders to incorporate positive feedback and address all issues of team members in the best possible way to maintain and enhance collaboration.
Conclusion
Interdisciplinary collaboration is central to enhancing enhanced patient outcomes as well as the quality of patient care. This collaboration is essential to solving problems and complex issues encountered in healthcare. Further, interprofessional collaboration offers an effective channel for communicating and executing change in healthcare practice. Effective collaboration must be coupled with effective leadership as well as collaborative strategies. Leadership strategies include effective communication, teamwork, and change and innovation. On the other hand, collaborative strategies go hand in hand with leadership strategies and include shared decision-making, delegation, and encouraging feedback.
Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Reflection Video Example 1 References
Beckett, C. D., Zadvinskis, I. M., Dean, J., Iseler, J., Powell, J. M., & Buck-Maxwell, B. (2021). An integrative review of team nursing and delegation: Implications for nurse staffing during COVID-19. Worldviews on Evidence-Based Nursing, 18(4), 251–260. https://doi.org/10.1111/wvn.12523
Elwyn, G. (2021). Shared decision making: What is the work? Patient Education and Counseling, 104(7), 1591–1595. https://doi.org/10.1016/j.pec.2020.11.032
Hlongwa, P., & Rispel, L. C. (2021). Interprofessional collaboration among health professionals in cleft lip and palate treatment and care in the public health sector of South Africa. Human Resources for Health, 19(1). https://doi.org/10.1186/s12960-021-00566-3
Schimith, M. D., Cezar-Vaz, M. R., Xavier, D. M., & Cardoso, L. S. (2021). Communication in health and inter-professional collaboration in the care for children with chronic conditions. Revista Latino-Americana de Enfermagem, 29, e3390. https://doi.org/10.1590/1518-8345.4044.3390
Skyberg, H. L., & Innvaer, S. (2020). Dynamics of interprofessional teamwork: Why three logics are better than one. Social Science & Medicine (1982), 265(113472), 113472. https://doi.org/10.1016/j.socscimed.2020.113472
Wagner, E. A. (2018). Improving patient care outcomes through better delegation-communication between nurses and assistive personnel. Journal of Nursing Care Quality, 33(2), 187–193. https://doi.org/10.1097/NCQ.0000000000000282
Wieke Noviyanti, L., Ahsan, A., & Sudartya, T. S. (2021). Exploring the relationship between nurses’ communication satisfaction and patient safety culture. Journal of Public Health Research, 10(2). https://doi.org/10.4081/jphr.2021.2225
Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Reflection Video Instructions
For this assessment you will create a 5-10 minute video reflection on an experience in which you collaborated interprofessionally, as well as a brief discussion of an interprofessional collaboration scenario and how it could have been better approached.
Interprofessional collaboration is a critical aspect of a nurse’s work. Through interprofessional collaboration, practitioners and patients share information and consider each other’s perspectives to better understand and address the many factors that contribute to health and well-being (Sullivan et al., 2015). Essentially, by collaborating, health care practitioners and patients can have better health outcomes. Nurses, who are often at the frontlines of interacting with various groups and records, are full partners in this approach to health care.
Reflection is a key part of building interprofessional competence, as it allows you to look critically at experiences and actions through specific lenses. From the standpoint of interprofessional collaboration, reflection can help you consider potential reasons for and causes of people’s actions and behaviors (Saunders et al., 2016). It also can provide opportunities to examine the roles team members adopted in a given situation as well as how the team could have worked more effectively.
As you begin to prepare this assessment you are encouraged to complete the What is Reflective Practice? activity. The activity consists of five questions that will allow you the opportunity to practice self-reflection. The information gained from completing this formative will help with your success on the Collaboration and Leadership Reflection Video assessment. Completing formatives is also a way to demonstrate course engagement
Note: The Example Kaltura Reflection demonstrates how to cite sources appropriately in an oral presentation/video. The Example Kaltura Reflection video is not a reflection on the Vila Health activity. Your reflection assessment will focus on both your professional experience and the Vila Health activity as described in the scenario.
Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Reflection Video References
Saunders, R., Singer, R., Dugmore, H., Seaman, K., & Lake, F. (2016). Nursing students’ reflections on an interprofessional placement in ambulatory care. Reflective Practice, 17(4), 393–402.
Sullivan, M., Kiovsky, R., Mason, D., Hill, C., Duke, C. (2015). Interprofessional collaboration and education. American Journal of Nursing, 115(3), 47–54.
Demonstration of Proficiency in Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Reflection Video
- Competency 1: Explain strategies for managing human and financial resources to promote organizational health.
- Identify how poor collaboration can result in inefficient management of human and financial resources supported by evidence from the literature.
- Competency 2: Explain how interdisciplinary collaboration can be used to achieve desired patient and systems outcomes.
- Reflect on an interdisciplinary collaboration experience noting ways in which it was successful and unsuccessful in achieving desired outcomes.
- Identify best-practice interdisciplinary collaboration strategies to help a team to achieve its goals and work more effectively together.
- Competency 4: Explain how change management theories and leadership strategies can enable interdisciplinary teams to achieve specific organizational goals.
- Identify best-practice leadership strategies from the literature, which would improve an interdisciplinary team’s ability to achieve its goals.
- Competency 5: Apply professional, scholarly, evidence-based communication strategies to impact patient, interdisciplinary team, and systems outcomes.
- Communicate via video with clear sound and light.
- The full reference list is from relevant and evidence-based (published within 5 years) sources, exhibiting nearly flawless adherence to APA format.
Professional Context for Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Reflection Video
This assessment will help you to become a reflective practitioner. By considering your own successes and shortcomings in interprofessional collaboration, you will increase awareness of your problem-solving abilities. You will create a video of your reflections, including a discussion of best practices of interprofessional collaboration and leadership strategies, cited in the literature.
Scenario
As part of an initiative to build effective collaboration at your Vila Health site, where you are a nurse, you have been asked to reflect on a project or experience in which you collaborated interprofessionally and examine what happened during the collaboration, identifying positive aspects and areas for improvement.
You have also been asked to review a series of events that took place at another Vila Health location and research interprofessional collaboration best practices and use the lessons learned from your experiences to make recommendations for improving interprofessional collaboration among their team.
Your task is to create a 5–10 minute video reflection with suggestions for the Vila Health team that can be shared with leadership as well as Vila Health colleagues at your site. Note: If you require the use of assistive technology or alternative communication methods to participate in this activity, please contact DisabilityServices@Capella.edu to request accommodations. If, for some reason, you are unable to record a video, please contact your faculty member as soon as possible to explore options for completing the assessment.
Capella NURS-FPX 4010 Assessment 1 Reflection Video Instructions
Using Kaltura, record a 5–10 minute video reflection on an interprofessional collaboration experience from your personal practice, proposing suggestions on how to improve the collaboration presented in the Vila Health: Collaboration for Change activity.
Be sure that your assessment addresses the following criteria. Please study the scoring guide carefully so you will know what is needed for a distinguished score:
- Reflect on an interdisciplinary collaboration experience, noting ways in which it was successful and unsuccessful in achieving desired outcomes.
- Identify how poor collaboration can result in inefficient management of human and financial resources, citing supporting evidence from the literature.
- Identify best-practice leadership strategies from the literature that would improve an interdisciplinary team’s ability to achieve its goals, citing at least one author from the literature.
- Identify best-practice interdisciplinary collaboration strategies to help a team achieve its goals and work together, citing the work of at least one author.
- Communicate in a professional manner, is easily audible, and uses proper grammar. Format reference list in current APA style.
You will need to relate an experience that you have had collaborating on a project. This could be at your current or former place of practice, or another relevant project that will enable you to address the requirements. In addition to describing your experience, you should explain aspects of the collaboration that helped the team make progress toward relevant goals or outcomes, as well as aspects of the collaboration that could have been improved.
A simplified gap-analysis approach may be useful:
- What happened?
- What went well?
- What did not go well?
- What should have happened?
After your personal reflection, examine the scenario in the Vila Health activity and discuss the ways in which the interdisciplinary team did not collaborate effectively and the negative implications for the human and financial resources of the interdisciplinary team and the organization as a whole.
Building on this investigation, identify at least one leadership best practice or strategy that you believe would improve the team’s ability to achieve their goals. Be sure to identify the strategy and its source or author and provide a brief rationale for your choice of strategy.
Additionally, identify at least one interdisciplinary collaboration best practice or strategy to help the team achieve its goals and work more effectively together. Again, identify the strategy, its source, and reasons why you think it will be effective.
You are encouraged to integrate lessons learned from your self-reflection to support and enrich your discussion of the Vila Health activity.
You are required to submit an APA-formatted reference list for any sources that you cited specifically in your video or used to inform your presentation. The Example Kaltura Reflection will show you how to cite scholarly sources in the context of an oral presentation.
Refer to the Campus tutorial Using Kaltura [PDF] as needed to record and upload your reflection.
Additional Requirements when Completing Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Reflection Video
- References: Cite at least 3 professional or scholarly sources of evidence to support the assertions you make in your video. Include additional properly cited references as necessary to support your statements.
- APA Reference Page: Submit a correctly formatted APA reference page that shows all the sources you used to create and deliver your video.
- You may wish to refer to the Campus APA Module for more information on applying APA style.
See Also:
NURS-FPX4010 Assessment 2 Interview and Interdisciplinary Issue Identification
Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Reflection Video Example Paper 2
Hello everyone, welcome to my collaboration and leadership reflection for Assessment 1. My name is (Insert name).
In this presentation, I intend to:
- Reflect on an interdisciplinary collaboration experience while summarizing a Vila Health Activity, including what was successful and what faltered in achieving the desired outcomes.
- Elaborate on how poor collaboration can result in inefficient management of human and financial resources.
- Explain the best leadership strategies to improve an interdisciplinary team’s ability to achieve collective goals while integrating insights from the literature.
Reflection of an Interdisciplinary Collaboration Experience
Change is inevitable in the healthcare sector, considering the need to provide quality care and address the increasing demand for healthcare services. One of the most profound strategies to enhance healthcare services is integrating technological advances by revamping the existing healthcare systems. After analyzing the importance of new technologies, our organization (Clarion Court Skilled Nursing Facility) embarked on a multidisciplinary commitment to implementing Healthix, a new electronic health record (EHR).
Since we relied on relatively outdated health record systems, the organizational management selected a team to collaborate with designers and information technology (IT) experts from Healthix for localized installations Capella NURS-FPX 4010 Assessment 1 Assignment Collaboration and Leadership Reflection Video. The team comprised local computer experts, advanced practice registered nurses (APRNs), the director of operations, and administrators.
The team from Healthix headquarters was supposed to interact with the local team to oversee the effective installation and replacement of the existing health record systems. However, that was not the case because IT experts from Healthix opted to ignore our team by downplaying our suggestions regarding the new EHR. Undoubtedly, this factor affected interdisciplinary collaboration, rendering the project ineffective and inefficient.
What went well?
Our team at Clarion Court Skilled Nursing Facility spearheaded an internal preparedness plan for implementing Healthix by embracing new approaches, including convincing the organization to avail resources for the new system. Also, we consolidated opinions from patients and other stakeholders regarding the importance of revamping and replacing old systems with Healthix. As a result, we were adequately prepared to embrace advanced technologies for promoting quality care and enhancing process efficiency.
What did not go well?
Ineffective collaboration between the team from Healthix headquarters and our implementation team hampered the overall process of incorporating a new electronic health record (EHR) system. The external team had a responsibility to design Healthix based on organizational needs and inputs for local professionals. However, IT experts opted to implement it based on their experience and expertise without considering insights from corporate stakeholders. Consequently, this consideration led to dissatisfaction from the local team, project ineffectiveness, and additional risks to patient safety.
How poor collaboration can result in inefficient management of human and financial resources.

Poor collaboration can lead to the inefficient management of human and financial resources due to ineffective communication patterns and conflicting ideologies.
Busari et al. (2017) describe collaboration in healthcare as “the capacity of every healthcare professional to effectively embrace complementary roles within a team, work cooperatively, share responsibilities for problem-solving, and make the decisions needed to formulate and carry out patient care” (p. 228).
In this sense, interprofessional and interdisciplinary collaboration between nurses, physicians, and other stakeholders enhances collective awareness and promotes knowledge and skills.
Amidst the need to deliver quality care in scenarios of financial and human resource constraints, team performance and collaboration enable healthcare professionals to pool skills and competencies together to enhance process effectiveness. In the Vila Health experience case study, it is clear that ineffective collaboration between the Healthix team and local stakeholders affected the overall utilization of financial and human resources to realize the collective objective of implementing the Healthix record system.
