Our Previous Samples
BSN-FP4002 Interdisciplinary CommunicationImagine you are part of an interdiscip ...
BSN-FP4002 Interdisciplinary Communication
Imagine you are part of an interdisciplinary healthcare team in your organization. Although the team has been working together for several months, communication between members is not always efficient or effective, and the situation has become stressful for everyone. The team leader asks you to develop a presentation for the team that addresses the issue.
PREPARATION
Search the Capella library and the Internet for scholarly and professional peer-reviewed articles on communication. You will need at least three articles to use as support for your work on this assessment.
DIRECTIONS
Create a 6–8-slide PowerPoint presentation to examine the communication issue and the risk it creates for positive health care outcomes.
- Describe the types of communication barriers that occur within an interdisciplinary team.
- Explain how the communication barriers can impact patient safety and health care outcomes.
- Recommend specific evidence-based strategies to improve communication within the team.
- Explain how the strategies will benefit team members and patients.
Use the notes section of each slide to expand your points and cite your supporting evidence. Also, include a title slide and a reference slide that lists the resources you used in this assessment.
ADDITIONAL REQUIREMENTS
- Use APA format for citations and references.
- Be creative. Consider your intended audience.
SUGGESTED RESOURCES
The following optional resources are provided to support you in completing the assessment or to provide a helpful context. For additional resources, refer to the Research Resources and Supplemental Resources in the left navigation menu of your courseroom.
Capella Resources
- APA Paper Template.
- APA Paper Tutorial.
Capella Multimedia
Click the links provided below to view the following multimedia pieces:
- Possible Barriers to Communication | Transcript.
SHOW LESS
Library Resources
The following e-books or articles from the Capella University Library are linked directly in this course:
- Brown, J., Lewis, L., Ellis, K., Stewart, M., Freeman, T., & Kasperski, M. J. (2011). Conflict on interprofessional primary health care teams – can it be resolved?Journal of Interprofessional Care, 25(1), 4–10.
- Gilardi, S., Guglielmetti, C., & Pravettoni, G. (2014). Interprofessional team dynamics and information flow management in emergency departments. Journal of Advanced Nursing, 70(6), 1299–1309.
- Garon, M. (2012). Speaking up, being heard: Registered nurses’ perceptions of workplace communication. Journal of Nursing Management, 20(3), 361–371.
- Wagner, J., Liston, B., & Miller, J. (2011). Developing interprofessional communication skills. Teaching and Learning in Nursing, 6, 97–101.
- Boykins, A. D. (2014). Core communication competencies in patient-centered care. ABNF Journal, 25(2), 40–45.
- Groves, W. (2014). Professional practice skills for nurses. Nursing Standard, 29(1), 51–59.
- Frederick, D. (2014). Bullying, mentoring, and patient care. AORN Journal, 99(5), 587–593.
- Ndoro, S. (2014). Effective multidisciplinary working: The key to high-quality care. British Journal of Nursing, 23(13), 724–727.
Course Library Guide
A Capella University library guide has been created specifically for your use in this course. You are encouraged to refer to the resources in the BSN-FP4002 – Assessment, Communication, and Collaboration Library Guide to help direct your research.
Internet Resources
Access the following resources by clicking the links provided. Please note that URLs change frequently. Permissions for the following links have either been granted or deemed appropriate for educational use at the time of course publication.
- Proper Patient Care – Team Communication | Transcript.
- Interprofessional Team | Transcript.
- Transforming Conflict to Collaboration in Healthcare | Transcript.
- Interdisciplinary Team Care: Case 1 | Transcript.
Bookstore Resources
The resources listed below are relevant to the topics and assessments in this course and are not required. Unless noted otherwise, these materials are available for purchase from the Capella University Bookstore. When searching the bookstore, be sure to look for the Course ID with the specific –FP (FlexPath) course designation.
- Clark, C. C., & Paraska, K. K. (2014). Health promotion for nurses: A practical guide. Burlington, MA: Jones & Bartlett.
- Chapter 3.
Scoring Guide
attachment
READ MORE >>
BSN-FP4012 Assessment 4OverviewWrite a 3-4 page analysis that assesses your prof ...
BSN-FP4012 Assessment 4
Overview
Write a 3-4 page analysis that assesses your professional development needs as a nurse leader.
Note: The assessments in this course build upon each other, so you are strongly encouraged to complete them in sequence.
For professional nurse-leaders, effective communication skills are essential for interprofessional teamwork and collaboration. Kelly and Tazbir (2014) emphasize the importance of this interaction:
Interprofessional teamwork and collaboration among staff nurses and other disciplines in the health care setting are so critical to optimizing patient care safety and outcomes that they are a priority for most health care administrators, directors, and managers (p. 140).
Successful leadership strategies are based on a leader’s strengths, the situation, the environment, and the stakeholders involved. Developing a plan for professional development is integral in developing leadership and management skills.
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
Competency 1: Integrate key nursing leadership, management, and communication concepts into collaborative practice situations.
Differentiate between leadership and management.
Explain key nursing leadership, management, and communication concepts that facilitate collaboration and support interprofessional teams.
Describe a personal leadership and communication style.
Identify skills or areas for future professional development.
Competency 5: Communicate in manner that is consistent with the expectations of a nursing professional.
Write content clearly and logically, with correct use of grammar, punctuation, and mechanics.
Correctly format citations and references using current APA style.
Reference
Kelly, P., &Tazbir, J. (2014). Essentials of nursing leadership and management (3rd ed.). Clifton Park, NY: Delmar.
Context
Throughout its history, nursing has relied on ethical principles to serve as guidelines in determining patient care (Kelly &Tazbir, 2014, p. 395). Health care leaders have the responsibility to create an ethically principled environment that upholds the professional standards. According to Kelly and Tazbir (2014), “Ethics is the branch of philosophy that concerns the distinction of right from wrong, based on a body of knowledge, not just based on opinions” (p. 395).
Reference
Kelly, P., &Tazbir, J. (2014). Essentials of nursing leadership and management (3rd ed.). Clifton Park, NY: Delmar.
Questions to Consider
To deepen your understanding, you are encouraged to consider the questions below and discuss them with a fellow learner, a work associate, an interested friend, or a member of your professional community.
What are some effective strategies for communicating and resolving conflict?
What are some of the communication challenges when working with interprofessional teams?
How does the leadership style and behavior affect an organization’s culture?
What are the attributes of an effective nurse leader?
Also Read:
- Discussion 4: Safety concerns for APRN providers
- Assignment 11: Barriers to nurses’ participation
- NUR 513 Week 6 Quiz Assignment
- Topic 3 DQ2 Patophysiology Week 2
- NUR 550 Topic 2: Epidemiology, Biostatistics, Genetics, and Genomics
- NUR 550 Topic 3 Translational Research Framework and Legal and Ethical Considerations
Resources
Suggested Resources
The following optional resources are provided to support you in completing each assessment. They provide helpful information about the topics in this unit. For additional resources, refer to the Research Resources and Supplemental Resources in the left navigation menu of your courseroom.
Capella Multimedia
Click the links provided below to view the following multimedia pieces:
Nurse Leadership: Present and Future Needs | Transcript.
Leadership Styles Questionnaire | Transcript.
Leadership Skills Questionnaire | Transcript.
Leadership Perception Questionnaire | Transcript.
Library Resources
The following resources are provided for you in the Capella University Library and are linked directly in this course. These articles contain content relevant to the topics and assessments that are the focus of this unit.
Giltinane, C. L. (2013). Leadership styles and theories. Nursing Standard, 27(41), 35–39.
Martin, D., Godfrey, N., & Walker, M. (2015). The baccalaureate big 5: What Magnet hospitals should expect from a baccalaureate generalist nurse. Journal of Nursing Administration, 45(3), 121–123.
Doroteo-Espinosa, M. M. (2013, February). Management strategies and leadership styles of selected hospitals for effective clinical nursing supervision. Paper presented at the International Conference on Management, Leadership & Governance, Kidmore End, UK.
Dickerson, P. S. (2014). Grounding our practice in nursing professional development. Journal of Continuing Education in Nursing, 45(7), 288–289.
Park, C. W. (2015). Interprofessional education: Implications for nursing professional development practice. Journal for Nurses in Professional Development, 31(4), 242–243.
Hauck, S., Winsett, R. P., &Kuric, J. (2013). Leadership facilitation strategies to establish evidence-based practice in an acute care hospital. Journal of Advanced Nursing, 69(3), 664–674.
Course Library Guide
A Capella University library guide has been created specifically for your use in this course. You are encouraged to refer to the resources in the BSN-FP4012 – Nursing Leadership and Management Library Guide to help direct your research
Internet Resources
Access the following resources by clicking the links provided. Please note that URLs change frequently. Permissions for the following links have been either granted or deemed appropriate for educational use at the time of course publication.
Nurse Manager Skill Inventor (2006). Retrieved from http://www.aacn.org/wd/practice/docs/nurse-manager-inventory-tool.pdf?menu=practice
Newline Ideas. (n.d.). Communication style self-assessment. Retrieved from http://www.newlineideas.com/communication-style-quiz.html
Free Management Library. (n.d.). Various self-assessments for personal and professional development. Retrieved from http://managementhelp.org/personaldevelopment/self-assessments.htm
Leadership IQ. (n.d.). Quiz: What’s your leadership style? Retrieved from http://www.leadershipiq.com/blogs/leadershipiq/36533569-quiz-whats-your-leadership-style
Situational Leadership Style Summary/Self Assessment. (n.d.). Retrieved from http://www.consumerstar.org/resources/pdf/Situational-Leadership-Self-Assessment.pdf
Psychology Today. (n.d.). Leadership style test. Retrieved from http://psychologytoday.tests.psychtests.com/take_test.php?idRegTest=3205
Learning Nurse. (n.d.). Nursing competence advanced self-assessment tools. Retrieved from http://www.learningnurse.org/index.php/assessment/sa-tools/sa-advanced
American Association of Colleges of Nursing. (2011). Core competencies for interprofessional collaborative practice. Retrieved from http://www.aacn.nche.edu/education-resources/IPECReport.pdf
READ MORE >>
BSN-FP4010 Capella Organizational Evaluation Health Care Concerns ReportDevelop ...
BSN-FP4010 Capella Organizational Evaluation Health Care Concerns Report
Develop a 3–5-page report that explains how an organization serves the health care concerns and needs of a population. The report should identify gaps in the health care service, explain strategies to bridge the gaps, and describe potential barriers to those strategies.
Note: The assessments in this course build upon each other. You are strongly encouraged to complete them in sequence. By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
- Competency 1: Explain the principles and concepts of disease prevention and health promotion for diverse and vulnerable populations.
- Identify barriers to implementing evidence-based strategies to bridge gaps in the health care service provided by an organization to a vulnerable or diverse population.
- Competency 2: Develop evidence-based health promotion and disease prevention initiatives for diverse and vulnerable populations.
- Identify gaps in the health care service provided by an organization to a vulnerable or diverse population.
- Explain evidence-based strategies to bridge gaps in the health care service provided by an organization to a vulnerable or diverse population.
- Competency 3: Apply basic epidemiological concepts, data analysis methods, tools, and databases to determine the effectiveness of health promotion and disease prevention initiatives for diverse and vulnerable populations.
- Explain how a health care organization serves the primary health care concerns of a vulnerable or diverse population.
- Competency 5: Communicate in a manner that is scholarly, professional, and consistent with expectations for members of the health care professions.
- Write content clearly and logically, with correct use of grammar, punctuation, APA formatting, and mechanics.
Competency Map
Check Your Progress Use this online tool to track your performance and progress through your course.
Also read: BSN-FP4010 Organizational Evaluation health Care Concerns Report Capella
Context
Pérez and Luquis (2014) stated, “Integrating cultural proficiency practices into the individual practices of health educators and public health organizational policies is a call to action” (p. 50). It is important for those in health care to be aware of the methods used to identify and evaluate the specific health care needs of individuals, communities, and populations, and to understand the meaning of health literacy as it pertains to the needs of a multicultural population or group.
With a growing diverse population, the incorporation of cultural and linguistic competence should be included into the planning, implementation, and evaluation of health education and promotion programs. “In this process, it is essential to employ theoretical models that describe and explain culture and related concepts (Pérez & Luquis, 2014, p. 165). Cultural constructs need to be applied to all health education, promotion, and prevention interventions targeting diverse communities (Pérez & Luquis, 2014).
Reference
Pérez, M. A., & Luquis, R. R. (2014). Cultural competence in health education and health promotion (2nd ed.). San Francisco, CA: Jossey-Bass.
Questions to Consider
To deepen your understanding, you are encouraged to consider the questions below and discuss them with a fellow learner, a work associate, an interested friend, or a member of the business community.
What factors are most likely to affect health promotion and wellness for vulnerable and diverse populations?
How would you assess your own cultural competence?
Resources
SUGGESTED RESOURCES
The following optional resources are provided to support you in completing the assessment or to provide a helpful context. For additional resources, refer to the Research Resources and Supplemental Resources in the left navigation menu of your courseroom.
Capella Multimedia
Click the link provided below to view the following multimedia piece:
- Assessment Models in Public Health | Transcript.
Library Resources
The following e-books or articles from the Capella University Library are linked directly in this course:
- Gertner, E. J., Sabino, J. N., Mahady, E., Deitrick, L. M., Patton, J. R., Grim, M. K., … Salas-Lopez, D. (2010). Developing a culturally competent health network: A planning framework and guide. Journal of Healthcare Management, 55(3), 190–204.
- Soulé, I. (2014). Cultural competence in health care: An emerging theory. Advances in Nursing Science, 37(1), 48–60.
- Somerville, M. H., Seeff, L., Hale, D., & O’Brien, D. J. (2015). Hospitals, collaboration, and community health improvement. Journal of Law, Medicine & Ethics, 43(1), 56–59.
- McClimens, A., Brewster, J., & Lewis, R. (2014). Recognising and respecting patients’ cultural diversity. Nursing Standard, 28(28), 45–52.
- Henderson, S., Kendall, E., & See, L. (2011). The effectiveness of culturally appropriate interventions to manage or prevent chronic disease in culturally and linguistically diverse communities: A systematic literature review. Health and Social Care in the Community, 19(3), 225–249.
- Truong, M., Paradies, Y., & Priest, N. (2014). Interventions to improve cultural competency in healthcare: A systematic review of reviews. BMC Health Services Research, 14(1), 1–31.
- Dovidio, J. F., & Fiske, S. T. (2012). Under the radar: How unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. American Journal of Public Health, 102(5), 945–952.
Course Library Guide
A Capella University library guide has been created specifically for your use in this course. You are encouraged to refer to the resources in the BSN-FP4010 – Health Promotion and Disease Prevention in Vulnerable and Diverse Populations Library Guide to help direct your research.
Internet Resources
Access the following resource by clicking the link provided. Please note that URLs change frequently. Permissions for the following link has either been granted or deemed appropriate for educational use at the time of course publication.
- U.S. Department of Health and Human Services, Office of Minority Health. (n.d.). The National CLAS Standards. Retrieved from http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=…
Bookstore Resources
The resource listed below is relevant to the topics and assessments in this course and is not required. Unless noted otherwise, this resource is available from the Capella University Bookstore. When searching the bookstore, be sure to look for the Course ID with the specific –FP (FlexPath) course designation.
Pérez, M. A., & Luquis, R. R. (Eds.). (2014). Cultural competence in health education and health promotion (2nd ed.). San Francisco, CA: Jossey-Bass.
Chapters 4 and 6.
Assessment Instructions
PREPARATION
Now that your team has a better understanding of the population served by the organization, you need to evaluate how able the organization is to serve the specific health care needs of the population identified in the Windshield Survey assessment.
- Use the Internet and the Capella library to locate at least three academic or professional resources to use in this assessment.
- Follow the same formatting instructions that you used in the Windshield Survey assessment. Your assessment should be done as a report for your team, using APA formatting for in-text citations and references.
REQUIREMENTS
In your organizational evaluation, complete the following:
- Describe the primary health concern for a vulnerable or diverse population.
- Explain how the organization currently serves this health care concern. Be sure you include information on how the organization communicates to the population.
- Identify gaps in the health care service provided to the population.
- Explain evidence-based strategies to bridge the gaps in health care service provided to the population.
- Identify any possible barriers to implementing your strategies.
ADDITIONAL REQUIREMENTS
Include a title page and reference page. The completed assessment should be 3–5 pages in length, not including the title page and reference page.
Reference at least three current scholarly or professional resources.
Use current APA format for citations and references.
Use Times New Roman font, 12 point.
Double space.
BSN-FP4010 Assessment 4 Professional Development
Assessment Instructions
Preparation
Your organization has seen an increase in the number of individuals using CAM, traditional medicine, holistic health, and spirituality. In addition to your work on the interdisciplinary team, you have been asked by your organization to prepare and deliver an educational session on CAM, traditional medicine, holistic health, and spirituality that can be used by all health care teams. How will you complete this task?
You should focus on these concepts as they pertain to your population (from the Windshield Survey assessment), but also in a broader sense. Use the Capella library and the Internet to look for recent research articles or information on these topics to use as supporting resources in your assessment.
Requirements
For this assessment, prepare a PowerPoint presentation in which you:
- Identify the topics you will cover in your educational plan.
- Provide a list of resources your audience can use to further their understanding of CAM.
- Explain why it is important for nurses and members of other health care teams to develop an understanding of CAM, traditional medicine, holistic health, and spirituality.
- Examine any ethical, legal, and economic principles related to CAM, traditional medicine, holistic health, and spirituality.
- Describe how these forms of health care can affect a plan of action for individuals and populations.
Your presentation should include a slide with the title of your educational session, a slide with the topics that will be covered (your agenda), and a reference slide at the end. Use the notes section of each slide to provide additional information on each topic, along with supporting references. References and in-text citations must adhere to APA guidelines.
Additional Requirements
- Include a title slide and reference slide. The completed assessment should be 8–10 slides in length, not including the title slide and reference slide.
- Reference at least three current scholarly or professional resources.
- Use current APA format for references.
- Be creative!
- Overview
Prepare a PowerPoint presentation of 8–10 slides that explains why an understanding of CAM and spirituality is important for members of health care teams; examines the ethical, legal, and financial principles related to CAM and spirituality; and describes how these forms of health care can impact plans of action.
Note: The assessments in this course build upon each other, so you are strongly encouraged to complete them in sequence.
As a leader in the field of nursing, it is important for you to identify areas within your organization that may need to improve cultural competence, and to develop educational materials to assist in doing so.
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
- Competency 1: Explain the principles and concepts of disease prevention and health promotion for diverse and vulnerable populations.
- Describe how CAM, traditional medicine, holistic health, and spirituality can affect a plan of action for individuals and populations.
- Competency 2: Develop evidence-based health promotion and disease prevention initiatives for diverse and vulnerable populations.
- Identify topics for an organizational education plan on CAM and spirituality.
- Explain the importance of health care professionals developing an understanding of CAM, traditional medicine, holistic health, and spirituality.
- Competency 3: Apply basic epidemiological concepts, data analysis methods, tools, and databases to determine the effectiveness of health promotion and disease prevention initiatives for diverse and vulnerable populations.
- Provide a list of resources to include in an organizational education plan on CAM and spirituality.
- Competency 4: Examine the ethical, legal, and economic factors related to health disparities in diverse and vulnerable populations.
- Examine ethical, legal, and economic principles related to CAM, traditional medicine, holistic health, and spirituality.
- Competency 5: Communicate in a manner that is scholarly, professional, and consistent with expectations for members of the health care professions.
- Write content clearly and logically, with correct use of grammar, punctuation, and mechanics.
- Correctly format citations and references using APA style.
Professional Development Scoring Guide
- Questions to Consider
To deepen your understanding, you are encouraged to consider the questions below and discuss them with a fellow learner, a work associate, an interested friend, or a member of the business community.
- What types of CAM, traditional medicine, holistic healing, or spirituality have you observed in your nursing practice?
- How do these practices affect the health and wellness of the individuals who practice them? How do the practices affect your ability to provide health care to individuals who practice them?
READ MORE >>
BSN-FP4012 Heart Failure Clinic Resourcing Plan 5Write a 3–4 page evidence-bas ...
BSN-FP4012 Heart Failure Clinic Resourcing Plan 5
Write a 3–4 page evidence-based resourcing plan for one component of the Heart Failure Clinic.
It is important for the nurse leader to have not only a basic understanding of the budget process, but to understand how to work with variances in staffing, patient loads, and supply costs in order to meet the needs of the patients, without compromising the funding process of the clinic.
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
• Competency 3: Apply management strategies and best practices for health care finance, human resources, and materials allocation decisions to improve health care delivery and patient outcomes.
o Apply evidence-based management strategies and best practices for resourcing health care services.
o Describe management and accountability tools and procedures used to manage health delivery services and patient outcomes.
Competency 4: Apply professional standards of moral, ethical, and legal conduct in professional practice.
o Apply legal and professional standards for resourcing outpatient services.
Competency 5: Communicate in manner that is consistent with the expectations of a nursing professional.
o Write content clearly and logically, with correct use of grammar, punctuation, and mechanics.
o Correctly format citations and references using current APA style.
ORDER THROUGH BOUTESSAY
Reference
Kelly, P., & Tazbir, J. (2014). Essentials of nursing leadership and management (3rd ed.). Clifton Park, NY: Delmar.
Context
Health care delivery is a complex process and system that includes multiple delivery sites such as hospitals, ambulatory care centers, private-provider offices, community-health facilities, home-care agencies, and extended-care facilities. Managed care is a method used to reimburse or pay for health care service. It includes more than just payment; it also controls the delivery services. Health care reform has been undertaken for a variety of reasons, not the least of which are access and health disparities issues. Nursing within an organization is a critical component of health care delivery and is an essential ingredient in patient outcomes (Kelly & Tazbir, 2014).
Questions to Consider
To deepen your understanding, you are encouraged to consider the questions below and discuss them with a fellow learner, a work associate, an interested friend, or a member of your professional community.
For the following questions, you may wish to review the Brown, Bornstein, and Wilcox article “Partnership and Empowerment Program: A Model for Patient-Centered, Comprehensive, and Cost-Effective Care,” listed in the Unit Resources.
Who makes you accountable for the delegation that you use in your organization, as well as on a state and national level?
Are there ways you could initiate greater collaboration with the health care team by using delegation?
What is the purpose of the National Council of State Boards of Nursing delegation decision-making tree?
What is the long-term implication related to health care cost if the patient or patient population continues to have poor outcomes related to cost containment?
How can you address cost within your organization, as a nursing leader, and how is this related to patient outcomes?
Resources
Suggested Resources
The following optional resources are provided to support you in completing each assessment. They provide helpful information about the topics in this unit. For additional resources, refer to the Research Resources and Supplemental Resources in the left navigation menu of your courseroom.
Library Resources
The following resources are provided for you in the Capella University Library and are linked directly in this course. These articles contain content relevant to the topics and assessments that are the focus of this unit.
Brown, C., Bornstein, E., & Wilcox, C. (2012). Partnership and empowerment program: A model for patient-centered, comprehensive, and cost-effective care. Clinical Journal of Oncology Nursing, 16(1), 15–17.
Rundio, A. (2012). The nurse manager’s guide to budgeting & finance. Indianapolis, IN: Sigma Theta Tau International.
Cranmer, P., & Nhemachena, J. (2013). Ethics for nurses: Theory and practice. Maidenhead, Berkshire, UK: Open University Press.
Pynes, J. E., Lombardi, D. N. (2011). Human resources management for health care organizations: A strategic approach. San Francisco: Jossey-Bass.
Simons, T., Leroy, H., Savage, G. T. (2013). Leading in health care organizations: Improving safety, satisfaction, and financial performance. Bingley, UK: Emerald Group.
Zelman, W. N., McCue, M. J., Glick, N. D., Thomas, M. S. (2014). Financial management of health care organizations: An introduction to fundamental tools, concepts, and applications (4th ed.). San Francisco: Jossey-Bass.