The best leadership strategies for enabling interdisciplinary teams to achieve collective goals
Appropriate leadership and change management strategies are crucial in enhancing the team’s effectiveness and ability to realize goals. Xu (2017) proposes transformational and participative leadership as appropriate styles to guarantee proper change management. The author suggests that the transformational leadership style enables nursing leaders to create an ideal impact, motivate followers, integrate intellectual stimulation, and incorporate personal considerations in decisions. On the other hand, participative leadership allows followers to connect and participate in the change management process by being more committed to goals.
Transformational and participative leadership styles complement other strategies for ensuring team effectiveness. Buljac-Samardzic et al. (2020) contend that a lack of team performance is a primary point of susceptibility to quality and safety of care. Further, the authors argue that organizational interventions, including simulation training, effective resource management, and interprofessional collaboration, are practical strategies for enhancing team effectiveness.
In the Vila Health experience, proper change management and leadership strategies were inadequate because they failed to uphold the tenets of interprofessional collaboration. This aspect jeopardized the adoption of Healthix electric health records systems.
In conclusion, interprofessional collaboration is an essential aspect of organizational change in the healthcare sector since it enables stakeholders to consolidate efforts, manage resources, and focus on achieving collective outcomes. The Vila Health experience shows that a lack of stakeholder engagement and participation presents a primary weakness when embracing new ways. Also, change management and leadership strategies determine the trajectories of institutional change by determining the levels of resource management and structural alignment to new ways.
Capella NURS-FPX 4010 Assessment 1 Reflection Video References
Buljac-Samardzic, M., Doekhie, K., & van Wijngaarden, J. (2020). Interventions to improve team effectiveness within health care: a systematic review of the past decade. Human Resources for Health, 18(1). https://doi.org/10.1186/s12960-019-0411-3
Busari, J., Moll, F., & Duits, A. (2017). Understanding the impact of interprofessional collaboration on the quality of care: a case report from a small-scale resource-limited health care environment. Journal Of Multidisciplinary Healthcare, 10, 227-234. https://doi.org/10.2147/jmdh.s140042
Xu, J. (2017). Leadership theory in clinical practice. Chinese Nursing Research, 4(4), 155-157. https://doi.org/10.1016/j.cnre.2017.10.001
NURS-FPX4010 Assessment 2 Interview and Interdisciplinary Issue Identification
For this assessment, you will create a 2-4 page report on an interview you have conducted with a health care professional. You will identify an issue from the interview that could be improved with an interdisciplinary approach, and review best practices and evidence to address the issue.
As a baccalaureate-prepared nurse, your participation and leadership in interdisciplinary teams will be vital to the health outcomes for your patients and organization. One way to approach designing an improvement project is to use the Plan-Do-Study-Act (PDSA) cycle. The Institute for Healthcare Improvement describes it thus:
The Plan-Do-Study-Act (PDSA) cycle is shorthand for testing a change in the real work setting—by planning it, trying it, observing the results, and acting on what is learned. This is the scientific method adapted for action-oriented learning…Essentially, the PDSA cycle helps you test out change ideas on a smaller scale before evaluating the results and making adjustments before potentially launching into a somewhat larger scale project (n.d.).
You might also recognize that the PDSA cycle resembles the nursing process. The benefit of gaining experience with this model of project design is that it provides nurses with an opportunity to ideate and lead improvements.
For this assessment, you will not be implementing all of the PDSA cycle. Instead, you are being asked to interview a health care professional of your choice to determine what kind of interdisciplinary problem he or she is experiencing or has experienced in the workplace. This interview, in Assessment 2, will inform the research that you will conduct to propose a plan for interdisciplinary collaboration in Assessment 3.
It would be an excellent choice to complete the PDSA Cycle activity prior to developing the re
READ MORE >>
check out the resources listed on the Writing Center’s Writing Support page. ...
Instructions
Complete this assessment in two parts.
Part 1
Assess the effect of the patient
READ MORE >>
Capella NURS-FPX4900 AssessmentsAssessing the Problem, Leadership, Collaboration ...
Capella NURS-FPX4900 Assessments
Assessing the Problem, Leadership, Collaboration, Communication, Change Management, and Policy Considerations Example Approach
Nurses, who make up the majority of the healthcare workforce, are vital to patient care. Nurses in all professional roles strive to improve organizational processes and achieve positive patient outcomes. In particular, nurses identify problems, plan interventions/strategies, and implement the strategies-skills, all of which directly impact patient outcomes and organizational effectiveness (Wakefield et al., 2021).
Patient care is constantly evolving, and this evolution is due to the initial identification of a problem and the pursuit of solutions. However, before embarking on a specific change management strategy, the best approach is to assess and review credible evidence to determine appropriate interventions. As a result, nurses must be actively involved in the entire change process, beginning with the prodromal phase of justifying the appropriateness of interventions to be implemented (Wakefield et al., 2021).
Using hypertension as an example, the goal of the following discussion is to elaborate on the problem extensively, drawing on evidence from relevant databases, and to discuss the effectiveness of nursing standards/or policies in improving the patient problem, as well as the leadership strategies relevant to the problem identified.
Identification of the Patient/Family/Population Health Problem Relevant to My Practice
Summary of the Health Problem
Chronic illness management places a significant burden on patients and the healthcare system as a whole. A significant proportion of the global population is affected by hypertension, chronic disease, and the leading preventable risk factor for cardiovascular disease (CVD). Hypertension is defined as high blood pressure, with a systolic blood pressure of ?140 mm Hg and a diastolic blood pressure of ?90 mm Hg (AHA, 2022).
Also, Mills et al. (2020) define hypertension as the current use of antihypertensive medications for research purposes. In 2010, the condition affected 1.38 billion people, or 31.1% of the global population, with men having a slightly higher prevalence of 31.9% than females, who had a prevalence of 30.1% (Mills et al., 2020). Modifiable risk factors for hypertension include obesity, alcohol, smoking, diet, and physical inactivity.
In contrast, the non-modifiable risk factors include a family history of hypertension, age over 65, and comorbidities such as chronic kidney disease [CKD] (WHO, 2021). Since hypertension is mostly asymptomatic, most people are unaware they have it, earning it the moniker “silent killer.”
If symptoms exist, they are often nonspecific and may include headaches, fatigue, nosebleeds, irregular heartbeats, vision changes, and ear buzzing (WHO, 2022). Because of the serious damage that hypertension causes to essential body organs such as the kidney, heart, eyes, brain, and so on, it is recommended that the problem be identified and treated as soon as possible to avoid rapid progression to unwanted sequela.
Patient/Family/Group that I intend to work with
I plan to work with adult hypertensive patients during my practicum. Patients with a systolic blood pressure of 140 mm Hg and a diastolic blood pressure of 90 mm Hg, or those who are currently taking hypertensive medications, fall into this category. According to WHO (2021), an estimated 1.28 billion adults aged 30-79 worldwide have hypertension, with two-thirds of them living in low-to-middle-income countries.
Approximately 46% of adults with hypertension are unaware of their condition, and approximately 42% are diagnosed and treated (WHO, 2021). Furthermore, it is estimated that only one in every five adults (21%) has hypertension under control. As a result, while efforts to control hypertension have long existed, more efforts are still required to meet the global target of a 33% reduction in hypertension prevalence between 2010 and 2030 (WHO, 2021). Adult hypertensive patients would be a potentially valuable population for my practicum.
Significance and Relevance of the Problem
Hypertension contributes significantly to the global burden of CVD and premature death. In 2015, there were approximately 10.7 million all-cause deaths associated with a systolic blood pressure of ?110-115 mm Hg (19.2% of all deaths) and 7.8 million (14% of all deaths) all-cause deaths associated with a systolic blood pressure of ?140 mm Hg (Mills et al., 2020). Various CVDs were responsible for these deaths, including ischemic heart disease (IHD), ischemic stroke, and hemorrhagic stroke.
In addition to CVD events, several studies have shown that hypertension is a significant independent risk factor for chronic kidney disease (CKD) and end-stage renal disease (ESRD). In one study, 332544 men aged 35-57 years who were screened for entry into the MRFIT trial and did not have ESRD at baseline were followed for 16 years, and when compared to normotensive men with a systolic blood pressure of <120 mm Hg and diastolic blood pressure of <80 mm Hg, the findings revealed that the relative risk of ESRD for men with hypertension who had a systolic BP >210 mmHg or diastolic BP >120 mmHg was 22.1 [P < 0.001] (Mills et al., 2020).
Additionally, individuals with hypertension in the United States (US) are estimated to have nearly $ 2,000 higher annual healthcare expenditures than their non-hypertensive peers, and hypertension is associated with approximately $131 billion in healthcare costs (Kirkland et al., 2018). With the obvious burden of hypertension, it is only necessary to work on strategies to lessen the disease’s impact.
Why is the Problem Relevant to My Practice as a Baccalaureate-Prepared Nurse
Nurses are frequently the first point of contact for patients. As a Baccalaureate-prepared nurse, I am trained to provide quality patient care, including initial review at the emergency unit, blood pressure measurements, diagnosis, treatment advice, or referral to a physician or other specialists. The interventions we provide to this group of patients must be aimed at lowering blood pressure and preventing the progression to unfavorable sequelae.
According to Rahimi et al. (2021), every 10 mm Hg reduction in systolic BP significantly reduces the risk of major CVD events by 20% (relative risk 0.80, 95% CI 0.77–0.83), IHD by 17% (relative risk 0.83, 0.78–0.88), stroke by 27% (relative risk 0.73, 0.68–0.77), heart failure by 28% (relative risk 0.72, 0.67–0.78) and all-cause mortality by 13% (0.87, 0.84–0.91). This indicates that even nurses’ efforts to assist hypertensive patients in managing their blood pressure count, and thus, the relevance of my practice to the population group chosen.
Evidence from Peer-Reviewed Literature
Barriers to the Implementation of Evidence-Based Practice in addressing the Problem
As the adult population with hypertension grows, it becomes more difficult for healthcare professionals to assist their patients with blood pressure control. According to the American Medical Association (AMA), there are five barriers to implementing evidence-based practice in hypertensive patients’ care. First, inaccurate and inconsistent blood pressure measurement techniques may impede hypertension diagnosis and management (AMA, 2018).
It is recommended that at least two blood pressure measurements be taken, with the cuff bladder encircling at least 80% of the arm (CDC, 2022), failure of which may result in incorrect readings and the inability to diagnose hypertension. Second, masked hypertension, which causes patients to appear to have normal blood pressures in the office while having elevated blood pressures outside the office, may contribute to hypertension underdiagnosis.
Third, clinical inertia, blamed on the care team, who may be hesitant to initiate and intensify hypertension treatment, may delay treatment and hasten disease progression (AMA, 2018). Fourth, the care team may lack appropriate evidence-based treatment protocols. Finally, poor patient participation in self-management behaviors may jeopardize blood pressure control.
Effectiveness of Nursing Standards/or Policies in Improving the Population Outcomes for the Problem
Nurses play an integral role in the care of hypertensive patients in various ways. Nurses identify, refer, and follow up on hypertensive patients. They use the best blood pressure measurement methods and also lead blood pressure screening and verification initiatives in community settings. Furthermore, they determine whether the readings are normal or in the hypertensive range according to the site protocol and then refer for urgent care (Georgiopoulos et al., 2018).
Nurses also assist in the diagnosis and management of hypertensive patients’ medications. According to Georgiopoulos et al. (2018), nurse-led hypertension management results in higher rates of blood pressure control than standard care. In addition, nurses provide patient education, counseling, and skill development, allowing patients to develop better self-management strategies that aid in blood pressure control.
Furthermore, nurses ensure care coordination—they are skilled at establishing and maintaining both formal and informal collaborative links between providers, resources, and services within and outside their practice settings (Georgiopoulos et al., 2018). Moreover, performance measurement and quality improvement indicators, a task of nurses, allow for the determination of whether or not the interventions provided to patients are effective. Leveraging the tasks nurses perform, effective blood pressure control is achieved, with a reduction in complications and mortality rates.
Role of Nurses in Policy Making to Improve Outcomes, prevent Illnesses and Reduce Hospital Readmissions.
Nurses spend significant time working directly with patients, so they are familiar with the specific needs of the people they serve. As a result, nurses can advocate for public policy changes that benefit the patients they care for. They develop policies where none exist, reform harmful or ineffective policies, and ensure those good policies are implemented and enforced (Turale & Kunaviktikul, 2019).
One of the most critical areas where nurses can influence policy is smoking cessation, where policies such as imposing heavy taxes on cigarettes or prohibiting smoking within specific areas may aid in smoking cessation. Because smoking is a risk factor for hypertension, smoking reduction or cessation is an evidence-based lifestyle modification to lower blood pressure (improve outcomes), prevent hypertension, or reduce readmission of already hypertensive patients.