Mensik, N. (2013). What nurses need to know about nurse staffing today | Transcript. Retrieved from https://www.youtube.com/watch?v=mo5OFmGQQH0
American Nurses Association (ANA). (2015). Code of ethics for nurses. Retrieved from http://www.nursingworld.org/MainMenuCategories/EthicsStandards/CodeofEthicsforNurses.aspx
National Council of State Boards of Nursing (NCSBN). (n.d.). Retrieved from https://www.ncsbn.org/index.htm
Joint Commission. (2015, January 12). Hospital outpatient department. Retrieved from http://www.jointcommission.org/hospital_outpatient_department
American Nurses Association (ANA). (n.d.). Scope of practice. Retrieved from www.nursingworld.org/EspeciallyForYou/AdvancedPracticeNurses/Scope-of-Practice-2
Kelly, P., & Tazbir, J. (2014). Essentials of nursing leadership and management (3rd ed.). Clifton Park, NY: Delmar.
o Chapters 8–10
o Chapters 14–15.
Assessment Instructions
Preparation
Refer to the Capella library and the Internet for supplemental resources to help you complete this assessment.
Instructions
Deliverable: Develop one component of an evidence-based resourcing plan.
READ MORE >>
Building Healthy Communities Sample DiscussionIntroduction.Community assessment ...
Building Healthy Communities Sample Discussion
Introduction.
Community assessment can be defined as the process of identifying the strengths, assets, needs and challenges of a specific community. Community assessment is categorized into community surveys, key informant interviews, focus groups and community forums (Wu, 2019). The whole community assessment process entails various components. It is critical to organize and plan adequately. This is followed by community engagement, development of a goal or a vision, conducting the assessment while prioritizing health issues. Development of a community health improvement plan followed by evaluation of the whole process and results are also key steps.
A community assessment provides key stakeholders with comprehensive information and data regarding the community’s health status, needs, requirements and issues. This information is critical in the development of a community health improvement plan as it guides the allocation of funds and other resources that are vital in meeting community health needs (Jones et al., 2018). The reason I am conducting this community assessment is to understand the impact of depression among teens and adolescents and to enable the formulation of programs and interventions aimed at addressing the issues. This essay involves assessment of the community to determine the impact of social determinants on the overall health of the community.
Impact of Social Determinants on Health.
Social determinants of health can be termed as the environmental conditions where an individual is born, lives, works and thrives that greatly impact the individual’s health and overall well-being. Social determinants of health can be broadly classified into five major domains. These include economic stability, access and quality of education, access and quality of health care, the immediate neighbourhood and social and community context (Palmer et al., 2019).
Social determinants of health greatly affect an individual’s health, overall well-being and quality of life. Social determinants greatly contribute to differences and inequities in health care. Simply promoting healthy lifestyle choices will not do much in addressing health disparities. Public health organizations are therefore, tasked with the responsibility of improving the general conditions of people’s environments (Donkin et al., 2017). Healthy people 2030 aims at the creation of an environment that promotes the attainment of the full potential for health and well-being for each and every individual.
Health Problem Under Investigation.
Depression, also termed as major depressive disorder is a mood disorder that is normally characterized by a constant feeling of sadness and or lack of interest in life and activities that were previously pleasurable. Depression manifests as feelings of sadness, hopelessness, outbursts of anger, irritability, sleep disorders and loss of interest in previously stimulating activities (Malhi & Mann, 2018). Depression in adolescents and teenagers has mostly been attributed to factors that negatively impact self-esteem and self-acceptance such as obesity, bullying, physical and sexual assault and academic woes.
Depression in teenagers is a serious condition that has far reaching consequences and requires long-term management and treatment. Apart from the normal expected emotional changes, depression in teenagers also manifests with behavioral changes (Miller & Campo, 2021). Drug and alcohol use, appetite changes, social isolation, thoughts of self-harm and suicide are some of the behavioral changes observed. Physical illness can also result in depression and it is therefore important to seek medical help as soon as the symptoms manifest.
Information Gathered on the Topic.
Depression is particularly high in adolescents and teenagers aged twelve to seventeen years. Prevalence of depression was higher in adolescents from low-income backgrounds as compared to their counterparts from high-income families. Children who had experienced traumatic childhood experiences also tended to report a higher prevalence of depression. The centre for disease control and prevention estimated that about 3.2% of children aged three years to seventeen suffer from depression (Lu, 2019). This rate was particularly higher in teens as compared to young children. In Florida, research done between 2013 and 2014 showed that about 146,000 adolescents, translating to approximately 10.5% of all adolescents, experienced at least one episode of depression within the year.
Community Under Investigation.
Boundaries.
Pahokee is a city that is located on the shore of Lake Okeechobee in Palm Beach County, Florida, United States. The city’s geographical coordinates are 26 degrees 49’11” North, 80 degrees 39’ 56” West
Environment.
The environment within Pahokee can be described as a harsh environment. The city comprises majorly of African Americans who are mostly a low-income community. Each and every year, residents of Pahokee experience what is termed as the fall of “black snow”. This is as a result of the burning of sugar cane fields that is common before harvesting. This resultant pollution greatly affects a majority of the population and has been attributed with asthma, respiratory illnesses and other immune system illnesses within the community. The sugar industry also causes major pollution of the local water sources (Yoder et al., 2020), including Lake Okeechobee, resulting in decreased access to clean water, affecting marine life and lowering the value of property in Pahokee. Other environmentally friendly methods of sugar harvesting have been suggested but the prominent sugar company remains adamant. This has resulted in increased levels of childhood asthma, COPD, cancer and other ailments as a result of the continued pollution.
Size.
The city of Pahokee occupies an estimated area of 5.32 square miles (13.77 square kilometres).
Climate.
Pahokee, Florida averages approximately 51 inches of rain each year. This is higher than the United States’ annual average which stands at 38 inches of rainfall each year. The region averages zero inches of snow annually with the nation averaging 28 inches of snow per year. There are approximately 239 sunny days experienced each year in Pahokee (Palm & Bolsen, 2020). This is higher than the national average which stands at 205 days. Pahokee experiences around 110 days of precipitation on average annually. The highest temperature is experienced in July and is around 92 degrees with lows of approximately 52 degrees being experienced in January.
History.
The city of Pahokee was initially known as East Beach and later Ridgeway Beach with Pahokee being adopted from the Seminole name for the Everglades, Pay-ha-o-kee, which means grassy waters. Much of Pahokee was initially owned by the State of Florida or the Southern States Land and Timber Company (Henry et al., 2021). The two often allowed farmers to work the fields without requiring purchase or rent payments. In 1915, a celery grower named B.A. Howard purchased about 400 acres and set up Pahokee Realty Company with the aim of selling the land in parcels.
In 1917, a frost destroyed crops throughout majority of Florida. A high ridge located in what is today downtown Pahokee shielded majority of the farms from the elements. News that vegetable fields in Pahokee had survived the frost coupled with the opening of the West Palm Beach Canal in the same year resulted to migration of many farmers into Pahokee. The Pahokee Drainage District was set up in 1922 and the City of Pahokee incorporated that same year. By the year 1930, the city of Pahokee had an estimated two thousand residents and it greatly thrived throughout the 1930s.
Population.
The city of Pahokee had a population of 6,327 people in 2020. It is the 209th largest city in Florida and the 4198th largest in the United States. The annual population growth rate is 0.09 percent with an increase of 12 percent in population from the most recent population census conducted in 2010 where the population was 5,649. The population density is approximately 1,190 people per square mile (Melix et al., 2020). The poverty rate is 37.82% with an average household income of $39,519. Majority of the people residing in Pahokee are African Americans accounting for about 62.63% of the total population. Whites comprise about 30.52% of the total population with other races making up 6.40% of the total population.
Population Under Investigation.
Size.
Data available showed that approximately 13% of the total population lies between the ages of 5 and 13 years. This is about eight hundred individuals. Most of these people meet the criteria for out investigation of depression among teenagers and adolescents.
Density.
The approximate population density of adolescents and teenagers is 160 people per square mile.
Demographic structure.
About 9% of the population is five years and below. Our target population aged between 5 and 17 makes up about 13% of the population. Residents aged 75 years and above make up slightly above 4% of the total population (Melix et al., 2020). A study conducted in 2018 showed that the average age of all residents of Pahokee was 35 years.
Observations.
Boundaries.
Pahokee is a city situated on the shore of Lake Okeechobee in Palm Beach County, Florida, United States. It is located at latitude 26 degrees 49’17.39” N and longitude -80 degrees 39’20.99” W.
Housing and Zoning.
Pahokee Housing Authority, Inc. Comprises of five Public Housing Developments. These include Fremd Village, McClure Village, McClure Annex, Padgett Island, Isles of Pahokee II. These properties are governed by the Department of Housing and Urban Development (HUD’s) rules and regulations (Allison, 2020). The main goal is to maintain a safe and healthy living environment for families and children residing in Pahokee.
Open Space.
Pahokee State Park is one of the open spaces available in the city of Pahokee and is situated near Belle Glade, Clewiston and Loxahatchee.
Commons.
The commons in Pahokee include Florida State Road 729, Pahokee High School and St. Mary’s Catholic Church.
Transportation.
Approximately 80% of the residents are vehicle drivers with majority choosing to drive alone. The busiest time on the roads is between 7:00am and 7:30am. Driving cars, vans and trucks was the commonest mode of transport that was used by about one 1300 residents. About 50 residents walked with about 22 opting to use other means of transportation.
Social Service Centres.
The Pahokee Center located at 170 S. Barfield Highway, Suite 101 provides various service including pediatric services, adult primary care, behavioral health, infectious disease among other services. It has several trained professionals who provide the necessary services. The centre can be reached via telephone at any time of the day or night.
Stores.
There are several stores in and around Pahokee that provide the necessary daily commodities at fairly affordable prices.
Animals.
There are several adoption shelters for animals in the city of Pahokee. Several organizations also provide animal control services for animals including iguanas, armadillos, squirrels, raccoons among others.
Condition of the Area.
93% of all individuals are from low-income families. Pahokee is a neighbourhood that has high incidences of crime. The region is also prone to frequent hurricanes which pose a threat to the local community.
Religion.
About 37.2% of the residents of Pahokee are religious individuals. Majority of the individuals are Catholics accounting for about 16.6% of all religious people. Various other denominations are represented in Pahokee with a small number of Muslims also present.
Health Indicators.
There are 254 physicians for every 100,000 residents in Pahokee. This is higher than the current national average which is about 210 physicians per 100,000 people. The annual health cost index stands at 96.3, lower than the national average of 100. The annual water quality index is 30, again below the US average of 55.
Politics.
Pahokee is a somewhat a liberal society. During the most recent presidential election, approximately 56% of the eligible voters voted Democrats while 43.3% voted for the Republican Party. 0.8% voted independently (Rich, 2019). This trend where Democrats gather more votes has been observed since they year 2000.
Media.
There are several media outlets within the city of Pahokee. Some of the major outlets include Talk 4 Media, FaceDown Media Magazine, CRD Media among others.
Business and Industry.
Unemployment in the city of Pahokee exceeds 25%. The major sugar plant that had been established in 1963 was closed in 2009. There are several other small business and establishments owned by the local community.
Overall Impression of the Community.
The constant exposure to pollution from what is termed as “black snow” from burning of the sugar cane fields greatly undermines the overall health of the residents of Pahokee. Despite other netter alternatives, responsible companies have insisted with continuous burning is what is now termed as economic racism. This has resulted in increased occurrence of respiratory illnesses such as asthma, COPD and other illness such as cancer and diseases affecting the overall immune system.
Poverty and unemployment are also rampant in the city of Pahokee. Employment rates exceed 25% with majority of the population being low income families. Such factors greatly bring about disparities in health care. Low literacy levels among the individuals also greatly impact the overall health of the community. Statistics show that about 36% of students achieved proficiency in reading and language arts which is lower than the Florida state average of 56%. They further contribute to disparities in seeking health care and other health related services.
Strengths and Weaknesses of the Community.
One of the strengths is the availability of Pahokee Center which provides various social services. The centre provides pediatric services, adult primary care, behavioral health, infectious disease, laboratory, care management and other services. The centre has several licensed practitioners and health care workers tasked with the responsibility of providing services to the community. This contributes to improved health care services among the residents of Pahokee.
Lack of clean water resulting from pollution of the local water sources greatly undermines the overall health of the community. Low income, high unemployment rates and high illiteracy levels also greatly undermine the overall health care seeking culture. These factors greatly undermine the overall health of the residents of Pahokee by predisposing them to diseases while also limiting health care seeking services.
Well-being of the Population.
About 46% of the residents of Pahokee report that they consume a healthy diet. Most of the residents consume at least three meals each day, most of which are prepared in fast food joints and grocery stores. 44% of the residents are obese with approximately 55% reporting that they were obese at one particular point in time (Kirk Wiese et al., 2018). A certain percentage of the population has at one point experimented with drugs such as marijuana, cocaine and other hard drugs. 11% of the population have been informed by a health professional that they have diabetes with 3% of the population currently on insulin. 30% of the population especially those above 18 years and older have been diagnosed with depression or feelings of hopelessness.
Safety of the Community.
The crime rate in Pahokee is 41.60 per 1000 residents on average each year. The northwest part of the city seems to be relatively safer when compared to other parts of the city. In the south neighbourhoods, the probability of becoming a victim of crime is about 1 in 16 (Lewis & Rodesiler, 2020). This is much lower in the northwest part of the city where the probability is 1 in 35. Violent crime incidence rate is 54.4 which is almost double the national average of 22.7. Pahokee property crime rate stands at 42.6. This is also higher than the United States average of 35.4. Other crimes witnessed in this region include rape, burglary, theft, motor vehicle theft, rape and murder. The city is also a high hurricane risk area.
Social Determinants Affecting Health.
High crime rates observed in the city of Pahokee greatly impact the mental health of teenagers and adolescents. People who are victims of violent crimes such as physical and sexual assault tend to have lower mental health and well-being (Smith et al., 2021). Observing and being victims of such crimes greatly impairs the self-esteem of individuals consequently affecting their mental health. Traumatic events such as the loss of loved ones to violent crimes may also trigger depression that has far reaching consequences.
Low income levels are also associated with several mental disorders and attempts of self-harm and suicide. Low income resulting from factors such as unemployment greatly contributes to stressors such as insecurity in food, housing and income. These stressors consequently trigger mental health complications such as depression and may exacerbate the use of drugs and other substances (Roddy et al., 2020). Stressors can also contribute to neglect from parents and guardians which also greatly impacts the mental health of both teenagers and adolescents.
Low literacy levels also greatly contribute to mental health deterioration and conditions such as depression. Illiteracy greatly hinders access to education, knowledge and other services aimed at mental health improvement (Clark et al., 2020). Inability to read and write also leads to lowered self-esteem and withdrawal from participation in social events. This lowered sense of self-esteem and isolation triggers mental health conditions such as depression which is particularly rampant in teenagers and adolescents.
Conclusion.
Social determinants greatly affect an individual’s general health and overall well-being (Magnan, 2017). Depression is a common condition witnessed among teenagers and adolescents. The condition is triggered by several factors and presents mostly with a feeling of hopelessness and loss of interest in life. A research of the city of Pahokee identified several inequities such as low literacy levels, unemployment and low income and high crime rates. These factors greatly affect the general well-being of the residents of Pahokee and can be directly attributed to the causation of mental health problems observed among teenagers and adolescents
References
- Allison, J. (2020). Greening inequality: How urban sustainable development fails under neoliberalism. https://doi.org/10.15760/honors.977
- Clark, L. H., Hudson, J. L., Rapee, R. M., & Grasby, K. L. (2020). Investigating the impact of masculinity on the relationship between anxiety specific mental health literacy and mental health help-seeking in adolescent males. Journal of Anxiety Disorders, 76, 102292. https://doi.org/10.1016/j.janxdis.2020.102292
- Donkin, A., Goldblatt, P., Allen, J., Nathanson, V., & Marmot, M. (2017). Global action on the Social Determinants of Health. BMJ Global Health, 3(Suppl 1). https://doi.org/10.1136/bmjgh-2017-000603
- Henry, T. J., White, C. E., & Halbert, S. E. (2021). New Florida and United States Heteropteran Records (Hemiptera: Aradidae, Coreidae, Miridae). Proceedings of the Entomological Society of Washington, 123(3). https://doi.org/10.4289/0013-8797.123.3.538
- Jones, R. B., Zhu, X., Moan, E., Murff, H. J., Ness, R. M., Seidner, D. L., Sun, S., Yu, C., Dai, Q., Fodor, A. A., Azcarate-Peril, M. A., & Shrubsole, M. J. (2018). Inter-niche and inter-individual variation in gut microbial community assessment using stool, rectal swab, and mucosal samples. Scientific Reports, 8(1). https://doi.org/10.1038/s41598-018-22408-4
- Kirk Wiese, L., Galvin, J. E., & Williams, C. L. (2018). Rural stakeholder perceptions about cognitive screening. Aging & Mental Health, 23(12), 1616–1628. https://doi.org/10.1080/13607863.2018.1525607
- LEWIS, M. A. R. K., & RODESILER, L. U. K. E. (2020). Special issue: Sports-related young adult literature. Study and Scrutiny: Research on Young Adult Literature, 4(2), i-ix. https://doi.org/10.15763/issn.2376-5275.2020.4.2.i-ix
- Lu, W. (2019). Adolescent depression: National trends, risk factors, and healthcare disparities. American Journal of Health Behavior, 43(1), 181–194. https://doi.org/10.5993/ajhb.43.1.15
- Magnan, S. (2017). Social Determinants of Health 101 for health care: Five plus five. NAM Perspectives, 7(10). https://doi.org/10.31478/201710c
- Malhi, G. S., & Mann, J. J. (2018). Depression. The Lancet, 392(10161), 2299–2312. https://doi.org/10.1016/s0140-6736(18)31948-2
- Melix, B. L., Uejio, C. K., Kintziger, K. W., Reid, K., Duclos, C., Jordan, M. M., Holmes, T., & Joiner, J. (2020). Florida neighborhood analysis of Social Determinants and their relationship to life expectancy. BMC Public Health, 20(1). https://doi.org/10.1186/s12889-020-08754-x
- Miller, L., & Campo, J. V. (2021). Depression in adolescents. New England Journal of Medicine, 385(5), 445–449. https://doi.org/10.1056/nejmra2033475
- Palm, R., & Bolsen, T. (2020). The science of climate change and sea-level rise. Coastal Research Library, 5–13. https://doi.org/10.1007/978-3-030-32602-9_2
- Palmer, R. C., Ismond, D., Rodriquez, E. J., & Kaufman, J. S. (2019). Social Determinants of Health: Future Directions for Health Disparities Research. American Journal of Public Health, 109(S1). https://doi.org/10.2105/ajph.2019.304964
- Rich, B. R. (2019). Sundance 2019: Infiltrating the scene. Film Quarterly, 72(4), 87–92. https://doi.org/10.1525/fq.2019.72.4.87
- Roddy, M. K. K., Rhoades, G. K., & Doss, B. D. (2020). Effects of eprep and ourrelationship on low-income couples’ mental health and Health Behaviors: A randomized controlled trial. Prevention Science, 21(6), 861–871. https://doi.org/10.1007/s11121-020-01100-y
- Smith, S., Ferguson, C. J., Askew, R., Pitts, J., & Hinderleider, A. (2021). Gun ownership, poverty, and Mental Health Associations with crime: A cross-state comparison. Criminology & Criminal Justice, 174889582110604. https://doi.org/10.1177/17488958211060473
- Wu, V. C.-S. (2019). The geography and disparities of Community Philanthropy: A community assessment model of needs, resources, and ecological environment. VOLUNTAS: International Journal of Voluntary and Nonprofit Organizations, 32(2), 351–371. https://doi.org/10.1007/s11266-019-00180-x
- Yoder, L., Chowdhury, R. R., & Hauck, C. (2020). Watershed Restoration in the florida everglades: Agricultural Water Management and long-term trends in nutrient outcomes in the everglades agricultural area. Agriculture, Ecosystems & Environment, 302, 107070. https://doi.org/10.1016/j.agee.2020.10707
READ MORE >>
Building Leadership Capacity Discussion NR703Building Leadership Capacity Discus ...
Building Leadership Capacity Discussion NR703
Building Leadership Capacity Discussion NR703
NR703 Week 1 Building Leadership Capacity
Discussion
Purpose
The purpose of this discussion is to examine your leadership skills, determine your leadership gaps, explore developmental opportunities, and differentiate between a leader’s strengths and a manager’s skills.
Instructions
Reflect on your personal and professional experience using the lessons in Week 1, your NR703 Self-Reflection: Performance Behaviors of Transformational Leaders, and the Strengths-to-Strategy Plan results. Address the following:
- Describe and give examples of your two strongest leadership competencies and two most significant leadership gaps, weakness, or developmental opportunities. (1 paragraph)
- Describe and explain how your leadership strengths differ from management skills or behaviors. (1 paragraph)
- Describe how you will integrate emotional intelligence into your leadership identity and how this may impact the characteristics of your followers. (1 paragraph)
Construct your responses using the CARE Plan method.
Please click on the following link to review the DNP Discussion Guidelines on the Student Resource Center program page:
- Link (webpage): DNP Discussion GuidelinesLinks to an external site.
Program Competencies
This discussion enables the student to meet the following program competences:
- Applies organizational and system leadership skills to affect systemic changes in corporate culture and to promote continuous improvement in clinical outcomes. (PO 6)
- Appraises current information systems and technologies to improve health care. (POs 6, 7)
- Creates a supportive organizational culture for flourishing collaborative teams to facilitate clinical disease prevention and promote population health at all system levels. (PO 8)
Also Read:
NR703 Week 2 Transformative Leader Presence Discussion
Organizational Needs Assessment NR703
Course Outcomes
This discussion enables the student to meet the following course outcomes:
- Compare and contrast theories of organizational behavior and leadership. (PCs 2, 4; PO 6)
- Differentiate attributes of effective leaders and followers in influencing healthcare. (PCs 2, 4; PO 6)
- Formulate selected strategies for leadership and influence across healthcare systems. (PC 6; PO 8)
Due Dates
- Initial Post: By 11:59 p.m. MT on Wednesday
- Follow-Up Posts: By 11:59 p.m. MT on Sunday
Sample Building Leadership Capacity Discussion NR703 Student AT
Mar 8, 2023Mar 8 at 6:39pm
According to Squazzo (2019), an effective leader is defined as someone with effective communication, strong relationship-building skills, adaptability, innovation, and accountability. My two strongest leadership competencies include adaptability and effective communication. An example of effective communication as a nurse practitioner working in the hospital or critical care setting is the ability to coordinate care across a multidisciplinary team of healthcare professionals.
Each of these professionals has their own role and responsibilities, and in order to work effectively with different team members, one may need to adjust a communication style in order to better collaborate with a team member (Marshall and Broome, 2021). My two biggest areas to develop as a leader include lack of focus and taking on too many tasks when leading a team.
An example of taking on too many tasks can include managing too large of a caseload while also taking on administrative tasks or completing paperwork. This in turn can lead to a lack of focus, burn-out, and reduced job satisfaction. Sometimes I find myself saying “yes” to too many tasks and spreading myself too thin to do an effective job at the tasks.
Leadership and management are often used interchangeably, but they are distinct concepts. According to Lush (2021), management is about planning, organizing, coordinating, and controlling resources to achieve specific objectives, while leadership is about influencing people to follow a vision, inspiring them to give their best, and creating an environment that enables them to achieve their full potential. While both management and leadership are important for the success of an organization, they require different skills and behaviors.
Management is more focused on the operational aspects of an organization, while leadership is more about inspiring and motivating people toward a common goal (Lush, 2021). As a leader, this focus is more on inspiring and motivating people toward a common goal, while a manager focuses on planning, organizing, and controlling resources to achieve specific objectives (Lush, 2021). Both skills are necessary for the success of an organization, and a good leader should also have strong management skills and vice versa
Integrating emotional intelligence (EI) into leadership identity involves developing self-awareness, empathy, and self-regulation (Goleman, 1998; Maqbool et al., 2017). Leaders who have a high degree of emotional intelligence are better able to understand their own emotions and those of others, communicate effectively, manage conflict, and build strong relationships (Goleman, 1998; Maqbool et al., 2017).
Maqbool et al. (2017) found that emotional intelligence, along with project managers’ competencies and transformational leadership, significantly impacted project success. Emotional intelligence was found to be positively associated with project success, suggesting that leaders who possess high levels of EI are more likely to lead successful projects (Goleman, 1998; Maqbool et al., 2017).
References
Goleman, D. (1998). Working with emotional intelligence. Bantam Books.