Nursing Theory or Conceptual Framework that frames and guides Actions during my Practicum
Nursing theories provide the foundations for the knowledge and skills used in practice. Comfort is a valuable outcome of care during delivery; I would thus refer to Katharine Kolcaba’s theory of comfort. Kolcaba distinguished three types of comfort: relief, which involves relieving patients of, say, pain, ease, which addresses comfort in a state of contentment, and transcendence, which is a state of comfort in which patients can rise above their challenges. (Oliveira et al., 2020).
Understanding that comfort can take the form of physical, psychospiritual, environmental, or sociocultural contexts; I will ensure that all strategies and care interventions delivered aim to provide comfort to the population group identified.
How State Board Nursing Practice Standards and/or Organizational or Governmental Policies affect the Population Problem Defined
Each state has its own set of nursing standards that resident nurses must follow. The standards frequently dictate independent practice and prescriptive authority. In Alabama, for example, a certified registered nurse (RN) is responsible for providing continuous and comprehensive care for a wide range of conditions for which the certified RN is educationally prepared, taking patients’ health histories and performing physical examinations, formulating working diagnoses, prescribing (albeit with limited prescriptive authority), administering and providing therapeutic measures, tests, and drugs, counseling patients, consulting and referring to other professionals (Alabama Board of Nursing, 2022).
The scope of practice established by the State Board of Nursing allows nurses to be fully responsible for the patients they care for, in this case, adult hypertensive patients. Specific organizational rules also govern how nurses care for patients. For example, certain organizations, such as the one with which I work, limit nurses’ prescriptive authority and only allow them to do so under the supervision of a physician. This can have negative consequences because one must wait for a physician to prescribe medications, which can cause the patient’s treatment to be delayed.
Leadership Strategies to Improve Outcomes, Patient-Centered Care, and Patient Experience related to the Population Problem Identified
Leadership is a critical tool in healthcare. It serves as the organization’s engine, providing fuel and direction as it journeys toward its objectives. Leaders are thus essential to the operation of an organization, and the strategies employed to determine whether or not the organization’s objectives are met.
Transformational leadership would be used in the care of adult hypertensive patients. Collins et al. (2020) define transformational leadership as an approach that causes a change in individuals and social systems. The practicum’s goal is to develop interventions or change strategies to improve the management of the defined population health problem, so transformational leadership is the best strategy.
In terms of collaboration, strategies that would ensure the team works effectively include (1) being aware of and respecting each other’s duties, (2) effective communication, (3) viewing patients as partners, and (4) recognizing the efforts of others. Preparing the organization for change, crafting a vision and plan for change, implementing the changes, embedding the changes within the organizational culture and practices, and finally, reviewing progress and analyzing the results (Barrow et al., 2021) are the change management strategies that I anticipate will be required.
The first step, which involves preparing people and organizations for change, is critical because it determines whether the subsequent phases are smooth or bumpy. With this in mind, pre-change management preparations in terms of finances, human personnel, skills, and organizational attitude are critical.
Conclusion
Change is a constant in healthcare, and it has greatly aided in the improvement of healthcare services. Before change can occur, an initial phase of identifying the problem and establishing the resources required for the change is pertinent. In the case of adult hypertensive patients, baccalaureate-prepared nurses play a significant role in identifying patient care needs and implementing evidence-based interventions and strategies to meet those needs.
However, using evidence-based strategies in the care of hypertensive patients can be hampered by various factors, including a lack of appropriate evidence-based treatment protocols and clinical inertia. These challenges can be forestalled with the right leadership and collaborative strategies, enabling patients to receive high-quality, safe, and cost-effective care.
Capella NURS-FPX4900 Assessments References
Alabama Board of Nursing. (2022). Alabama State Board Nursing Practice Standards. Alabama.gov. https://www.abn.alabama.gov/
American Heart Association. (2022). High blood pressure. Www.heart.org. https://www.heart.org/en/health-topics/high-blood-pressure
American Medical Association. (2018, November 20). 5 barriers to hypertension control: What they are and how to address them. American Medical Association. https://www.ama-assn.org/delivering-care/hypertension/5-barriers-hypertension-control-what-they-are-and-how-address-them
Barrow, J. M., Annamaraju, P., & Toney-Butler, T. J. (2021). Change Management. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459380/
CDC. (2022, September 8). Measure your blood pressure. Centers for Disease Control and Prevention. https://www.cdc.gov/bloodpressure/measure.htm
Collins, E., Owen, P., Digan, J., & Dunn, F. (2020). Applying transformational leadership in nursing practice. Nursing Standard (Royal College of Nursing (Great Britain): 1987), 35(5), 59–66. https://doi.org/10.7748/ns.2019.e11408
Georgiopoulos, G., Kollia, Z., Katsi, V., Oikonomou, D., Tsioufis, C., & Tousoulis, D. (2018). Nurse’s contribution to alleviate non-adherence to hypertension treatment. Current Hypertension Reports, 20(8), 65. https://doi.org/10.1007/s11906-018-0862-2
Kirkland, E. B., Heincelman, M., Bishu, K. G., Schumann, S. O., Schreiner, A., Axon, R. N., Mauldin, P. D., & Moran, W. P. (2018). Trends in healthcare expenditures among US adults with hypertension: National estimates, 2003-2014. Journal of the American Heart Association, 7(11). https://doi.org/10.1161/JAHA.118.008731
Mills, K. T., Stefanescu, A., & He, J. (2020). The global epidemiology of hypertension. Nature Reviews. Nephrology, 16(4), 223–237. https://doi.org/10.1038/s41581-019-0244-2
Oliveira, S. M. de, Costa, K. N. de F. M., Santos, K. F. O. D., Oliveira, J. D. S., Pereira, M. A., & Fernandes, M. das G. M. (2020). Comfort needs as perceived by hospitalized elders: an analysis under the light of Kolcaba’s theory. Revista Brasileira de Enfermagem, 73(suppl 3), e20190501. https://doi.org/10.1590/0034-7167-2019-0501
Rahimi, K., Bidel, Z., Nazarzadeh, M., Copland, E., Canoy, D., Ramakrishnan, R., Pinho-Gomes, A.-C., Woodward, M., Adler, A., Agodoa, L., Algra, A., Asselbergs, F. W., Beckett, N. S., Berge, E., Black, H., Brouwers, F. P. J., Brown, M., Bulpitt, C. J., Byington, R. P., … Davis, B. R. (2021). Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet, 397(10285), 1625–1636. https://doi.org/10.1016/s0140-6736(21)00590-0
Turale, S., & Kunaviktikul, W. (2019). The contribution of nurses to health policy and advocacy requires leaders to provide training and mentorship: Nurses’ contribution to health policy and advocacy. International Nursing Review, 66(3), 302–304. https://doi.org/10.1111/inr.12550
Wakefield, M., Williams, D. R., Le Menestrel, S., & Flauber, J. L. (2021). The role of nurses in improving health equity. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK573898/
World Health Organization. (2021). Hypertension. Who.int. https://www.who.int/news-room/fact-sheets/detail/hypertension
Capella NURS-FPX4900 Assessment 1: Assessing the Problem: Leadership, Collaboration, Communication, Change Management, and Policy Considerations
- In a 5-7 page written assessment, define the patient, family, or population health problem that will be the focus of your capstone project. Assess the problem from a leadership, collaboration, communication, change management, and policy perspective.
- Plan to spend approximately 2 direct practicum hours meeting with a patient, family, or group of your choice to explore the problem and, if desired, consulting with subject matter and industry experts. Document the time spent (your practicum hours) with these individuals or group in the Capella Academic Portal Volunteer Experience Form.
Introduction
Nurses in all professional roles work to effect positive patient outcomes and improve organizational processes. Professional nurses are leaders in problem identification, planning, and strategy implementation—skills that directly affect patient care or organizational effectiveness.
Too often, change agents jump to a conclusion that an intervention will promote the envisioned improvement. Instead, the ideal approach is to determine which interventions are appropriate, based on an assessment and review of credible evidence. Interventions could be patient-facing or involve a change in policy and process. In this assessment, you’ll identify and make the case for your practicum focus area, then explore it in depth from a leadership, collaboration, communication, change management, and policy perspective.
This assessment lays the foundation for the work that will carry you through your capstone experience and guide the practicum hours needed to complete the work in this course. In addition, it will enable you to do the following:
- Develop a problem statement for a patient, family, or population that’s relevant to your practice.
- Begin building a body of evidence that will inform your approach to your practicum.
- Focus on the influence of leadership, collaboration, communication, change management, and policy on the problem.
Preparation
In this assessment, you’ll assess the patient, family, or population health problem that will be the focus of your capstone project. Plan to spend approximately 2 hours working with a patient, family, or group of your choice to explore the problem from a leadership, collaboration, communication, change management, and policy perspective. During this time, you may also choose to consult with subject matter and industry experts about the problem (for example, directors of quality or patient safety, nurse managers/directors, physicians, and epidemiologists).
To prepare for the assessment, complete the following:
- Identify the patient, family, or group you want to work with during your practicum The patient you select can be a friend or a family member. You’ll work with this patient, family, or group throughout your capstone project, focusing on a specific health care problem.
- Begin surveying the scholarly and professional literature to establish your evidence and research base, inform your assessment, and meet scholarly expectations for supporting evidence.
In addition, you may wish to complete the following:
- Review the assessment instructions and scoring guide to ensure that you understand the work you’ll be asked to complete and how it will be assessed.
- Review the Practicum Focus Sheet: Assessment 1 [PDF], which provides guidance for conducting this portion of your practicum.
Note: As you revise your writing, check out the resources listed on the Writing Center’s Writing Support page.
Capella NURS-FPX4900 Assessments Instructions
Complete this assessment in two parts.
Part 1
Define the patient, family, or population health problem that will be the focus of your capstone project. Assess the problem from a leadership, collaboration, communication, change management, and policy perspective and establish your evidence and research base to plan, implement, and share findings related to your project.
Part 2
Connect with the patient, family, or group you’ll work with during your practicum. During this portion of your practicum, plan to spend at least 2 hours meeting with the patient, family, or group and, if desired, consulting with subject matter and industry experts of your choice. The hours you spend meeting with them should take place outside of regular work hours. Use the Practicum Focus Sheet [PDF] provided for this assessment to guide your work and interpersonal interactions. Document the time spent (your practicum hours) with these individuals or group in the Capella Academic Portal Volunteer Experience Form.
Capella Academic Portal
Complete the NURS-FPX4900 Volunteer Experience Form in Capella Academic Portal. Include a description of your relationship to the patient, family, or group in the Volunteer Experience comments field.
The BSN Capstone Course (NURS-FPX4900 ) requires the completion and documentation of nine (9) practicum hours. All hours must be recorded in the Capella Academic Portal. Please review the BSN Practicum Campus page for more information and instructions on how to log your hours.
Requirements
The assessment requirements, outlined below, correspond to the scoring guide criteria, so be sure to address each main point. Read the performance-level descriptions for each criterion to see how your work will be assessed. In addition, note the additional requirements for document format and length and for supporting evidence.
- Define a patient, family, or population health problem that’s relevant to your practice.
- Summarize the problem you’ll explore.
- Identify the patient, family, or group you intend to work with during your practicum.
- Provide context, data, or information that substantiates the presence of the problem and its significance and relevance to the patient, family, or population.
- Explain why this problem is relevant to your practice as a baccalaureate-prepared nurse.
- Analyze evidence from peer-reviewed literature and professional sources that describes and guides nursing actions related to the patient, family, or population problem you’ve defined.
- Note whether the authors provide supporting evidence from the literature that’s consistent with what you see in your nursing practice.
- Explain how you would know if the data are unreliable.
- Describe what the literature says about barriers to the implementation of evidence-based practice in addressing the problem you’ve defined.
- Describe research that has tested the effectiveness of nursing standards and/or policies in improving patient, family, or population outcomes for this problem.
- Describe current literature on the role of nurses in policy making to improve outcomes, prevent illness, and reduce hospital readmissions.
- Describe what the literature says about a nursing theory or conceptual framework that might frame and guide your actions during your practicum.
- Explain how state board nursing practice standards and/or organizational or governmental policies could affect the patient, family, or population problem you’ve defined.
- Describe research that has tested the effectiveness of these standards and/or policies in improving patient, family, or population outcomes for this problem.
- Describe current literature on the role of nurses in policy making to improve outcomes, prevent illness, and reduce hospital readmissions.
- Describe the effects of local, state, and federal policies or legislation on your nursing scope of practice, within the context of this problem.
- Propose leadership strategies to improve outcomes, patient-centered care, and the patient experience related to the patient, family, or population problem you’ve defined.
- Discuss research on the effectiveness of leadership strategies.
- Define the role that you anticipate leadership must play in addressing the problem.
- Describe collaboration and communication strategies that you anticipate will be needed to address the problem.
- Describe the change management strategies that you anticipate will be required to address the problem.
- Document the time spent (your practicum hours) with these individuals or group in the Capella Academic Portal Volunteer Experience Form.
- Organize content so ideas flow logically with smooth transitions.
- Apply APA style and formatting to scholarly writing.
Capella NURS-FPX4900 Assessments Additional Requirements
- Format: Format your paper using APA style. APA Style Paper Tutorial [DOCX] is provided to help you in writing and formatting your paper. Be sure to include:
- A title page and reference page. An abstract is not required.
- Appropriate section headings.
- Length: Your paper should be approximately 5–7 pages in length, not including the reference page.
- Supporting evidence: Cite at least five sources of scholarly or professional evidence that support your central ideas. Resources should be no more than five years old. Provide in-text citations and references in APA format.
- Proofreading: Proofread your paper, before you submit it, to minimize errors that could distract readers and make it more difficult for them to focus on its substance.
Competencies Measured
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
- Competency 1: Lead people and processes to improve patient, systems, and population outcomes.
- Define a patient, family, or population health problem that’s relevant to personal and professional practice.
- Competency 2: Make clinical and operational decisions based upon the best available evidence.
- Analyze evidence from peer-reviewed literature and professional sources that describes and guides nursing actions related to a defined patient, family, or population problem.
- Competency 5: Analyze the impact of health policy on quality and cost of care.
- Explain how state board nursing practice standards and/or organizational or governmental policies could affect a defined patient, family, or population problem.
- Competency 7: Implement patient-centered care to improve quality of care and the patient experience.
- Propose leadership strategies to improve outcomes, patient-centered care, and the patient experience related to a defined patient, family, or population problem and document the practicum hours spent with these individuals or group in the Capella Academic Portal Volunteer Experience Form.
- Competency 8: Integrate professional standards and values into practice.
- Organize content so ideas flow logically with smooth transitions.
- Apply APA style and formatting to scholarly writing.
NURS-FPX4900 Assessment 2: Assessing the Problem: Quality, Safety, and Cost Considerations
- In a 5-7 page written assessment, assess the effect of the patient, family, or population problem you’ve previously defined on the quality of care, patient safety, and costs to the system and individual.
- Plan to spend approximately 2 direct practicum hours exploring these aspects of the problem with the patient, family, or group you’ve chosen to work with and, if desired, consulting with subject matter and industry experts. Document the time spent (your practicum hours) with these individuals or group in the Capella Academic Portal Volunteer Experience Form. Report on your experiences during your first two practicum hours.
Introduction
Organizational data, such as readmission rates, hospital-acquired infections, falls, medication errors, staff satisfaction, serious safety events, and patient experience can be used to prioritize time, resources, and finances. Health care organizations and government agencies use benchmark data to compare the quality of organizational services and report the status of patient safety. Professional nurses are key to comprehensive data collection, reporting, and monitoring of metrics to improve quality and patient safety.
Preparation
In this assessment, you’ll assess the effect of the health problem you’ve defined on the quality of care, patient safety, and
READ MORE >>
199–200.This article discusses the needs for quality and safety education in ...
- This article discusses the needs for quality and safety education in nursing and how the Journal of Continuing Education in Nursing supports QSEN competency implementation in practice.
Johnson
READ MORE >>
Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety Example 1Enhancin ...
Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety Example 1
Enhancing Quality and Safety
Safety in healthcare is essential in ensuring quality services. Safety in healthcare services is a measure of quality in that safety issues in healthcare translate to poor quality services and vice versa. Various patient safety risks and concerns exist in healthcare settings, leading to poor outcomes, loss of trust in the healthcare system, increased costs, and increased hospital length of stay. Quality healthcare also entails patient-centered care, utilization of evidence-based practice, clinical guidelines, and implementation of patient safety initiatives.
This paper examines Healthcare Associated Infections (HAI), a safety quality issue affecting my healthcare setting, and provides evidence-based solutions to address the issue. Additionally, the paper will explore the factors leading to patient safety risks in the healthcare setting, the evidence-based and best-practice solutions to improve patient safety and reduce costs, explain how nurses can help coordinate care to increase patient safety and reduce costs, and finally, identifies stakeholders with whom nurses would coordinate to drive safety enhancements with the safety quality issue.
Factors Leading to HAI in a healthcare Setting
Hospital-associated infections are infections that patients acquire while receiving healthcare services in a healthcare setting, including inpatient and outpatient settings. Various factors lead to HAIs in a healthcare setting. A major factor contributing to HAIs is poor maintenance and use of medical devices. Medical devices such as catheters and ventilators cause infections when not used and maintained appropriately. The other factor is the failure to maintain adequate infection control practices. According to Ripa et al. (2021), failure to adhere to recommended infection control measures significantly contributes to hospital-acquired infections.
Furthermore, patient factors may lead to HIAs in a healthcare setting. Ripa et al. (2021) note that some patients have a high risk of contracting HAIs. These include patients with compromised immune systems, underlying conditions prone to infections, and prolonged hospital stays. Understaffing and high workloads are other issues leading to HIAs. In understaffed settings, care providers have high patient-to-staff ratios, which increases the workload, potentially leading to lapses in infection control practices.
Evidence-based and Best-Practice Solutions to Improve Patient Safety and Reduce Costs
The World Health Organization (2021) developed a patient safety action plan to eliminate harm in healthcare settings, emphasizing the essence of infection prevention and control practices. Every healthcare setting should adhere to strict infection prevention and control measures and develop policies customized to the institution’s needs. Infection control measures include appropriate use of personal protective equipment for the care providers, disinfection of surfaces, environmental cleaning, and adherence to isolation precautions.
The other best-practice solution to improve patient safety and reduce costs is surveillance and monitoring patient safety issues. According to Duarte et al. (2020), healthcare institutions can reduce patient safety issues by creating robust surveillance systems to monitor patient safety issues, including tracking antimicrobial resistance patterns and identifying outbreaks, which allows for early detection and prompt response to prevent further infection transmission. Additionally, educating care providers on infection control practices, guidelines, and protocols is vital in improving patient safety and reducing costs.
Care Coordination to Improve Patient Safety and Reduce Costs
Nurses significantly help in coordinating care to improve patient safety and reduce costs. As among the care team leaders, nurses can mobilize other healthcare providers in initiatives aimed at improving patient safety and reducing care costs (Vaismoradi et al., 2020). For example, nurses can lead in infection prevention and control staff education and programs, ensuring all care providers are aware of the practices, policies, and protocols, thus improving patient safety and reducing costs.
Nurses also coordinate care by ensuring seamless communication among the care team, preventing gaps in care that would lead to patient safety issues such as medication errors, thus promoting patient safety. For instance, nurses can communicate with other care team members on the infection prevention and control protocols currently used to enhance patient safety and reduce costs related to HAIs.
Stakeholder Identification to Drive Safety Enhancements with HAIs
There are various stakeholders with whom nurses would need to coordinate in driving safety enhancements to prevent HAIs. Institution leaders and administrators are among the relevant stakeholders whom nurses need to involve in driving quality initiatives to enhance safety. The leaders allocate resources for the various initiatives and programs in institutions. Therefore, coordinating them in driving safety enhancements is crucial. Additionally, getting their buy-in and support for the initiative is vital, thus promoting success.
Other stakeholders include the clinical support staff, patients, and families, as well as other members of the interdisciplinary team. Simsekler et al. (2020) note that clinical support staff, such as lab technicians, play a major role in minimizing and preventing HAIs. Therefore, they are relevant stakeholders in safety enhancements.
Patients and their families should also be involved in enhancing safety since they also participate in self-management and home care. These stakeholders can also help provide feedback on safety issues, thus improving the initiatives. The interdisciplinary team is also vital in safety enhancements since it takes part in patient care planning, treatment, and care continuity (Simsekler et al., 2020).
Conclusion
Hospital Associated Infections are a major patient safety risk in healthcare institutions. Patient safety issues such as HAIs compromise care quality and increase the costs to the individual patient and the system. However, as discussed above, a wide array of evidence-based and best-practice solutions exist to address the issues. Nurses can also coordinate care to improve patient safety and reduce costs. Identifying relevant stakeholders in safety enhancement initiatives is crucial to improve their success.
Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety References
Duarte, S. D. C. M., Azevedo, S. S., Muinck, G. D. C., Costa, T. F. D., Cardoso, M. M. V. N., & Moraes, J. R. M. M. (2020). Best Safety Practices in Nursing Care in Neonatal Intensive Therapy. Brazilian Journal of Nursing 73(2), e20180482. https://doi.org/10.1590/0034-7167-2018-0482
Ripa, M., Galli, L., Poli, A., Oltolini, C., Spagnuolo, V., Mastrangelo, A., Muccini, C., Monti, G., De Luca, G., Landoni, G., Dagna, L., Clementi, M., Rovere Querini, P., Ciceri, F., Tresoldi, M., Lazzarin, A., Zangrillo, A., Scarpellini, P., Castagna, A., & COVID-BioB study group (2021). Secondary infections in patients hospitalized with COVID-19: incidence and predictive factors. Clinical Microbiology and Infection: The Official Publication of the European Society of Clinical Microbiology and Infectious Diseases, 27(3), 451–457. https://doi.org/10.1016/j.cmi.2020.10.021
Simsekler, M. C. E., Qazi, A., Alalami, M. A., Ellahham, S., & Ozonoff, A. (2020). Evaluation of patient safety culture using a random forest algorithm. Reliability Engineering & System Safety, 204, 107186. https://doi.org/10.1016/j.ress.2020.107186
Vaismoradi, M., Tella, S., A Logan, P., Khakurel, J., & Vizcaya-Moreno, F. (2020). Nurses’ Adherence to Patient Safety Principles: A Systematic Review. International Journal of Environmental Research and Public Health, 17(6), 2028. https://doi.org/10.3390/ijerph17062028
World Health Organization. (2021). Global patient safety action plan 2021-2030: towards eliminating avoidable harm in health care. World Health Organization. https://www.who.int/teams/integrated-health-services/patient-safety/policy/global-patient-safety-action-plan
Also Read:
NURSFPX4020 Capella Assessment 3 Improvement Plan In-Service Presentation.
Capella University NURS-FPX4020 Assessment 4 Quality Improvement Initiative Tool Kit Essay
Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety Instructions
- For this assessment, you will develop a 3-5 page paper that examines a safety quality issue pertaining to medication administration in a health care setting. You will analyze the issue and examine potential evidence-based and best-practice solutions from the literature as well as the role of nurses and other stakeholders in addressing the issue.
Health care organizations and professionals strive to create safe environments for patients; however, due to the complexity of the health care system, maintaining safety can be a challenge. Since nurses comprise the largest group of health care professionals, a great deal of responsibility falls in the hands of practicing nurses.
Quality improvement (QI) measures and safety improvement plans are effective interventions to reduce medical errors and sentinel events such as medication errors, falls, infections, and deaths. A 2000 Institute of Medicine (IOM) report indicated that almost one million people are harmed annually in the United States, (Kohn et al., 2000) and 210,000–440,000 die as a result of medical errors (Allen, 2013).
The role of the baccalaureate nurse includes identifying and explaining specific patient risk factors, incorporating evidence-based solutions to improving patient safety and coordinating care. A solid foundation of knowledge and understanding of safety organizations such as Quality and Safety Education for Nurses (QSEN), the Institute of Medicine (IOM), and The Joint Commission and its National Patient Safety Goals (NPSGs) program is vital to practicing nurses with regard to providing and promoting safe and effective patient care.
You are encouraged to complete the Identifying Safety Risks and Solutions activity. This activity offers an opportunity to review a case study and practice identifying safety risks and possible solutions. We have found that learners who complete course activities and review resources are more successful with first submissions. Completing course activities is also a way to demonstrate course engagement.
Demonstration of Proficiency in Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
Competency 1: Analyze the elements of a successful quality improvement initiative.
- Explain evidence-based and best-practice solutions to improve patient safety focusing on medication administration and reducing costs.
Competency 2: Analyze factors that lead to patient safety risks.
- Explain factors leading to a specific patient-safety risk focusing on medication administration.
Competency 4: Explain the nurse’s role in coordinating care to enhance quality and reduce costs.
- Explain how nurses can help coordinate care to increase patient safety with medication administration and reduce costs.
- Identify stakeholders with whom nurses would need to coordinate to drive quality and safety enhancements with medication administration.
Competency 5: Apply professional, scholarly, evidence-based strategies to communicate in a manner that supports safe and effective patient care.
- Organize content so ideas flow logically with smooth transitions; contains few errors in grammar or punctuation, word choice, and spelling.
- Apply APA formatting to in-text citations and references exhibiting nearly flawless adherence to APA format.