Marshall, E. S., & Broome, M. E. (2021). Frameworks for becoming a transformational leader. In M. E. Broome & E. S. Marshall (Eds.), Transformational leadership in nursing: From expert clinician to influential leader (3rd ed). Springer Publishing Company.
Lush, M. (2021). The leadership versus management debate: What’s the difference? The Institute of Management New Zealand. https://www.imnz.co.nz/the-leadership-versus-management-debate
Maqbool, R., Ye, S., Manzoor, N., & Rashid, Y. (2017). The impact of emotional intelligence, project managers’ competencies, and transformational leadership on project success: An empirical perspective. Project Management Journal, 48(3), 58-75. https://doi.org/10.1177/875697281704800304
Squazzo, J. D. (2020). Defining moment for leadership: How CEOs are leading successfully. Healthcare Executive, 35(6), 20-22.
NR703 WEEK 1 Building Leadership Capacity Discussion Resources
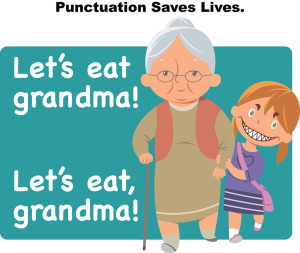
Punctuation Image Description
Watch the following video for a tutorial on Grammarly:
- Link (video): How to Use Grammarly – Beginner’s GuideLinks to an external site.(10:37)
The APA Basics section of the Writing Center contains several resources such as APA paper templates and guidelines.
- Link (webpage): APA BasicsLinks to an external site.
Week 1 References
- Baumgardner, A. (2017, May 11). Collaborative artistic leadership: 3 tips on leveraging strengths to enhance the power of your team.Astrid Baumgardner Coaching & Training. https://www.astridbaumgardner.com/blog-and-resources/blog/collaborative-artistic-leadership-3-tips-on-leveraging-strengths-to-enhance-the-power-of-your-team/
- Broome, M. E., & Marshall, E. S. (Eds.). (2021). Transformational leadership in nursing: From expert clinician to influential leader(3rd ed). Springer Publishing Company. https://doi.org/10.1891/9780826135056
- Goleman, D. (1998). Working with emotional intelligence. Bantam Books.
- Marshall, E. S., & Broome, M. E. (2021). Frameworks for becoming a transformational leader. In M. E. Broome & E. S. Marshall (Eds.), Transformational leadership in nursing: From expert clinician to influential leader(3rd ed). Springer Publishing Company.
- Lush, M. (2021). The leadership versus management debate: What’s the difference? The Institute of Management New Zealand. https://www.imnz.co.nz/the-leadership-versus-management-debate
- Maqbool, R., Ye, S., Manzoor, N., & Rashid, Y. (2017). The impact of emotional intelligence, project managers’ competencies, and transformational leadership on project success: An empirical perspective. Project Management Journal, 48(3), 58-75. https://doi.org/10.1177/875697281704800304
- Sharma, S., & Sharma, S. (2019). Self-assessment for image building. IUP Journal of Soft Skills, 13(2), 49-54
- Toor, S., & Ofori, G. (2008). Leadership versus management: How they are different, and why. Leadership and Management in Engineering, 8(2), 61-71. https://doi.org/10.1061/(ASCE)1532-6748(2008)8:2(61)
Lesson 1 Assessing Leadership Strengths
Assessing Leadership Strengths
There are several?leadership assessments, tools, and reflection methods available to help you reflect on your skills, abilities, and talents in leadership. Many?also focus?on management skills, and some reveal personality characteristics.
Assessing your leadership strengths is an important first step to discovering your leadership gaps and developing a plan to bridge those gaps. One area of distinction to make is that management skills and leadership strengths differ in focus. However, both are incorporated in transformational leadership roles from the executive suite to the bedside. A transformational leader cultivates leadership behaviors and management practices to create a role that transforms people and environments.
The following table shows how leadership strengths and management skills combine to create transformational leadership.
Management Skills, Leadership Strengths, & Transformational Leadership
Leadership StrengthsManagement SkillsTransformational LeadershipDrives innovationDrives policySupports but validates policy using evidence and creative innovationGuides, influences, motivatesOrganizes, schedulesStrategically guidesMotivates, coaches, trustsPlans, budgets, evaluatesEmpowers teams to performDevelops intuition and insightDevelops analytic abilitiesDevelops analytical insightMay not have developed management skillsMay not have developed leadership strengthsDevelops both management skills and leadership strengthsPower from leadership strengthsPower from position and authorityPower from influenceEnablesOrdersGuidesDevelops personal agencyDevelops organizational agencyCreates positive agency for both the team and the organizationEthic of Care personaEthic of Justice personaBalances the Ethics of Justice and Care in one leadership personalityCare-basedRules-basedChange-basedVision-focusedResource-focusedOutcome-focusedInternal locus of controlExternal locus of controlInformed internal locus of controlSituational awarenessPolicy awarenessEmotional intelligenceNow, stop for a moment and consider the leadership strengths you have just examined. Think also about the skillset of a manager. Although both leadership and management strengths and skills tend to cross over in transformational leadership, alone they do define distinct characteristics worth consideration.
NR703 Self-Reflection: Performance Behaviors of Transformational Leaders
The NR703 Self-Reflection: Performance Behaviors of Transformational Leaders helps you define your transformational leadership strengths and talents. Through this reflection, you can better develop effectiveness as a leader.
Click on the following link and reflect on this representative list of leader and manager performance behaviors while thinking about the Strengths-to-Strategy interactive that follows in the next section of this lesson. You can use this reflection to evaluate your overall leadership effectiveness. Then, focus on just the leadership strengths that you feel are your strongest and weakest for the Strengths-to-Strategy Interactive.
- Link (Word doc): NR703 Self-Reflection: Performance Behaviors of Transformational LeadersLinks to an external site.
NR703: Week 1 | Self-Reflection
Self-Reflection: Performance Behaviors of Transformational Leaders
Strength Category & Performance Behaviors
Leading Strengths
Creates a Behavioral Vision
- Behaviors reflect vision
- Generates an image of healthy team integration
- Inspires personal goal achievement
- Creates a desirable image for the future
Imagines innovations
- Courage to experiment
- Takes calculated risks to change
- Accepts suggestions for new ideas
- Drives innovation & synthesis of ideas
Empowers People
- Trusts others to act
- Encourages individuals to take action
- Builds confidence
- Creates a collaborative culture
- Reacts with situational awareness
Demonstrates Personal Ethics/Morals
- Operates with caring (Leadership Ethic of Care)
- Known for personal integrity
- Does the right things when no one is watching
- Does the right thing even if directed otherwise
- Respects and values people
- Exercises self-awareness & self-management (emotional intelligence)
Builds Relationships
- Demonstrates relationship behaviors
- Exercises social awareness & management (emotional intelligence)
- Delivers honest but constructive communication
- Embraces diversity & connects people
- Reaches out to make connections
- Adapts with Positivity
Influences Others
- Launches events into action
- Exhibits calmness in change
- Inspires allegiance
- Motivates commitment
- Direction is future-focused
Managing Skills
Represents Organizational Vision
- Uses positive vision language
- Interprets the vision of the future for each individual
- Projects the big picture
- Promotes organizational goal achievement
Demonstrates the Workplace Standards
- Drives organizational policy
- Makes policy and procedure
- Understands the business
- Has professional (technical) expertise
Creates Organization
- Organizes, schedules, orders, strategizes
- Plans, budgets, evaluates (employee management tasks)
- Directs work routines
- Adapts to change through complexity & resolves chaos
- Achieves strategic and operational goals
Demonstrates Organizational Ethics
- Operates with fairness (Leadership Ethic of Justice)
- Enforces regulations and rules fairly
- Acts on organizational values over personal values
- Creates a positive organizational culture
Communicates to Create Best Outcomes
- Challenges the status quo
- Engages evidence-based practice
- Translates science to bridge practice gaps
- Collaborates with interprofessional efficiency
- Embraces & encourages change
Enables
- Delegates authority
- Authorizes decision-making
- Empowers problem-solving
- Promotes individual development
Rewards
- Gives honest complements
- Avoids empty praise
- Acknowledges efforts
- Gives public acclaim appropriately
After completing the reflection, consider your findings as you watch this video clip.
Reflect on Your Leadership Strengths (0:50)
The practical results of any leadership reflection are discovered when you apply them to those you lead. Therefore, self-reflection should focus on how best to use those results to modify your own leadership personality and behaviors. Throughout this course, you will have the opportunity to reflect on yourself as a leader in relation to different leadership topics and concepts. So, keep your mind open to change. Use the results from your NR703 Self-Reflection: Performance Behaviors of Transformational Leaders to reflect on your personal Johari window (Sharma & Sharma, 2019).
Johari Window Interactive Transcript
When you leave this course, we hope you will find that you have matured as a leader, regardless of your current role, through self-reflection and explorations—keep an open mind and be ready to change as you explore your leadership “windows”!
Leveraging Strengths as a Practice Scholar
One of the strengths of leadership is the ability to leverage skills and talents—both in yourself and in others. By developing your own Strengths-to-Strategy plan, you can better assess where strengths can be applied to compensate for areas that require development. The same dynamic can be applied to those for whom the leader manages.
Leaders also leverage the strengths of others and their teams. Astrid Baumgardner (2017) is a successful career coach who offers three tips to leverage the strengths of the team to achieve the best outcomes:
- Know the strengths of your team members
- Have a strengths conversation at the outset of your project
- Allocate roles based on the strengths of your teammates (para. 8)
By knowing your strengths as a leader and the leadership strengths of your team, you can create your leadership Strengths-to-Strategy plan by identifying the following:
- Your leadership strengths
- Areas of opportunities for growth, improvement, and development in leadership (i.e., leadership gaps/shortcomings/weaknesses)
- Strategies to turn these opportunities into strengths
- Strategies for leveraging the strengths of others
An important Strengths-to-Strategy plan uses your strengths to leverage others’ strengths to provide a full complement of skills. Likewise, leveraging others’ strengths through delegation can often strengthen your own leadership gaps. As a leader, you may use this tool to create a Strengths-to-Strategy plan to support professional formation in others that you lead.
READ MORE >>
As online learning expands dramatically across primary, secondary, and higher ed ...
As online learning expands dramatically across primary, secondary, and higher education, crucial questions arise surrounding assessment integrity when exams occur remotely under unsupervised home conditions. Can learning management systems like Canvas actively monitor potential cheating behaviors like switching open browser tabs when students take crucial tests? What oversight functionalities exist natively or through integrated proctoring tools to ensure fair evaluations?
Let’s analyze how tab toggling on devices proves during remote quizzes.
What is Canvas?
Developed by Instructure, Canvas represents a trusted, user-friendly, cloud-based learning management system utilized by over 4,000 institutional clients globally. Core components include:
Canvas Catalog: Customizable course catalog enabling administration and tracking all academic offerings at an institution using a consolidated database.
Canvas Studio: Intuitive course development tool empowering instructors to build engaging video-based lessons through interactive slide layers.
Canva Commons: Shareable content repository allowing professors to import pre-made textbooks, assignments, rubrics, and other academic resources into personalized courses.
MasteryConnect: Competency-based assessment platform with embedded grading tools and differentiated assignment options for customized evaluations.
Dashboards: Consolidated real-time data analytics across individual users, courses, departments, and entire institutes for informed progress monitoring driving strategic decisions.
Can Canvas Track Tabs?
On its own, Canvas cannot detect or track browser tab switching during non-proctored quizzes and tests. The Canvas quiz log records events like answering questions, navigation within the quiz, and any time the student leaves or returns to the quiz page. However, it cannot identify specific external sites students visit when they switch tabs during a non-proctored exam.
How Does Canvas Detect Cheating?
Canvas partners with proctoring tools like Respondus Monitor, Proctorio, and Honorlock to enhance academic integrity. These use the student’s webcam and microphone to monitor their testing environment and restrict computing activities. This allows more comprehensive cheating detection, even during remote online tests. Tactics flagged by proctoring software include:
- Switching or opening new browser tabs
- Use of other devices like mobile phones
- Copy-pasting content from different sources
- Speaking with others during the test
- Screensharing and screenshots
Proctoring tools basically turn the student’s computer into a virtual exam proctor, restricting prohibited actions through a LockDown Browser while monitoring via webcam. Some capabilities include:
- Recording video, audio, and screen activity
- Disabling copy, paste, screenshots etc.