References for Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety
- Allen, M. (2013). How many die from medical mistakes in U.S. hospitals? Retrieved from https://www.npr.org/sections/health-shots/2013/09/20/224507654/how-many-die-from-medical-mistakes-in-u-s-hospitals.
- Kohn, L. T., Corrigan, J., & Donaldson, M. S. (Eds.). (2000). To err is human: Building a safer health system. Washington, DC: National Academy Press.
Professional Context
As a baccalaureate-prepared nurse, you will be responsible for implementing quality improvement (QI) and patient safety measures in health care settings. Effective quality improvement measures result in systemic and organizational changes, ultimately leading to the development of a patient safety culture.
Scenario for Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety
Consider a previous experience or hypothetical situation pertaining to medication errors, and consider how the error could have been prevented or alleviated with the use of evidence-based guidelines.
Choose a specific condition of interest surrounding a medication administration safety risk and incorporate evidence-based strategies to support communication and ensure safe and effective care.
For this assessment:
- Analyze a current issue or experience in clinical practice surrounding a medication administration safety risk and identify a quality improvement (QI) initiative in the health care setting.
Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety Instructions
The purpose of this assessment is to better understand the role of the baccalaureate-prepared nurse in enhancing quality improvement (QI) measures that address a medication administration safety risk. This will be within the specific context of patient safety risks in a health care setting of your choice. You will do this by exploring the professional guidelines and best practices for improving and maintaining patient safety in healthcare settings from organizations such as QSEN and the IOM.
Looking through the lens of these professional best practices to examine the current policies and procedures currently in place at your chosen organization and the impact on safety measures for patients surrounding medication administration, you will consider the role of the nurse in driving quality and safety improvements. You will identify stakeholders in QI improvement and safety measures as well as consider evidence-based strategies to enhance the quality of care and promote medication administration safety in the context of your chosen healthcare setting.
Be sure that your plan addresses the following, which corresponds to the grading criteria in the scoring guide. Please study the scoring guide carefully so that you know what is needed for a distinguished score.
- Explain factors leading to a specific patient-safety risk focusing on medication administration.
- Explain evidence-based and best-practice solutions to improve patient safety focusing on medication administration and reducing costs.
- Explain how nurses can help coordinate care to increase patient safety with medication administration and reduce costs.
- Identify stakeholders with whom nurses would coordinate to drive safety enhancements with medication administration.
- Communicate using writing that is clear, logical, and professional, with correct grammar and spelling, using current APA style.
Additional Requirements for Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety
- Length of submission: 3–5 pages, plus title and reference pages.
- Number of references: Cite a minimum of 4 sources of scholarly or professional evidence that support your findings and considerations. Resources should be no more than 5 years old.
- APA formatting: References and citations are formatted according to current APA style.
Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety: Medication Safety Sample Paper 2
Medication errors have significantly affected patient safety, as some have led to mortality or disability. Despite significant improvements by our health system to mitigate these errors, medication safety is still a concern due to various causes.
The Food and Drug Administration (FDA) defines a medication error as an event capable of causing inappropriate medication use or patient harm in the hand of the prescriber, administering clinician, patient, or consumer of the medication (Center for Drug Evaluation & Research, 2019).
In the FDA’s definition, medication errors are preventable. The purpose of this paper is to describe a situation where a medication error occurred, explain the specific risks for the patient, and describe the best nursing coordination strategies to improve patient safety.
Patient Scenario
Charlie is a 22-year-old white male who had an emergency appendectomy following acute appendicitis. His pain persisted even on day four after the resumption of oral intake, and his surgeon prescribed oral morphine medication 10 mg start dose that evening. RN, the oncoming nurse that evening, administered 10 milliliters of morphine solution for injection infusion because the patient had been on other intravenous infusions in the postoperative period.
The formulation given contained a 10mg/ml solution. Three hours about half an hour minutes after the administration of this solution, Charlie started vomiting the milk he had taken that evening and appeared to be in respiratory distress. Therefore, RN called Charlie’s surgeon to review him.
Factors Leading to Patient-Safety Risk
Various patient safety risks could have led to this patient’s risk for medication errors. These errors relate to healthcare professional practice, products, procedures, and systems. These errors can be traced back to product labeling, packaging, prescription, administration, and monitoring.
These patient-safety risks related to medication administration include but are not limited to inadequate or unclear instructions, illegible writing, lack of medication reconciliation, improper administration documentation (Rosenthal & Burchum, 2020), inappropriate drug selection during administration, and failure to continue or discontinue medications. More than one risk can contribute to a single occurrence of medication error due to medication administration.
A qualitative study by Schroers et al. (2020) classified these patient safety risk factors in medication administration into personal factors and contextual factors. Personal factors include fatigue and complacency, while contextual factors include interruptions (Rosenthal & Burchum, 2020), night shift duty, unavailability of administration guidelines (Wondmieneh et al., 2020), and heavy nurse workloads. According to Rosenthal & Burchum (2020), about 60% of these medication errors occur during the care transition. Personal and contextual factors come into play at this time.
Improving Patient Safety Focusing on Medication Administration and Reducing Costs
Every healthcare organization continually works on various measures that they can use to prevent medication errors. Some of the evidence-based strategies to reduce medication errors, especially relating to medication administration, include but are not limited to the adoption of technology, bedside shift reporting, patient education, improving documentation in writing, and medication reconciliation. Adverse events from medication errors are too costly to the healthcare system and the patient. Treating adverse events due to medication increases the medical costs due to unintended patient harm and can cost the patient their lives.
The adoption of technology improves medication prescription and decision-making. According to Rosenthal & Burchum (2020), using technology reduces medication errors by 50%. The use of technology systems such as computerized physician order entry and computerized clinical decision support systems ensures that reduces errors of reception while the use of barcoded technology that identifies the drugs’ barcodes and against the patient information reduces errors of administration by up to 85% in some institutions (Rosenthal & Burchum, 2020). Therefore, technology can play a crucial role in the prevention of medication errors in the whole continuum of patient treatment.
Medication reconciliation is the process of comparing and updating the patient’s old and new medication lists. Medication reconciliation can be carried out at all care transitions, including inter-institutional transfer, admission, and discharge during shift reporting. About 60% of errors are reduced when medication reconciliation at all points of care transition. Bedside shift reporting offers an excellent opportunity for medication reconciliation during care transitions.
The Institute for Safe Medical Practices (ISMP) recommends using brand and generic names of medication during a prescription to ensure that during administration, the nurse is sure and less likely to make medication errors. The joint commission (TJC) banned the use of some abbreviations in prescriptions to reduce the chances of confusion during medication administration.
Improving documentation includes reserving verbal prescriptions for emergencies only. Documentation using electronic means ensures good communication between nurses, dispenses of medication, and prescribers of the medications. On the other hand, patient medication requires developing strong collaborative relationships that improve compliance with prescriptions to reduce the chances of medication errors (MacDowell et al., 2021). Education improves their understanding of the need for compliance and the potential side effects of overdose and toxicity.
Nursing Care Coordination to Increase Patient Safety
Nursing care is the center for care coordination in any healthcare institution. During care coordination, nurses organize patient care activities and share pertinent information with care stakeholders to ensure care effectiveness, safety, and quality (Agency for Healthcare Research and Quality, 2018). Care coordination aims at meeting patient care needs thus, the nurse needs to identify all patient needs and ensure they are met by the care providers. Some of the care coordination strategies that the nurse would employ include interprofessional collaboration and medication management.
For example, during interprofessional collaboration, the nurse can help with care transition, assess patient needs, and share all relevant information. The shared relevant information would be used to develop patient medication lists with a low risk of drug interaction and adverse events such as allergies. During care coordination, the nurse should also conduct medication reconciliation at every point of change in patient care providers. These two strategies would increase patient safety relating to medication administration.
Stakeholders During Care Coordination
The nursing care coordination must account for all relevant stakeholders of patient care. These stakeholders can be patient-specific and may not apply to all patient cases. Some of the key stakeholders that the nurse has to coordinate with include but are not limited to patient physicians, informaticists, pharmacists, patient caregivers, and the patient themselves. This coordination requires constant, timely communication and collaboration (Agency for Healthcare Research and Quality, 2018).
Collaboration with the patient or their caregivers would be important in safety monitoring and improving compliance with the prescription. Whenever in doubt, the nurse must coordinate with the prescribers of the patient medication lists to ensure that the correct drug and dosage are given to the patient, thereby lowering safety risks, especially due to administration. The nurse must coordinate with the pharmacists to ensure that the correct medication is dispensed. Their collaboration will also ensure that the risk of drug-drug interactions is lowered through medication reconciliation.
Another critical coordination is with fellow nurses. Collaboration with other nurses is essential in various ways. Firstly, it improves job satisfaction, thus lowering the chances of medication and medical errors. This interprofessional coordination and collaboration also enhance fast and smooth medication reconciliation (Tariq et al., 2022). This usually happens during shift handover. The exchange of other essential patient information at this time is also made easy through mutual information sharing and setting new care plans and care goals.
Conclusion
The medication error in this paper involved an overdose that could be due to a myriad of factors ranging from prescription to administration. Documented literature evidence has reported that medication errors due to medication administration arise from personal and contextual factors. Contextual factors are systemic and relate to the circumstances of the error occurrence. Personal factors related to complacency and fatigue from nurses.
To improve patient safety by preventing medication errors, the nurse should adopt strategies such as medication reconciliation, the use of technology, improving documentation, and patient education. Nursing care coordination strategies such as identifying patient needs and sharing information should involve all pertinent patient care stakeholders.
The patient caregivers, doctors, pharmacists, informaticists, the patient themselves, and other nurses and key stakeholders that the nurse will require to communicate and collaborate with to improve patient safety. Medication reconciliation at every point of care transition will be important during the coordination process.
Capella NURS-FPX4020 Assessment 1 Enhancing Quality and Safety Sample 2 References
- Agency for Healthcare Research and Quality. (2018, August). Care Coordination. Ahrq.gov. Retrieved from https://www.ahrq.gov/ncepcr/care/coordination.html
- Center for Drug Evaluation & Research. (2019, August 23). Working to Reduce Medication Errors. U.S. Food and Drug Administration. Retrieved from https://www.fda.gov/drugs/information-consumers-and-patients-drugs/working-reduce-medication-errors
- MacDowell, P., Cabri, A., & Davis, M. (2021). Medication Administration Errors. Intensive Care Medicine. https://psnet.ahrq.gov/primer/medication-administration-errors
- Rosenthal, L., & Burchum, J. (2020). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants (2nd ed.). Saunders. https://www.us.elsevierhealth.com/lehnes-pharmacotherapeutics-for-advanced-practice-nurses-and-physician-assistants-9780323936064.html
- Schroers, G., Ross, J. G., & Moriarty, H. (2020). Nurses’ perceived causes of medication administration errors: A qualitative systematic review. Joint Commission Journal on Quality and Patient Safety, 47(1), 38–53. https://doi.org/10.1016/j.jcjq.2020.09.010
- Tariq, R. A., Vashisht, R., Sinha, A., & Scherbak, Y. (2022). Medication dispensing errors and prevention. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK519065/
- Wondmieneh, A., Alemu, W., Tadele, N., & Demis, A. (2020). Medication administration errors and contributing factors among nurses: a cross-sectional study in tertiary hospitals, Addis Ababa, Ethiopia. BMC Nursing, 19(1), 4. https://doi.org/10.1186/s12912-020-0397-0
Resources: Collaboration and Leadership
Cho, S. M., & Choi, J. (2018). Patient safety culture associated with patient safety competencies among registered nurses. Journal of Nursing Scholarship, 50(5), 549–557. https://doi-org.library.capella.edu/10.1111/jnu.12413
- This article discusses the importance of creating a unit-specific patient safety culture that is tailored to the competencies of the unit’s RNs in patient safety practice.
SonÄŸur, C., Özer, O., Gün, C., & Top, M. (2018). Patient safety culture, evidence-based practice and performance in nursing. Systemic Practice and Action Research, 31(4), 359–374.
- Evidence-based practice is a problem-solving approach in which the best available and useful evidence is used by integrating research evidence, clinical expertise, and patient values and preferences to improve health outcomes, service quality, patient safety and clinical effectiveness, and employee performance.
Stalter, A. M., & Mota, A. (2017). Recommendations for promoting quality and safety in health care systems. The Journal of Continuing Education in Nursing, 48(7), 295–297.
- This article provides recommendation to promote quality and safety education with a focus on systems thinking awareness among direct care nurses. A key point is error prevention, which requires a shared effort among all nurses.
Manno, M. S. (2016). The role transition characteristics of new registered nurses: A study of work environment influences and individual traits. (Publication No. 10037467) [Doctoral dissertation, Capella University].