- Preventing new tabs and programs
- Monitoring all applications and websites accessed
- Flagging suspicious behaviors for review
Can Canvas Detect Copy-Paste?
Canvas itself does not detect copy-pasting content into quiz answers. However, it does integrate plagiarism checkers like Turnitin that compare student submissions against various databases to identify any copied or plagiarized work. However, simply paraphrasing content using tools like QuillBot can often bypass plagiarism detection in Canvas.
Proctoring software provides another layer of protection against copy-paste cheating during proctored online exams. By restricting access to other apps and the clipboard, students are blocked from easy copy-pasting. Any attempts to speak exam questions or responses out loud could also be detected via webcam monitoring.
Can Canvas Detect New Tabs?
On its own, Canvas cannot determine if a student opens new tabs or switches to other browser windows during a non-proctored quiz. Its monitoring capability is limited to logging navigation within the Canvas quiz itself. However, proctoring tools integrated with Canvas, like Respondus LockDown Browser, actively block students from launching new tabs or switching windows. The webcam enables the proctoring software to visually confirm the student’s focus remains on the Canvas quiz tab alone.
Can Canvas Detect Switching Tabs?
Similarly, Canvas does not natively detect tab switching during non-proctored quizzes. But with proctoring tools enabled, any attempts by students to switch tabs or browse unauthorized websites can be identified and prevented. Students are locked into the Canvas tab running the online test. Sites they try to access outside the quiz are blocked, and access attempts are flagged for review.
Can Canvas Detect Screen Sharing?
Without proctoring software, Canvas allows screen-sharing activities like mirroring the Canvas tab to another device. However, proctoring tools use webcam videos and screen recordings to observe the students’ monitor and environment throughout the online exam. Any secondary devices or attempts to broadcast the Canvas screen are detectable.
Can Canvas Detect Screenshots?
Canvas itself does not monitor or block students from taking screenshots of quiz questions or results. However, integrated proctoring tools like Respondus Monitor can utilize the webcam to visually confirm no secondary capturing devices are used. The LockDown Browser also prohibits accessing screenshot tools and blocks shortcut keys used for screenshots. Any screenshot attempt can be identified and flagged.
Can Canvas Detect Split Screen?
Similarly, without proctoring tools, Canvas cannot detect the use of split screens to display unauthorized information alongside the quiz tab. But proctoring software Leverages screen recording and webcam video to observe the student’s monitor and any attempts to split the display. Access to system controls for splitting screens is disabled through the LockDown Browser.
What Can Professors See On Canvas During Quizzes?
On its own, Canvas allows professors to see the quiz log with details like:
- When a student starts and completes the quiz
- How long they spent on each question
- When they navigated away from and back to the quiz page
For proctored exams, professors can review recordings of the student’s screen, webcam video, and audio throughout the test via integrated proctoring tools. This provides complete visibility into the testing environment and any behaviors like tab switching.
Clever Hacks to Cheat on Canvas Quizzes
While proctoring technology has enhanced Canvas quiz security, students still attempt cheating with tactics like:
- Using a separate device like a phone or notes placed strategically off-screen
- Enabling a virtual machine on their computer to sandbox the LockDown Browser
- Collaborating with other students through screen sharing or a group chat app
- Masking chat conversations as “speaking to oneself” out loud
- Paraphrasing copy-pasted content to evade plagiarism checkers
Using Canvas to Detect the Switching of Tabs
While Canvas itself cannot track student browser behaviors during non-proctored quizzes, proctoring integrations like Respondus Monitor provide comprehensive monitoring. Recording the on-screen activity, environment audio, webcam video, and restricting computing functions allows proctoring tools on Canvas to detect and deter prohibited actions like tab switching that could constitute cheating.
However, students continue attempting innovative workarounds. Ultimately, promoting academic integrity requires a combination of technology vigilance and fostering an ethical learning culture. With proper implementation, Canvas can detect cheating, and be part of a solid framework to uphold online exam integrity standards.
READ MORE >>
BUSINESS CASE FOR A NEW ECONOMIC OPPORTUNITY SAMPLEWhilborne Medical Center (WMC ...
BUSINESS CASE FOR A NEW ECONOMIC OPPORTUNITY SAMPLE
Whilborne Medical Center (WMC) is a multispecialty health care facility situated in proximity to an industrial park. Its management is planning to start a new economic initiative in the form of an urgent care center (UCC) within WMC’s premises. The UCC will not only help provide quality health care to the community but also provide an additional revenue stream for WMC. The objective of this business case is to present a detailed report on the feasibility and cost–benefit considerations of implementing the proposed economic initiative over the next five years. The business case includes an evaluation of various risks and opportunities associated with the new initiative. It recommends ways to lessen the risks associated with setting up the UCC and strategies for controlling costs and maximizing benefits.
Opportunities Associated With the Proposed Economic Initiative
An economic and environmental analysis was performed to determine the opportunities and risks associated with the UCC. WMC is situated near Maxima Industrial Park. Most of the patients treated at WMC are among the 30,000 workers from different companies in the industrial park. Additionally, the area has around 3,000 locals. The UCC may cater to the nonemergent needs of both the workers from the park and the locals in the area.
UCCs present an opportunity to reduce overcrowding in the ED at WMC. Often, EDs have to tend to patients whose cases are urgent, but do not merit the emergent care that EDs provide (Qin, Prybutok, Prybutok, & Wang, 2015). Non-emergent cases can be diverted to the UCC, where health care personnel will be able to treat workers of the industrial park who walk in with work-related injuries or for preventive care. Additionally, any urgent health care needs of the local community may be met by the UCC. The ED will be able to exclusively tend to the more emergent cases, while the UCC will exclusively tend to the urgent care cases received by WMC. Thus, an additional revenue stream for WMC will be created with the addition of the UCC.
Additionally, UCCs must serve a high number of patients to break even (Yee, Lechner, & Boukus, 2013). Therefore, location near a target patient population is an important factor in the success of a UCC (Gurganious & Greenfield, 2015). The required target population for the UCC is found in the 30,000 workers employed at Maxima Industrial Park. WMC has developed a relationship with workers from the park through the annual health checkups it organizes. The UCC can benefit from this relationship as there is a high likelihood that employees who are satisfied with the care they received at WMC will return to the UCC for urgent care issues.
A competitor analysis conducted in the area shows that there are two primary health clinics, but no UCCs in WMC’s vicinity. Most patients prefer primary health clinics over UCCs and EDs (Qin et al., 2015). This issue is mitigated by the number of work hours that EDs and UCCs have over primary health clinics. With the introduction of a UCC, patients will be able to avail after-hours health care for minor illnesses on any day of the week at lower costs compared to primary health clinics (Chang, Brundage, & Chokshi, 2015). Also, as patients can go to a UCC without an appointment (unlike a primary health clinic), they will find the UCC more accessible for treating minor illnesses (Yakobi, 2017). These advantages over its competitors will help WMC capture a significant market share in the urgent care segment.
Risks Associated With the Economic Initiative and Ways to Address Them
The potential risks associated with the setting up of a UCC were identified. It was observed during the competitor analysis that a retail health clinic inside a Walmart store situated near WMC could pose a threat to the UCC. Retail health clinics are walk-in clinics located inside grocery stores or supermarkets. They mainly provide convenient care to retail store customers suffering from minor illnesses. Like UCCs, many retail health clinics offer after-hours care and easy accessibility without an appointment; at the same time, the health care cost at these clinics is less than it is at UCCs (Chang et al., 2015). Therefore, the presence of the retail health clinic puts the financial security of the UCC at risk as it might appear more attractive to patients in need of urgent care.
A UCC is equipped to handle a wider number of ailments than a retail health clinic (Chang et al., 2015). Being affiliated with WMC, the UCC can provide its patients access to more facilities such as scans and tests that are not provided by retail health clinics and other UCCs. These factors set the UCC at WMC apart from its competitors and can be used to promote the clinic. Clients will consider the UCC a convenient and viable option for their healthcare, where multiple tests can be done if needed. Additionally, the UCC must also ensure that the focus of the clinic is on providing a convenient and satisfactory experience for the patient (Gurganious & Greenfield, 2015). If patients receive quick and timely care from excellent service providers, they will be encouraged to visit again and refer new patients to the UCC.
UCCs are known for providing immediate care to many patients in a relatively short time (Yakobi, 2017). The staff and management of the UCC will have to be aware that the highvolume, speedy health care delivery environment leaves room for errors such as misdiagnoses. These errors can result in the UCC and its staff facing serious legal risks. Therefore, it is important for the UCC to maintain meticulous documentation to insulate itself from the consequences of misdiagnoses or medical malpractice. The symptoms, physical observations, and lab results which are used to develop a plan to administer care should be identified to ensure that the plan has clarity and is logical (“Why good documentation matters”, 2016). It is also binding on UCC physicians to set patients’ expectations by communicating with them effectively about the nature of services provided (“Helping patients make informed decisions”, 2014). These measures ensure that, despite the difficulties resulting from high demand, both patients and health care practitioners are mindful of the treatment that is administered.
Cost–Benefit Analysis of the Proposed Economic Initiative
After considering the opportunities and risks involved, the costs and benefits of setting up a UCC are analyzed. To assess the economic feasibility of setting up a UCC, the present value of the estimated costs and benefits and the net benefit over a 5-year time horizon are calculated using a present value discount rate of 11%. The present value discount rate has been determined based on the standard cost of capital and the estimated target returns. The estimated capital cost includes minor construction costs and the cost of purchasing furniture and equipment.
These are conservatively projected to be $350,000 in the current year (Golinkin & Danielle, 2013). The estimated operating costs comprise expenditure on salaries paid to the staff; basic utilities such as electricity, gas, and the Internet; insurance (including insurance for staff, business liability, building, furniture, and equipment); and other operating expenses such as administrative and marketing costs.
On an average, most UCCs have two full-time (or part-time) physicians, two nurse practitioners, and three medical assistants or other clinical staff (Weinick, Bristol, & DesRoches, 2009). It is assumed that two physicians, two nurse practitioners, three medical assistants, and a medical receptionist will be recruited by the UCC. Based on the national average recruitment incentives, staff salaries (per annum) in the first year of operation are assumed to be around $232,000 for a full-time physician, $112,000 for a nurse practitioner, $35,000 for a medical assistant, and $32,000 for a receptionist (U.S. Bureau of Labor Statistics, 2017). The actual growth rate of an employee’s salary in the U.S. is 2.7% per annum (Economic Policy Institute, 2018). For this analysis, salaries of the employees of the UCC are assumed to increase at a conservative rate of 3% per annum. Additional costs will be incurred in years four and five to hire a full-time nurse practitioner (year four) and a full-time physician (year five) to cater to the increased number of patients.
The cost of basic utilities is assumed to increase by around 5% per annum, as utilization of basic utilities will increase owing to an increase in patient volume. Considering that new staff will be hired in the fourth and fifth years of operation, insurance costs are assumed to increase in these 2 years owing to addition of staff. Other operating costs are assumed to be around 12% of annual revenue based on WMC’s financial statements. As per the cost–benefit analysis, the present value of the total costs over the 5-year period is estimated at $5,489,745.62, using a present value discount rate of 11% (see Appendix for more information on cost–benefit analysis over a 5-year period).
Benefit (revenue) was calculated based on the fee collected from each patient and the number of patients expected to make use of the medical services at the UCC. Most clinics tend to the needs of an average of around 357 patients every week and charge an average fee of approximately $156 per patient visit (AMN Healthcare, 2015; Yakobi, 2017). Therefore, the estimated revenue earned during the first year of operations will be $2,730,000. It is also assumed that the revenue will increase by 5.3% per annum over the 5-year period based on the national average (“Urgent Care Center Market”, 2018). Based on the estimated revenue over the 5-year period and the 11% present value discount rate, the present value of total benefits is estimated at $11,037,800.03 (see Appendix for more information on cost–benefit analysis over a 5-year period). The net benefit, calculated by subtracting the present value of total benefits from the present value of total costs, is estimated at $5,548,054.41 over a 5-year period (see Appendix for more information on cost–benefit analysis over a 5-year period). Based on the positive net benefit, it can be concluded that this initiative will be an economically viable one.