- This research study may be helpful in identifying traits and qualities of new registered nurses that are helpful in coordinating and leading quality and safety measures related to this assessment.
Boomah, S. A. (2018). Emergence of informal clinical leadership as a catalyst for improving patient care quality and job satisfaction. Journal of Advanced Nursing. 75(5), 1000–1009. https://doi-org.library.capella.edu/10.1111/jan.13895
- This research analyzes attributes and best practices of leadership and nursing staff that help aid in patient care quality and job satisfaction.
Greenstein, T. (2020). Leading innovation is completely different from leading change. WWD.com.
- This article examines competencies that may help nurses collaborate more effectively to improve patient outcomes.
Poder, T. G., & Mattais, S. (2018). Systemic analysis of medication administration omission errors in a tertiary-care hospital in Quebec. Health Information Management Journal, 49(2-3), 99–107.
- This examination of underlying systemic causes of medication errors may be useful as you consider QI vest practices and ways to coordinate care to increase safety and quality.
Antevy, P. (2017). How care collaboration is improving patient outcomes. EMS World, 46(4), 26–33.
- This article examines competencies that may help health care professionals collaborate more effectively to improve patient outcomes.
Keers, R. N., Plácido, M., Bennet, K., Clayton, K., Brown, P., & Ashcroft, D. M. (2018, October 26). What causes medication administration errors in a mental health hospital? A qualitative study with nursing staff. PLOS One. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0206233
- This examination of underlying systemic causes of medication errors may be useful as you consider QI best practices and ways to coordinate care to increase safety and quality.
Quality and Safety Education
Lyle-Edrosolo, G., & Waxman, K. (2016). Aligning healthcare safety and quality competencies: Quality and safety education for nurses (QSEN), the Joint Commission, and American Nurses Credentialing Center (ANCC) Magnet® standards crosswalk. Nurse Leader, 14(1), 70–75.
- This artic
READ MORE >>
Capella NURS-FPX6011 Assessment 1 EBP Assignment ExamplePart 1: Concept MapPart ...
Capella NURS-FPX6011 Assessment 1 EBP Assignment Example
Part 1: Concept Map
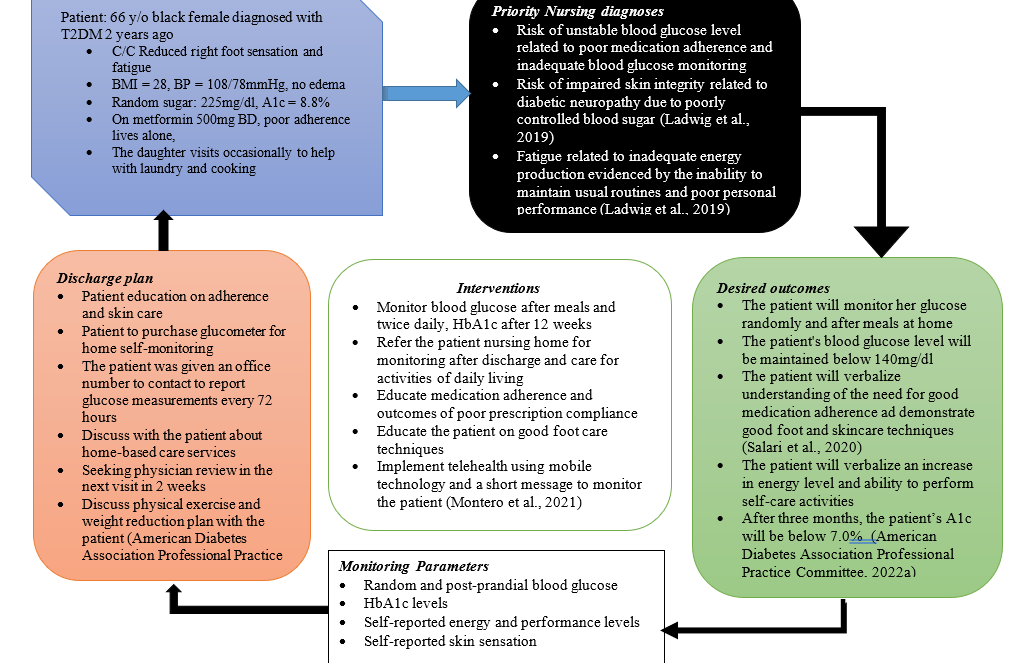
Part 2: Supporting the Concept Map
The development of this concept map was guided by the nursing process. This patient came into the office with a chief complaint of reduced sensation on the right foot that was on and off but mild in functional limitation. The assessment revealed no other symptoms related to renal, ophthalmic, gastrointestinal, or cardiac complications of diabetes. The purpose of this narrative review of the concept map is to describe how evidence-based practice influenced this concept map and care plan in terms of analysis of the patient’s needs, communication with the patient and her family, and the value of the evidence-based sources used.
Patient Needs Analysis
During this visit, the patient’s main concerns were the reduction of right lower limb and foot sensation and fatigue. On further probing, the assessment found that this patient’s compliance with her metformin has been erratic and her socioeconomic circumstances could have also contributed to her current situation. She has missed most of her doses in the past few months because her daughter, who used to remind her to take her pills, moved to another state for permanent employment and has been held up with work lately.
The patient is retired; thus, her primary source of income is through her son and daughter, who are both employed. Her children are both married but still find time to come and visit. This patient is a staunch Christian believer and she reports that her faith has kept her through to this time. This might have contributed to the reluctance to comply fully with her prescription. Nevertheless, this patient’s cultural and socioeconomic needs greatly influenced the development of this concept map and the care plan.
The patient lives alone; thus, this care plan instituted monitoring strategies to ensure that the patient achieves self-care by improving her fatigue. Priority was given to stabilizing blood sugar levels and improving adherence to ensure that her metabolic demands were met. Monitoring through telehealth and mobile technology was a vital part of this plan because it would enable remote management of the patient through enhanced follow-up after short time intervals. In the discharge plan, the patient was helped to create a plan that included an alarm to remind her about her medication time and times to record her blood glucose to report three days later.
The development of the patient was also influenced by her identity and cultural needs. As an African American, she is at risk of cardiovascular diseases such as heart failure. Therefore, an assessment of her blood pressure and cardiovascular complication, such as lower limb edema from heart failure and acute kidney injury, was justified for this patient. This patient is overweight (BMI=28), which adds to her cardiovascular risk. Therefore, the inclusion of exercise and a weight reduction plan through diet were discussed during a motivational interviewing session.
The interventions were driven at meeting care needs illustrated in the three priority diagnoses. Most of the desired outcomes of these interventions were intertwined and such that more than one intervention could be used to meet a single outcome. Therefore, I included the monitoring outcomes measurement parameters that would be discussed with the patient during every review session after every 72 hours. The patient’s family was included in this plan through her daughter, who accompanied her to the office. She desired to treat her mother from home even if it meant that the care costs would increase. Therefore, I added community resources such as home-based care interventions to improve this patient’s self-care at home.
Communication Strategies.
The communication plan with this patient and her family will involve both remote and face-to-face communication. Remote communication through telehealth would help monitor patient progress and scheduling appointments. After every four weeks, the patient would revisit the officer for physical assessment and face-to-face communication. To ensure that these communications were honest and productive. The communication times would be scheduled and contents tailored to meet the patient’s care needs.
The patient’s daily readings would be communicated through phone calls but charted on paper to be delivered during physical sessions. This would ensure that only important and useful is shared, but every detail is documented for monitoring and evaluation. The content of the communication with the patient and her family will be kept short and basic so that they would understand and follow through with her care.
Value and Relevance of Resources
Four evidence-based sources informed this care plan. These sources have different values and relevance to making the concept map. The annotated bibliography below explains how these sources were valuable ad relevant.
American Diabetes Association Professional Practice Committee. (2022a). 4. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in diabetes—2022. Diabetes Care, 45(Supplement_1), S46–S59. https://doi.org/10.2337/dc22-s004
This source provided information on current evaluation and assessment strategies relevant to the nursing process. This piece of information was relevant to this patient’s case because it ensures that my care was multisystemic and, thus, holistic and patient-centered. This article provides level I evidence in the hierarchy of evidence because it contains evidence-based guidelines. The value of the information herein is critical to patient safety and quality of care.
American Diabetes Association Professional Practice Committee. (2022b). 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in diabetes—2022. Diabetes Care, 45(Supplement_1), S60–S82. https://doi.org/10.2337/dc22-s005
This resource was a peer review article that provided information on the current management of diabetes and the incorporation of mental health outcomes relevant to this patient. This piece of information was relevant to this patient’s case because it ensured that my care was multisystemic and, thus, holistic and patient-centered. This article provides level I evidence in the hierarchy of evidence because it contains evidence-based guidelines by a recognized and reputable organization, the American Diabetes Association.
Ladwig, G. B., Ackley, B. J., & Makic, M. B. F. (2019). Mosby’s guide to nursing diagnosis (6th ed.). Mosby.
This resource is a course book and a tertiary source of information. The content of this source is heterogeneous and sourced from different primary and secondary articles and guidelines. The quality of evidence in this resource is high but can’t be ranked in the hierarchy because this resource doesn’t contain a single topic of information. This resource was vital in needs assessment and making priority diagnoses for this patient that are related to NANDA diagnoses. This information was also important for goal setting for the care of this patient.
Montero, A. R., Toro-Tobon, D., Gann, K., Nassar, C. M., Youssef, G. A., & Magee, M. F. (2021). Implications of remote monitoring Technology in Optimizing Traditional Self-Monitoring of blood glucose in adults with T2DM in primary care. BMC Endocrine Disorders, 21(1), 222. https://doi.org/10.1186/s12902-021-00884-6
This source of information was the primary source with the information I used in the selection of the best and most appropriate technology for communication to meet this patient’s needs. The use of technology would ensure self-monitoring of glucose by this patient and this would improve outcomes. This source is level II evidence because it was from a comparative experimental study with no randomization.
Salari, N., Hosseinian-Far, A., Hosseinian-Far, M., Kavoussi, H., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Rasoulpoor, S., Mohammadi, M., & Shabani, S. (2020). Evaluation of skin lesions in diabetic patients: a systematic review and meta-analysis. Journal of Diabetes and Metabolic Disorders, 19(2), 1909–1916. https://doi.org/10.1007/s40200-020-00629-7
The value of this article in the management of this patient is high because it is a level-I evidence source that addresses this patient’s chief complaint. This source is a systemic review with meta-analyses; thus, it provides the highest level of evidence (Melnyk & Fineout-Overholt, 2023). This article provides information about current best practices regarding skin care among diabetic patients. Therefore, it is relevant to this patient’s case.
The above five sources are credible because they meet the CRAAP criteria for credibility. The CRAAP credibility test is an acronym that stands for currently, relevance, accuracy, authoritativeness, and purpose. I used sources published within the last five years, thus current. These sources were published by an expert in nursing and medical fields and are thus authoritative. The purpose and relevance of the sources had been annotated earlier.
Conclusion
The concept map presented summarized the patient assessment findings, presented three priory nursing diagnoses and elaborated a care plan for the patient. The desired outcomes of the patient care plan were based on an assessment of the patient’s needs. These needs were related to the patient’s current social, economic, cultural, and self-care status. This plan was evidence based because the information that guided its development was derived from five credible sources.
Capella NURS-FPX6011 Assessment 1 EBP Assignment References
American Diabetes Association Professional Practice Committee. (2022a). 4. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in diabetes—2022. Diabetes Care, 45(Supplement_1), S46–S59. https://doi.org/10.2337/dc22-s004
American Diabetes Association Professional Practice Committee. (2022b). 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in diabetes—2022. Diabetes Care, 45(Supplement_1), S60–S82. https://doi.org/10.2337/dc22-s005
Ladwig, G. B., Ackley, B. J., & Makic, M. B. F. (2019). Mosby’s guide to nursing diagnosis (6th ed.). Mosby.
Melnyk, B. M., & Fineout-Overholt, E. (2023). Evidence-based practice in nursing & healthcare: A guide to best practice (5th ed.). Wolters Kluwer Health.
Montero, A. R., Toro-Tobon, D., Gann, K., Nassar, C. M., Youssef, G. A., & Magee, M. F. (2021). Implications of remote monitoring Technology in Optimizing Traditional Self-Monitoring of blood glucose in adults with T2DM in primary care. BMC Endocrine Disorders, 21(1), 222. https://doi.org/10.1186/s12902-021-00884-6
Salari, N., Hosseinian-Far, A., Hosseinian-Far, M., Kavoussi, H., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Rasoulpoor, S., Mohammadi, M., & Shabani, S. (2020). Evaluation of skin lesions in diabetic patients: a systematic review and meta-analysis. Journal of Diabetes and Metabolic Disorders, 19(2), 1909–1916. https://doi.org/10.1007/s40200-020-00629-7
Capella NURS-FPX6011 Assessment 1 EBP Assignment Instructions
Create an evidence-based, patient-centered concept map that illustrates an individualized approach to patient care based on a patient case file of your choice.
Evidence-based practice is a critical skill in the toolkit of the master’s-prepared nurse. Its goal is to ensure that healthcare practitioners use the best available evidence to ensure patients receive the best care possible (Godshall, M., 2015.). In essence, evidence-based practice is all about providing quality care Capella FP6011 Assessment 1 EBP Assignment.
In this assessment, you can apply evidence-based practice and personalized care concepts to ensure quality care and improve a single patient’s health.
Completing this assessment will demonstrate your proficiency in the following course competencies and assessment criteria Capella FP6011 Assessment 1 EBP Assignment.
Competency 1: Apply evidence-based practice to plan patient-centered care.
Analyze the needs of a patient and their family about how they will influence a patient-centered concept map.
Design an individualized, patient-centered concept ma, based on the best available evidence for treating a patient’s health, economic, and cultural needs.
Competency 3: Evaluate outcomes of evidence-based interventions.
Propose relevant and measurable criteria for evaluating the outcomes of a patient-centered concept map.
Competency 4: Evaluate available evidence’s value and relative weight to make a clinical decision.
Justify the value and relevance of evidence used for a patient-centered concept map.
Competency 5: Synthesize evidence-based practice and academic research to communicate effective solutions.
Develop a strategy for communicating with patients and their families in an ethical, culturally sensitive, and inclusive way.
Integrate relevant and credible sources of evidence to support assertions, correctly formatting citations and references using APA style.
Capella NURS-FPX6011 Assessment 1 EBP Assignment Reference:
Godshall, M. (2015). Fast facts for evidence-based practice in nursing: Implementing EBP in a nutshell(2nd ed.). New York, NY: Springer Publishing Company.
Preparation for Capella NURS-FPX6011 Assessment 1 EBP Assignment
You have been presented with several patient case files in the Evidence-Based Patient-Centered Care media piece Capella FP6011 Assessment 1 EBP Assignment. You reviewed each case, selected one point for further research, and created a draft evidence-based concept map to illustrate an approach to individualized care for the patient. In this assessment, you will build upon and refine your draft concept map and develop a supporting narrative.
Create your concept map and narrative as separate documents. Be sure to note the areas where you need to include your evidence-based support and where you need to make clear your strategies for communicating information to the patient and the patient’s family.
Note: Many organizations use the spider style of concept maps (see the Taylor & Littleton-Kearney article for an example). Also, if a specific type of concept map is used in your current care setting, you may use it in this assessment.
Create your concept map and narrative as separate documents. Be sure to note the areas where you need to include your evidence-based support and where you need to make clear your strategies for communicating information to the patient and the patient’s family Capella FP6011 Assessment 1 EBP Assignment.
Requirements for Capella NURS-FPX6011 Assessment 1 EBP Assignment

Note: The requirements below correspond to the grading criteria in the scoring guide, so address each point. In addition, you may want to review the performance level descriptions for each bar to see how your work will be assessed.
Supporting Evidence and APA Style
Integrate relevant evidence from 3–5 current scholarly or professional sources to support your assertions.
Apply correct APA formatting to all in-text citations and references.
Attach a reference list to your narrative.
Concept Map
Develop a concept map for the individual patient based on the best available evidence for treating your patient’s health, economic, and cultural needs.
Narrative
Develop a narrative (2–4 pages) for your concept map.
Analyze the needs of your patient and their family, and determine how those needs will influence a patient-centered concept map.
Consider how your patient’s economic situation and relevant environmental factors may have contributed to your patient’s current condition and affected their future health.
Consider how your patient’s culture or family should influence your concept map.
Justify the value and relevance of the evidence you used as the basis of your concept map.
Explain why your evidence is valuable and relevant to your patient’s case.
Explain why each piece of evidence is appropriate for both the health issue you are trying to correct and for the unique situation of your patient and their family.
Propose relevant and measurable criteria for evaluating the degree to which the desired outcomes of your concept map were achieved.
Explain why your proposed criteria are appropriate and valid measures of success.
Explain how you will communicate specific aspects of the concept map to your patient and their family in an ethical, culturally sensitive, and inclusive way. Ensure that your strategies:
- Promote honest communications.
- Facilitate sharing only the information you are required and permitted to share.
- Are mindful of your patient’s culture.
- Enable you to make complex medical terms and concepts understandable to your patient and their family, regardless of language, disabilities, or level of education.
Capella NURS-FPX6011 Assessment 1 EBP Assignment Additional Requirements
Be sure to include both documents when you submit your assessment.
Also Read:
Select NURS FPX 4040 Technology in Nursing Annotated BibliographyNURS FPX 4040 Technology in Nursing Annotated BibliographySelect MSNFP6016 Capella University Quality Improvement Initiative EvaluationMSNFP6016 Capella University Quality Improvement Initiative EvaluationREAD MORE >>
Capella PSYC3770 Human Treatment and Prevention of Obesity AssignmentHuman Motiv ...
Capella PSYC3770 Human Treatment and Prevention of Obesity Assignment
Human Motivation and Performance
For the course project, you are required to write a paper on a topic related to human motivation and performance. You developed your topic in Unit 2 and wrote an annotated bibliography in Unit 5.
In this unit, you will submit your finished course project paper for grading. Your paper should be 7–9 pages, not including your title page and reference page, with a minimum of six references from scholarly resources. Be sure to complete the following in your final paper:

- Apply a minimum of two theories or models to your selected topic related to human motivation and performance.
- Describe the components of behavior or motivation (biological, learned, or cognitive processes) as related to the topic you have selected.
- Apply knowledge of theories of human motivation and performance to explain human motivation, behavior, and goals in regard to your topic.
- Apply findings from research to the understanding of your topic.
- Analyze how theory and research findings inform personal behavior, professional goals, and the development of social policy.
- Capella PSYC3770 Human Treatment and Prevention of Obesity Assignment
- Follow current APA style and formatting guidelines.
SUBMISSION REQUIREMENTS
- Written communication: Written communication is free of errors that detract from the overall message.
- Capella PSYC3770 Human Treatment and Prevention of Obesity Assignment
- APA formatting: Resources and citations are formatted according to current APA style and formatting.
- Number of resources: Minimum of six resources.
- Length of paper: 7–9 typed, double-spaced pages, not including title page and reference page.
- Font and font size: Times New Roman, 12 point.
Portfolio Prompt: You may choose to save this learning activity to your ePortfolio for Program Outcome 1, 2, 3, 4, 5, 6, or 7.
Capella PSYC3770 Human Treatment and Prevention of Obesity Assignment Resources
- Human Motivation and Performance Scoring Guide.
- APA Style Paper Template.
- Capella University Library Undergraduate Research Guide.
- Writing Center.
- ePortfolio.
- APA Style and Format.
You must proofread your paper. But do not strictly rely on your computer’s spell-checker and grammar-checker; failure to do so indicates a lack of effort, and you can expect your grade to suffer accordingly. Papers with numerous misspelled words and grammatical mistakes will be penalized.
Read over your paper – in silence and then aloud – before handing it in, and make corrections as necessary. Often, having a friend proofread your paper for obvious errors is advantageous. Handwritten corrections are preferable to uncorrected mistakes Capella PSYC3770 Human Treatment and Prevention of Obesity Assignment.
Use a standard 10 to 12-point (10 to 12 characters per inch) typeface. Smaller or compressed type and papers with small margins or single-spacing are hard to read. Letting your essay run over the recommended number of pages is better than compressing it into fewer pages.
Likewise, large type, large margins, large indentations, triple-spacing, increased leading (space between lines), increased kerning (space between letters), and any other such attempts at “padding” to increase the length of a paper are unacceptable, wasteful of trees, and will not fool your professor.
The paper must be neatly formatted and double-spaced with a one-inch margin on each page’s top, bottom, and sides. When submitting a hard copy, use white paper and print it out using dark ink. If it is hard to read your essay, it will also be hard to follow your argument Capella PSYC3770 Human Treatment and Prevention of Obesity Assignment.
Building a Comprehensive Health History on Patient Suffering from Obesity
Building health history is the first step to managing the patient because the history contributes a significant role in making the diagnosis and influencing the choice of treatment. A more comprehensive history also directs more relevant investigations and laboratory tests. The process of building a health history requires good communication skills and techniques to collect more comprehensive and accurate information for diagnosis, investigations, and management purposes. My assigned patient case scenario is an adult patient – a 35-year-old male with morbid obesity. He lives in a rural setting. The purpose of this discussion is to present a summary of the interview that I would have with this patient, the best communication techniques to build this health history, and the risk assessment tool that I would apply to this patient’s case.
Summary of the Interview
My interview with this patient would aim at building a comprehensive health history as well as setting up a relationship for future engagement in his care and follow-up. My interview with the patient addressed the reasons for this patient’s visit to the care center, the duration he has been unwell, who else has similar illnesses, which interventions he has sought or taken for his illnesses, and what would have led to him having that illness, and how his environment may have contributed to his reasons for the visit to the care center.
Therefore, this interview seeks to address the etiologies, risk factors, presenting clinical signs and symptoms, management so far, and any other issue relevant to the patient and not necessarily the reason for presentation. The interview addresses the factors leading to the unwellness by seeking to clarify the precipitating factors, maintaining factors, and risks. To acquire these sensitive pieces of information from the patient I would employ certain communication techniques – both verbal and nonverbal.
Communication techniques
Effective communication, according to Ball et al. (2022), leads to a positive patient relationship and relies on building confirmation, courtesy, comfort, and connection. According to Diamond-Fox (2021), poor patient communication contributes to poor healthcare quality. Therefore, developing an effective advanced clinical practitioner-patient relationship through communication requires the employment of certain skills that do not work on every patient case. Therefore, patient-centered communication and identification of communication requirements would be an effective first step. There are several communication techniques that I would use to achieve these concepts in my clinical interview.
I would ensure courtesy and connection with the patient by welcoming him to the interview, ensuring he is as comfortable as he could be, and explaining to him the content and purpose of the interview. This courtesy process will also include seeking the patient’s verbal and intended consent before introducing him to the interview. In my interview, I also avoid the use of medical jargon to ensure that the patient understands me with ease. Reassurance to the patient about the confidentiality of our interview will create a rapport and good relationship to allow openness and comprehensiveness of their responses.
Keeping the questions simple and direct will help me avoid overload (Diamond-Fox, 2021). I will also use normalizing questions to avoid or minimize the patient’s sense of embarrassment bearing in mind that this patient is morbidly obese and most likely has developed body image and self-esteem issues (Bouzas et al., 2019; Yazdani et al., 2020). By employing these techniques, I will get a clue about the patient’s risk factors leading to his obesity and the best ways to tackle patient education or other interventions. The use of risk assessment tools would also objectively diagnose this patient’s risk factors.
Risk Assessment
The patient is at risk of various systemic and organ-specific diseases such as diabetes mellitus, heart failure, dyslipidemia, ischemic heart disease, and stroke. Risk assessment is an objective process and helps the clinician qualify and quality the risks of the patient. In this patient, I would use the body mass index as the initial assessment tool for her risks associated with obesity. The body mass index tool is a product of the division of the patient’s weight in kilograms and the square of their height in meters.
The result of the BMI is expressed as a ratio and there are cutoffs for objectively classifying the severity of his obesity (Crum et al., 2019). Morbid obesity would give a BMI above 40 and this value gives information about the severity of his risk of development of cardiovascular disorders (Good et al., 2021). The value will also determine the next risk assessment for specific diseases associated with morbid obesity. The use of objectively targeted questions would also assess those specific risks.
Targeted Question
Risk assessment of this patient using targeted questions would be established by the use of questions that the interviewer or the examiner feels would give them appropriate reopposes (Benwell & Rhys, 2018). These are some of the targeted questions that I would use to perform risk assessments:
- Do you have diabetes or heart disease?
- Is there anyone with heart disease or diabetes in your family?
- Have felt excess thirst, hunger, or weight loss recently?
- How often in a day do you go to pass urine?
- Are there tasks that you used to perform before that you can’t do nowadays as a result of your condition?
References
Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2022). Seidel’s guide to physical examination: An interprofessional approach (10th ed.). Elsevier – Health Sciences Division.