It should be noted that, although the cost–benefit analysis suggests that setting up a UCC is a viable option, some knowledge gaps and unknowns are bound to be present. The impact of nonmonetary costs, such as the time and effort spent on marketing and ensuring a good patient experience, has not been considered in the analysis. Nonmonetary costs can have an effect on the patient volume and that, in turn, can affect the net benefit. An increase in capital and operating costs due to some unexpected developments or unforeseen expenses can affect the net benefit gained. The patient volume may also vary depending on unpredictable factors such as the health care market environment. All these factors can have a significant impact on the result of the cost–benefit analysis.
Ways to Control Costs and Maximize Benefits
It is essential for the senior management to regularly implement methods to control costs and monitor the financial position of the UCC. Overhead costs that are not directly related to providing health care services make up a large portion of the total costs of the UCC. Overhead costs include expenditure on building maintenance, repairs, insurance, basic utilities, and supplies. The UCC will keep a check on building maintenance costs by undertaking maintenance checks on a regular basis. To avoid significant repair costs, the staff will ensure that equipment is handled with care and maintained in good condition. By reviewing the usage of electricity, gas, water, phone, and the Internet on an annual basis, the UCC will also control basic utility expenses.
Low-cost plans, based on the UCC’s requirements, will be chosen to control expenses on phone and Internet services. To avoid wastage of supplies, the staff will be encouraged to use office supplies with discretion. Impractical cost control measures might adversely affect staff morale and performance. Therefore, care will be taken to ensure that all the measures undertaken are relevant, ethical, and culturally equitable.
Along with keeping a check on the costs, efforts will be made to maximize the benefits. A potential means of increasing the benefits of the UCC is sending automated health reminders to regular clients. This will help ensure a regular inflow of clients. Providing consistently good service to all patients will encourage them to come back to the UCC whenever they need immediate medical attention. This will also help build strong patient trust and loyalty. Also, understanding what motivates patients and their views about health care will help the UCC staff to customize care and thus increase patient satisfaction and inflow (Qin et al., 2017). Therefore, ensuring optimal utilization of resources and providing quality care will help the UCC maintain its financial stability.
Conclusion
The UCC will cater to the urgent care needs of the community by providing quick, affordable, and convenient health care services. The center’s proximity to the industrial area will benefit workers who might require urgent care or want to get preventive health checkups done as part of their employment requirements. Thus, the UCC will be able to generate an additional revenue stream and contribute to the economic growth of WMC. Moreover, the cost–benefit suggests that setting up the UCC will be an economically viable initiative. Ethical solutions such as careful documentation of the treatment process and full communication of the plan of care with the patient were recommended. These solutions, which reduce the risks associated with the setting up of the UCC, will also help safeguard the future of WMC.
References
AMN Healthcare. (2015). Convenient care: Growth and staffing trends in urgent care and retail medicine. Retrieved from https://amnhealthcare.com/uploadedFiles/MainSite/Content/Healthcare_Industry_Insights/Industry_Research/AMN%2015%20W001_Convenient%20Care%20Whitepaper(1).pdf
Chang, J. E., Brundage, S. C., & Chokshi, D. A. (2015). Convenient ambulatory care—Promise, pitfalls, and policy. The New England Journal of Medicine, 373(4), 382–388. Retrieved from http://library.capella.edu/login?qurl=https%3A%2F%2Fsearch.proquest.com%2Fdocvie w%2F1698429950%3Fac
Economic Policy Institute. (2018). Nominal wage tracker. Retrieved from https://epi.org/nominal-wage-tracker/
Golinkin, W. F., & Danielle, B. (2013). The dollars and cents of running a clinic. In J. Riff, S. Ryan, & T. Hansen-Turton (Eds.), Convenient care clinics: The essential guide to retail clinics for clinicians, managers, and educators (pp. 179–186). Retrieved from https://ebookcentral-proquestcom.library.capella.edu/lib/capella/detail.action?docID=1188973.
Gurganious, V., & Greenfield, D. (2015). Starting an urgent care center 5 essentials for success. Medical Economics, 92(11), 47–48. Retrieved from http://library.capella.edu/login?qurl=https%3A%2F%2Fsearch.proquest.com%2Fdocvie w%2F1696889732%3F
Helping patients make informed decisions. (2014, April). Retrieved from https://cmpaacpm.ca/en/advice-publications/browse-articles/2014/helping-patients-make-informeddecisions
Qin, H., Prybutok, G. L., Prybutok, V. R., & Wang, B. (2015). Quantitative comparisons of urgent care service providers. International Journal of Health Care Quality Assurance, 28(6), 574–594. Retrieved from http://library.capella.edu/login?qurl=https%3A%2F%2Fsearch.proquest.com%2Fdocvie w%2F1694933787%3Facco
Urgent Care Center Market by Service (Acute Illness Treatment, Trauma/Injury Treatment, Physical Examination, Immunization & Vaccination), Ownership (Corporate Owned,
Physician Owned, Hospital Owned), and Region – Global Forecast to 2023. (2018, March). Retrieved from https://marketsandmarkets.com/Market-Reports/urgent-carecenter-market-197843477.html
U.S. Bureau of Labor Statistics. (2017). Occupational employment statistics [Data set]. Retrieved from https://www.bls.gov/oes/current/naics4_621400.htm
Findings from a national survey. BMC Health Services Research, 9(79). http://dx.doi.org/10.1186/1472-6963-9-79
Why good documentation matters. (2016, October). Retrieved from https://cmpaacpm.ca/en/advice-publications/browse-articles/2011/why-good-documentation-matters
Yakobi, R. (2017). Impact of urgent care centers on emergency department visits. Health Care
Current Reviews, 5(3). http://dx.doi.org/10.4172/2375-4273.1000204
Yee, T., Lechner, A. E., & Boukus, E. R. (2013). The surge in urgent care centers: Emergency department alternative or costly convenience? Research Briefs. Retrieved from https://researchgate.net/profile/Tracy_Yee/publication/257202014_The_surge_in_urgent_care_centers_emergency_department_alternative_or_costly_convenience/links/5750682 008aed9fa2bd2d531
Appendix
Cost–Benefit Analysis Over a 5-Year Period
CostsCurrent Year (CY) ($)CY +1 ($)CY +2 ($)CY +3 ($)CY +4 ($)CY +5 ($)Total Costs ($)Capital Costs Construction350,000.00 Furniture & EquipmentOperating Costs Staff Salaries825,000.00849,750.00875,242.501,023,885.201,315,719.80 Basic Utilities55,000.0057,750.0060,637.5063,669.3866,852.84 Insurance15,000.0015,000.0015,000.0020,000.0025,000.00 Other Operating Costs327,600.00343,980.00361,179.00379,237.95398,199.85Total Costs (FutureValue)
350,000.001,222,600.001,266,480.001,312,059.001,486,792.521,805,772.49Total Costs (PresentValue)
350,000.001,101,441.441,027,903.58959,366.23979,396.291,071,638.085,489,745.62BenefitsCurrent Year (CY) ($)CY +1 ($)CY +2 ($)CY +3 ($)CY +4 ($)CY +5 ($)Total Costs ($)Increase in Revenue2,730,000.002,866,500.003,009,825.003,160,316.253,318,332.06Total Benefits (FutureValue)
2,730,000.002,866,500.003,009,825.003,160,316.253,318,332.06Total Benefits (PresentValue)
2,459,459.462,326,515.702,200,758.102,081,798.201,969,268.5711,037,800.03Present ValueDiscount Rate
0.11PV Denominator1.001.111.231.371.521.69Net Benefit5,548,054.41
READ MORE >>
Cannabis nursing, also known as cannabis therapeutics, is an emerging nurse spec ...
Cannabis nursing, also known as cannabis therapeutics, is an emerging nurse specialty that has grown alongside legislative changes and shifting public opinion regarding medical marijuana. Cannabis nurses primarily focus on educating patients and work in various settings, from wellness clinics to dispensaries. Their scope of practice is defined by the American Cannabis Nurses Association (ACNA) and aligns with evidence-based practice.
Two major nursing associations, the American Cannabis Nurses Association (ACNA) and the Cannabis Nurse Network (CNN), support this growing specialty. Let’s explore trends in cannabis therapy, the role of nursing in this field, and the potential of cannabis nursing as a career path.
Who Is a Cannabis Nurse?
The American Cannabis Nurses Association (ACNA) defines the scope and standards of cannabis nursing, which involves not only supporting and educating patients but also promoting wellness and healing through compassionate care that addresses patients’ needs. Cannabis nurses must possess knowledge and expertise beyond the standard registered nurse competencies.
This includes a deep understanding of the endocannabinoid system, cannabis therapeutics, cannabinoids, terpenoids, cannabis laboratory testing requirements, potential medication interactions, advocacy, ethics, and relevant laws.
Cannabis nurses also serve as advocates, coaches, and navigators, guiding patients through the vast landscape of cannabis information and misinformation. They strive to help patients achieve optimal homeostasis by supporting the endocannabinoid system. To maintain a professional and caring presence with patients, cannabis nurses must also prioritize self-care.
NCSBN Guidelines for Cannabis Nursing
The National Council of State Boards of Nursing (NCSBN) has established the Six Principles of Essential Knowledge, which outline the necessary information and skills nurses must possess when working with cannabis therapeutics:
- Comprehensive and current understanding of cannabis laws: Nurses must stay well-informed about the most recent cannabis legislation in the United States to ensure they practice within legal boundaries.
- Familiarity with local medical cannabis programs: Nurses should have a solid grasp of the medical cannabis programs available within their jurisdiction to guide better and support their patients.
- Thorough knowledge of the endocannabinoid system: A deep understanding of the endocannabinoid system is crucial for nurses to comprehend how cannabis interacts with the human body and its potential therapeutic effects.
- Expertise in cannabis pharmacology and research: Nurses must stay up-to-date with the latest research on cannabis treatments and have a strong foundation in cannabis pharmacology to make informed decisions and provide accurate information to patients.
- Awareness of safety considerations: Nurses should be well-versed in the potential risks and safety concerns associated with cannabis use to ensure patient well-being and minimize adverse effects.
- Unbiased approach to patient treatment choices: Nurses must maintain an open-minded and non-judgmental attitude regarding patients’ treatment decisions, respecting their autonomy and supporting them without prejudice.
What Does a Cannabis Nurse Do?
A cannabis nurse plays a vital role in educating, guiding, and supporting patients who use medical marijuana for various health conditions. Some of their key responsibilities include:
- Patient education: Cannabis nurses provide comprehensive information about the potential benefits, risks, and proper use of medical marijuana, helping patients make informed decisions about their treatment options.
- Dosage and administration guidance: They assist patients in determining the appropriate dosage, strain, and method of administration based on their individual needs and medical history.
- Monitoring and assessment: Cannabis nurses regularly monitor patients’ responses to treatment, assess the effectiveness of the medication, and watch for any potential side effects or adverse reactions.
- Collaboration with healthcare providers: They work closely with physicians, pharmacists, and other healthcare professionals to ensure a coordinated and comprehensive approach to patient care.
- Advocacy and support: Cannabis nurses act as advocates for their patients, helping them navigate the legal and social complexities surrounding medical marijuana use and providing emotional support throughout the treatment process.
- Staying current with research: They keep abreast of the latest research, developments, and best practices in cannabis therapeutics to provide their patients with the most up-to-date and evidence-based care.
- Maintaining professional standards: Cannabis nurses adhere to the scope and standards of practice set forth by professional organizations like the American Cannabis Nurses Association (ACNA) to ensure the highest quality of care and ethical conduct.
What are the Benefits of Being a Cannabis Nurse?
- High demand and job security: With the increasing legalization of medical marijuana and the ongoing nursing shortage in the USA, cannabis nurses are expected to be in high demand for the foreseeable future, ensuring excellent job prospects and security.
- Competitive compensation: As demand for cannabis nurses grows, so does the potential for attractive salaries, which are likely to increase further in the coming years.
- Opportunity to be part of a medical revolution: Cannabis nurses have the chance to participate in the exciting and rapidly evolving field of medical marijuana as more research unveils the therapeutic potential of cannabinoids like THC, CBD, CBG, and CBN in treating various medical conditions.