Benwell, B., & Rhys, C. S. (2018). Negotiating relevance in pre-operative assessments. Social Science & Medicine (1982), 200, 218–226. https://doi.org/10.1016/j.socscimed.2018.01.034
Bouzas, C., Bibiloni, M. D. M., & Tur, J. A. (2019). Relationship between body image and body weight control in overweight ?55-year-old adults: A systematic review. International Journal of Environmental Research and Public Health, 16(9), 1622. https://doi.org/10.3390/ijerph16091622
Crum, A., Flanders, C., Wheaton, R., Morgan, A., Kiss, J., & Ludy, M. (2019). Assessment of cardiovascular risk in first-semester college students. Journal of the Academy of Nutrition and Dietetics, 119(9), A70. https://doi.org/10.1016/j.jand.2019.06.199
Diamond-Fox, S. (2021). Undertaking consultations and clinical assessments at an advanced level. British Journal of Nursing (Mark Allen Publishing), 30(4), 238–243. https://doi.org/10.12968/bjon.2021.30.4.238
Good, M., Braun, A. C., Taylor, C. A., & Spees, C. K. (2021). US adults fall short of the dietary guidelines for cancer prevention regardless of BMI category. Journal of the Academy of Nutrition and Dietetics. https://doi.org/10.1016/j.jand.2021.02.013
Yazdani, N., Elahi, N., Sharif, F., Hosseini, S. V., & Ebadi, A. (2020). The comparison of morbid obesity quality of life and body image between surgery and other treatments: A case-control study. Journal of Education and Health Promotion, 9, 25. https://doi.org/10.4103/jehp.jehp_400_18
READ MORE >>
Capella University NURS FPX 4050 Caring for Alzheimers Patient Discussion – P ...
Capella University NURS FPX 4050 Caring for Alzheimers Patient Discussion – Preliminary Care Coordination Plan Example Paper
Selected Health Concern
Mental health has become a global concern in recent years. Despite the increasing incidence of this illness, stakeholders have not given it the necessary attention. The National Institute of Mental Health (2022) reports that one in five adults in the United States lives with a mental illness, representing about 52.9 million people in 2020. These people are afflicted with incapacitating impairments that substantially impact their daily lives.
As a result of this insurmountable, afflicted persons believe that their difficulties lack legitimacy because they are uncommon in contrast to other illnesses. Sufferers with apparent health impairments in their ability to accomplish numerous errands are treated with derision, whereas the general public views mental health patients as having irrelevant worries.
Despite the fact that mental health conditions and invulnerable health concerns may not be indicative of a successful life, success is frequently associated with the availability of community resources and treatment alternatives. In low-income countries, more than 75% of mental health patients go untreated, while 35 to 50 % of high-income patients do not seek medical care and go untreated (Qin & Hsieh, 2020). This trend has a negative impact on the fight against mental illness.
Additionally, more than $280 billion are lost annually in the United States providing services and treating mental health issues (The White House, 2022). Furthermore, according to the National Alliance on Mental Illness (2021), major depressive episodes, anxiety disorders, posttraumatic stress disorder, and bipolar disorder are leading causes of hospitalization for adults. Consequently, mental health problems remain a global hazard.
In addition, these diseases influence numerous social and economic areas. Among other aspects of life, mental health illnesses affect a person’s schooling abilities, work chances, and ability to maintain healthy interpersonal relationships. Therefore, seeking medical care and utilizing available community services is essential to living a mentally healthy life. In this view, the purpose of this project is to focus on a community member with a mental health disorder. The study’s primary objective is to design a care coordination plan.
The case patient has a mental illness (a depressive episode). During the evaluations, it becomes apparent that his family and acquaintances are willing to care for him. However, their assistance is insufficient, and they fail to comprehend the patient’s financial constraints in meeting his family’s demands. In addition, the patient sets unrealistic ambitions to conserve most of his resources, leaving his family with inadequate financial assistance. He desires to spend as little as possible on his healthcare. The patient’s worries necessitate discussing with mental health care specialists and developing a treatment plan appropriate to the community’s existing resources.
Community Resources Available for Effective and safe Care Continuum
The patient can benefit from a variety of support services aimed to help patients achieve mental health. First, Mental Health America (MHA) is committed to promoting mental health wellness by providing early identification and interventions for people at risk, integrating support, care, and services, with the sole goal of mental wellness recovery. It provides an affiliate network of mental health organizations to influence public policy and ensure access to reasonable and effective care for the vast number of mental health patients in the United States.
Operating in 42 states and with more than 200 affiliates, the MHA’s affiliate network is committed to providing assistance and advocacy to all individuals affected in all communities throughout the United States (Mental Health America (MHA), 2022). The affiliates provide outstanding programs and services specifically designed to address the needs of an area. The case patient can access information, mental health care, and a rehabilitation program through the affiliate network of the Mental Health Association.
Other resources include Substance Abuse Treatment Facility Locator, which assists individuals in locating programs with affordable payment options and links to support institutions. In addition, the National Suicide Prevention Lifeline provides vital support to those with mental health by connecting them to a local crisis center where they can seek emergency care. There is a toll-free number for this service. Therefore, one can select the choice that best meets their needs from among these options. However, he needs assistance in recognizing the existence of such resources and gaining access to them.
The Care Coordination Plan
Given the delicate nature of mental health issues, it is crucial to utilize effective and evidence-based approaches supported by the best clinical expertise, evidence, and research to give the highest possible level of care. A suitable intervention must be effective, well-defined, consider the patient’s goals, and comply with society norms (Lyon & Bruns, 2019). In addition, it should not be prohibitively expensive and should be adaptable to changing demands from patients and the community. According to this point of view, the healthcare professional and the patient need to work together to establish health goals that both parties are comfortable with.
The patient identified for this case resides within New York City. We planned an interview in two weeks and identified several objectives. One of them is to identify individuals who can offer unconditional support. Since his family is reluctant to provide support, the patient is encouraged to engage in social activities to help him identify new persons who can offer invaluable support.
Nevertheless, the relatives are also encouraged to adopt a more accepting and supportive attitude towards the patient. This would go a long way in enhancing the patient’s mental health and general well-being. Treating a patient in isolation from his family is doomed to fail. Therefore, incorporating the family members in the care coordination plan is vital.
Moreover, the patient is encouraged to value himself, avoid negative self-evaluation and criticism, and treat himself respectively. The patient should also be able to live without undue fear or guilt, work more productively and provide positive input to his family and community, establish more meaningful and healthy interpersonal relationships, accurately appraise reality, and attain a self-defined spiritual view.
These goals are all realistic and achievable. After identifying them, the patient should gradually focus on how to achieve them. Whenever he encounters unprecedented or considerably weighing down challenges, the patient should seek the available support from resources and personnel. He should also adhere to any prescribed treatment and therapeutic activities. Lastly, the patient should adopt healthy coping mechanisms to stress to avoid relapses and further deterioration of his state.
Capella University NURS FPX 4050 Caring for Alzheimers Patient Discussion References
Lyon, A. R., & Bruns, E. J. (2019). From Evidence to Impact: Joining Our Best School Mental Health Practices with Our Best Implementation Strategies. School Mental Health. https://doi.org/10.1007/s12310-018-09306-w
Mental Health America (MHA). (2022). About Mental Health America. Mental Health America. https://mhanational.org/about
National Alliance on Mental Illness. (2021). Mental health by the numbers. Nami.org; National Alliance on Mental Illness. https://www.nami.org/mhstats
National Institute of Mental Health. (2022, January). Mental Illness. https://www.nimh.nih.gov/health/statistics/mental-illness
Qin, X., & Hsieh, C.-R. (2020). Understanding and Addressing the Treatment Gap in Mental Healthcare: Economic Perspectives and Evidence From China. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 57, 004695802095056. https://doi.org/10.1177/0046958020950566
The White House. (2022, May 31). Reducing the Economic Burden of Unmet Mental Health Needs. The White House. https://www.whitehouse.gov/cea/written-materials/2022/05/31/reducing-the-economic-burden-of-unmet-mental-health-needs/
Capella University NURS FPX 4050 Caring for Alzheimers Patient Discussion Instructions
Develop a 3-4 page preliminary care coordination plan for a selected health care problem. Include physical, psychosocial, and cultural considerations for this health care problem. Identify and list available community resources for a safe and effective continuum of care.
NOTE: You are required to complete this assessment before Assessment 4.
The first step in any effective project or clinical patient encounter is planning. This assessment provides an opportunity for you to strengthen your understanding of how to plan and negotiate the coordination of care for a hypothetical individual in your community as you consider the hypothetical patient’s unique needs; the ethical, cultural, and physiological factors that affect care; and the critical resources available in your community that are the foundation of a safe plan for the continuum of care.
As you begin to prepare this assessment, you are encouraged to complete the Care Coordination Planning activity. Completion of this will provide useful practice, particularly for those of you who do not have care coordination experience in community settings. The information gained from completing this activity will help you succeed with the assessment. Completing formatives is also a way to demonstrate engagement.
Capella University NURS FPX 4050 Caring for Alzheimers Patient Discussion – DEMONSTRATION OF PROFICIENCY
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
- Competency 1: Adapt care based on patient-centered and person-focused factors.
- Analyze a health concern and the associated best practices for health improvement.
- Competency 2: Collaborate with patients and family to achieve desired outcomes.
- Describe specific goals that should be established to address a selected health care problem.
- Competency 3: Create a satisfying patient experience.
- Identify available community resources for a safe and effective continuum of care.
- Competency 6: Apply professional, scholarly communication strategies to lead patient-centered care.
- Organize content so ideas flow logically with smooth transitions; contains few errors in grammar/punctuation, word choice, and spelling.
- Apply APA formatting to in-text citations and references, exhibiting nearly flawless adherence to APA format.
PREPARATION for Capella University NURS FPX 4050 Caring for Alzheimers Patient Discussion
Imagine that you are a staff nurse in a community care center. Your facility has always had a dedicated case management staff that coordinated the patient plan of care, but recently, there were budget cuts and the case management staff has been relocated to the inpatient setting.
Care coordination is essential to the success of effectively managing patients in the community setting, so you have been asked by your nurse manager to take on the role of care coordination. You are a bit unsure of the process, but you know you will do a good job because, as a nurse, you are familiar with difficult tasks.
As you take on this expanded role, you will need to plan effectively in addressing the specific health concerns of community residents.
To prepare for this assessment, you may wish to:
- Review the assessment instructions and scoring guide to ensure that you understand the work you will be asked to complete.
- Allow plenty of time to plan your chosen health care concern.
Note: Remember that you can submit all, or a portion of, your draft plan to Smarthinking Tutoring for feedback, before you submit the final version for this assessment. If you plan on using this free service, be mindful of the turnaround time of 24–48 hours for receiving feedback.
Capella University NURS FPX 4050 Caring for Alzheimers Patient Discussion
INSTRUCTIONS
Note: You are required to complete this assessment before Assessment 4.
Develop the Preliminary Care Coordination Plan
Complete the following:
- Identify a health concern as the focus of your care coordination plan. In your plan, please include physical, psychosocial, and cultural needs. Possible health concerns may include, but are not limited to:
- Stroke.
- Heart disease (high blood pressure, stroke, or heart failure).
- Home safety.
- Pulmonary disease (COPD or fibrotic lung disease).
- Orthopedic concerns (hip replacement or knee replacement).
- Cognitive impairment (Alzheimer’s disease or dementia).
- Pain management.
- Mental health.
- Trauma.
- Identify available community resources for a safe and effective continuum of care.
Document Format and Length
- Your preliminary plan should be an APA scholarly paper, 3–4 pages in length.
- Remember to use active voice, this means being direct and writing concisely; as opposed to passive voice, which means writing with a tendency to wordiness.
- In your paper include possible community resources that can be used.
- Be sure to review the scoring guide to make sure all criteria are addressed in your paper.
- Study the subtle differences between basic, proficient, and distinguished.
Supporting Evidence
Cite at least two credible sources from peer-reviewed journals or professional industry publications that support your preliminary plan.
Grading Requirements
The requirements, outlined below, correspond to the grading criteria in the Preliminary Care Coordination Plan Scoring Guide, so be sure to address each point. Read the performance-level descriptions for each criterion to see how your work will be assessed.
- Analyze your selected health concern and the associated best practices for health improvement.
- Cite supporting evidence for best practices.
- Consider underlying assumptions and points of uncertainty in your analysis.
- Describe specific goals that should be established to address the health care problem.
- Identify available community resources for a safe and effective continuum of care.
- Organize content so ideas flow logically with smooth transitions; contains few errors in grammar/punctuation, word choice, and spelling.
- Apply APA formatting to in-text citations and references, exhibiting nearly flawless adherence to APA format.
- Write with a specific purpose with your patient in mind.
- Adhere to scholarly and disciplinary writing standards and current APA formatting requirements.
Additional Requirements
Before submitting your assessment, proofread your preliminary care coordination plan and community resources list to minimize errors that could distract readers and make it more difficult for them to focus on the substance of your plan. Be sure to submit both documents.
READ MORE >>