- Fulfilling work in helping patients: Nurses passionate about assisting others can find great satisfaction in working with patients who benefit from medical cannabis, as it is increasingly recognized as a breakthrough treatment for numerous ailments, including chronic pain, multiple sclerosis, fibromyalgia, and migraines.
- Engaging in a fascinating and growing industry: Whether you are a supporter, user, or simply curious about the applications and future of medical cannabis, being a cannabis nurse allows you to be at the forefront of this captivating and expanding industry.
How to Become a Cannabis Nurse
To become a cannabis nurse, you’ll need to follow these steps:
- Obtain a nursing degree: Earn an Associate Degree in Nursing (ADN) or a Bachelor of Science in Nursing (BSN) from an accredited nursing program.
- Pass the NCLEX-RN exam: After completing your nursing degree, you must pass the National Council Licensure Examination for Registered Nurses (NCLEX-RN) to obtain your nursing license.
- Gain experience: Work as a registered nurse to gain clinical experience and develop nursing skills.
- Pursue specialized education in cannabis therapeutics: Enroll in courses, workshops, or certificate programs focused on cannabis nursing offered by organizations such as the American Cannabis Nurses Association (ACNA) or educational institutions.
- Stay current with research and best practices: Continuously educate yourself about the latest research findings, legal developments, and best practices in cannabis therapeutics to provide the most up-to-date care to your patients.
- Consider cannabis nurse certification: Although not currently required, earning a certificate in cannabis nursing or science can demonstrate your expertise and commitment to the field.
- Network and engage with the cannabis nursing community: Join professional organizations like the ACNA or the Cannabis Nurse Network to access resources, attend conferences, and connect with other cannabis nurses.
- Seek job opportunities: Look for cannabis nursing positions in dispensaries, consulting practices, hospitals, clinics, research institutions, or educational settings that align with your career goals and interests.
Remember that the field of cannabis nursing is still evolving, and requirements may vary by state or employer. Staying informed about your area’s latest developments and regulations is essential for success in this growing specialty.
Where do Cannabis Nurses Work?
Cannabis nurses can work in various healthcare settings, providing direct patient care, conducting research, or offering clinical expertise in collaboration with product manufacturing companies.
In dispensaries, cannabis nurses assist patients by addressing unwanted or unintended consequences of cannabis products, such as side effects or concerns about habit formation. They help patients find the right cannabis strain and provide education on proper medication administration and dosing.
Cannabis nurses in consulting practices focus on educating patients about cannabis products, promoting safe cannabis use, and advising on the therapeutic effects of cannabis. They may also collaborate with product manufacturers in product development.
In hospitals or clinics, cannabis nurses inform patients about cannabis and its medical applications, provide support, and advocate for patients taking medical cannabis. They may also recruit patients for clinical trials and measure outcomes.
Regardless of the specific setting, cannabis nurses play a crucial role in educating and supporting patients, promoting safe and effective use of medical cannabis, and contributing to the growing body of knowledge in this emerging field.
Is there a certification for cannabis nurses?
Currently, there is no nationally recognized certification specifically for cannabis nurses. However, the ACNA offers a core curriculum for cannabis nursing, which provides a foundation for nurses interested in specializing in this field. Some universities and private organizations also offer certificate programs in cannabis science and therapeutics.
Cannabis Nursing Community
The cannabis nursing community is a growing network of healthcare professionals who are dedicated to advancing the field of cannabis therapeutics and supporting patients who use medical marijuana. Engaging with this community can provide numerous benefits for aspiring and practicing cannabis nurses.
Two prominent organizations in the cannabis nursing community are the American Cannabis Nurses Association (ACNA) and the Cannabis Nurse Network (CNN). These organizations offer a platform for nurses to connect, share knowledge, and access valuable resources.
The ACNA and CNN provide educational resources, including webinars, conferences, and workshops, to help nurses stay current with the latest research, best practices, and legal developments in cannabis therapeutics. Participating in these events can enhance your knowledge and skills while providing opportunities to network with other cannabis nurses.
Engaging with the cannabis nursing community allows you to connect with colleagues who share your interests and face similar challenges. These connections can lead to valuable friendships, mentorship opportunities, and professional collaborations.
As a member of the cannabis nursing community, you can contribute to the field’s growth and advancement by advocating for patient rights, participating in research, and taking on leadership roles within professional organizations.
Networking within the cannabis nursing community can open doors to new career opportunities, such as consulting, education, or research positions. Staying active and engaged in the community can help you stay informed about job openings and industry trends.
To get involved in the cannabis nursing community, consider joining the ACNA or CNN, attending conferences and workshops, participating in online forums and discussions, and connecting with other cannabis nurses through social media platforms like LinkedIn. By actively engaging with this community, you can contribute to the advancement of cannabis therapeutics while enhancing your own professional growth and career satisfaction.
Final Thoughts on How to Become a Dispensary Nurse
As the field of cannabis nursing continues to evolve, it’s crucial for nurses to stay informed about the latest developments in medical cannabis use, including frequently asked questions from patients and updates to the cannabis nurse’s scope of practice. With the growing acceptance and use of medical cannabis to treat various conditions, the demand for knowledgeable cannabis nurses is likely to increase, offering exciting career pathways for cannabis nurses interested in this specialty nursing practice.
READ MORE >>
Capella BSN-FP4006 Nursing and Workplace Violence ResearchA new initiative has b ...
Capella BSN-FP4006 Nursing and Workplace Violence Research
A new initiative has been introduced to educate nurses, health care workers, and social services workers on how to prevent workplace violence where you work. Write a 750–1,000-word article on workplace violence and prevention measures for the hospital employee newsletter. By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
Competency 1: Explain the effect of health care policies, legislation, and legal issues on health care delivery and patient outcomes.
- Identify the political, legal, and/or legislative factors that may contribute to violence in health care settings.
- Competency 2: Explain the effect of regulatory environments and controls on health care delivery and patient outcomes.
- Identify the main components of OSHA’s workplace violence prevention guidelines.
- Explain the American Nursing Association’s position on violence in the workplace.
- Explain safety policies and protocols for preventing and responding to violence against health care workers.
- Competency 4: Communicate in a manner that is consistent with expectations of nursing professionals.
- Write content clearly and logically, with correct use of grammar, punctuation, and mechanics.
- Correctly format citations and references using APA style.
Competency Map
Check Your Progress Use this online tool to track your performance and progress through your course.
Context
The Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health (NIOSH) (2002) defines workplace violence as any physical assault, threatening behavior, or verbal abuse occurring in the workplace. Violence includes overt and covert behaviors ranging in aggressiveness from verbal harassment to murder.
Specific to hospital workers, studies by the Institute for Occupational safety and Health (NIOSH) show that: Violence often takes place during times of high activity and interaction with patients, such as at meal times and during visiting hours and patient transportation. Assaults may occur when service is denied, when a patient is involuntarily admitted, or when a health care worker attempts to set limits on eating, drinking, or tobacco or alcohol use. (2002, para. 4)
Reference
Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. (2002). Violence: Occupational hazards in hospitals. Retrieved from http://www.cdc.gov/niosh/docs/2002-101
Questions to Consider
To deepen your understanding, you are encouraged to consider the questions below and discuss them with a fellow learner, a work associate, an interested friend, or a member of your professional community.
- What are the more common reasons for workplace violence?
- What clinical risk factors can lead to workplace violence?
- What obligation does a health care facility have to protect workers from violence?
- What personal safety strategies do you have to protect yourself from violence at work?
Resources
SUGGESTED RESOURCES
The following optional resources are provided to support you in completing the assessment or to provide a helpful context. For additional resources, refer to the Research Resources and Supplemental Resources in the left navigation menu of your courseroom.
Capella Resources
Click the links provided to view the following resources:
- APA Citation: Citing a Journal Article.
- APA Citation: Citing a Book.
- APA Citation: Citing a Website.
- APA Paper Template.
- APA Paper Tutorial.
Library Resources
The following e-books or articles from the Capella University Library are linked directly in this course:
- Doby, V. (2015). Leadership’s role in eliminating workplace violence and changing perceptions in the emergency department. Journal of Emergency Nursing, 41(1), 7.
- Blando, J., Ridenour, M., Hartley, D., & Casteel, C. (2015). Barriers to effective implementation of programs for the prevention of workplace violence in hospitals. Online Journal of Issues in Nursing, 20(1), 1–11.
- Bruce, M. D., & Nowlin, W. A. (2011). Workplace violence: Awareness, prevention, and response. Public Personnel Management, 40(4), 293–308.
- Saltzberg, C. W., & Clark, C. M. (2015). A bold call to action: Mobilizing nurses and employers to prevent and address incivility, bullying, and workplace violence. (2015). American Nurse Today, 10(8), 1.
- Gillespie, G. L., Gates, D. M., Miller, M., & Howard, P. K. (2010). Workplace violence in healthcare settings: Risk factors and protective strategies. Rehabilitation Nursing, 35(5), 177–184.
- Magnavita, N. (2014). Workplace violence and occupational stress in healthcare workers: A chicken-and-egg situation-results of a 6-year follow-up study. Journal of Nursing Scholarship, 46(5), 366–376.
- Speegle-Clark, K. (2013). Violence in the workplace: A prevention program for healthcare workers. (Doctoral dissertation). Available from ProQuest Dissertations and Theses database. (UMI No. 1539707).
- Papa, A., & Venella, J. (2013). Workplace violence in healthcare: Strategies for advocacy. Online Journal of Issues in Nursing, 18(1), 1.
Course Library Guide
A Capella University library guide has been created specifically for your use in this course. You are encouraged to refer to the resources in the BSN-FP4006 – Policy, Law, Ethics, and Regulations Library Guide to help direct your research.
Internet Resources
Access the following resources by clicking the links provided. Please note that URLs change frequently. Permissions for the following links have been either granted or deemed appropriate for educational use at the time of course publication.
- Professional Issues Panel on Incivility, Bullying, and Workplace Violence. (2015). Incivility, bullying, and workplace violence [Position paper]. Retrieved from https://www.nursingworld.org/~49d6e3/globalassets/…
- United States Department of Labor, Occupational Health & Safety Administration. (n.d.). Workplace violence. Retrieved from https://www.osha.gov/SLTC/healthcarefacilities/vio…
- United States Department of Labor, Occupational Health and Safety Administration. (n.d.). Workplace violence prevention – Health care and social service workers. Retrieved from https://www.osha.gov/dte/library/wp-violence/healt…
- AACN. (n.d.). Position statement: Workplace violence prevention. Retrieved from http://www.aacn.org/WD/Practice/Docs/Workplace_Vio…
- Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. (n.d.). Occupational violence. Retrieved from http://www.cdc.gov/niosh/topics/violence/training_…
- Liss, G. M. (2000). Violence in the health care workplace. CMAJ, 162(4). Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC123115…
Capella BSN-FP4006 Nursing and Workplace Violence Research Assessment Instructions
Your workplace has experienced some serious problems with workplace violence that occurred between patients and caregivers. A new initiative has been introduced to educate nurses, health care workers, and social services workers on how to prevent workplace violence. You have been asked to write an article on workplace violence and prevention measures for the hospital employee newsletter.
PREPARATION
Search the Capella library and the Internet for scholarly and professional peer-reviewed articles on workplace violence. You will need at least five articles to use as support for your work on this assessment.
DIRECTIONS
Write a 750–1,000-word article (3–4 pages) on workplace violence and prevention measures for the hospital employee newsletter. Address the following in your article:
- Identify the political, legal, and/or legislative factors that may contribute to violence in health care settings. Consider the types of patients that may be treated within a clinical or hospital setting.
- Compare OSHA regulations and the ANA position statement on workplace violence to organizational policies.
- Explain safety policies and protocols for preventing and responding to violence against health care workers.
ADDITIONAL REQUIREMENTS
Your presentation should meet the following requirements:
- Written communication: Written communication should be free of errors that detract from the overall message.
- References: Cite a minimum of five resources, with the majority being peer-reviewed sources. Your reference list should be appropriate to the body of literature available on this topic that has been published in the past 5 years.
- APA format: Resources and citations should be formatted according to current APA style and formatting.
- Length: 750– 1,000 words or 3–4 typed, double-spaced pages, excluding title page and reference page. Use Microsoft Word to complete the assessment.
- Font and font size: Times New Roman, 12-point.
READ MORE >>
