Our Previous Samples
NUR 621 Benchmark – Staffing Matrix And ReflectionNUR 621 Benchmark – Staffi ...
NUR 621 Benchmark – Staffing Matrix And Reflection
NUR 621 Benchmark – Staffing Matrix And Reflection
The purpose of this assignment is to prepare students to make staffing decisions based on sound financial management principles and compliance guidelines.
Scenario: You are the nurse leader of a 30-bed medical-surgical unit and have to account for all staffing, including any discrepancies Benchmark – Staffing Matrix And Reflection. Using sound financial management principles, complete the “NUR-621 Topic 8: Staffing Matrix” in the provided Excel template.
ORDER COMPREHENSIVE SOLUTION PAPERS ON Benchmark – Staffing Matrix And Reflection
After completing the matrix, compose a 1,000-1,250-word reflection answering the following questions:
- Why is it important to use a staffing matrix in your healthcare setting?
- Briefly describe your staffing matrix. How many FTEs (full-time equivalent) on the staffing roster are required to cover daily needs? What units of services or work measurement did you use and why? What financial management principles did you use to determine your staffing matrix?
- Explain how you adjusted your staffing based on changes in the patient census. Benchmark – Staffing Matrix And Reflection
- You receive your financial report for the month. You have used more FTEs than what was budgeted for your census. How will you make up the variance? How would you reallocate resources to make up for the variance and still comply with guidelines?
Include two to four peer-reviewed references in your essay, including the textbook.
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center. An abstract is not required.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
NUR-621 Topic 8: Staffing MatrixCensus30292827262524Direct CaregiversScheduled HoursShift LengthNumber of StaffDay ShiftRNNAHealth Unit CoordinatorNight ShiftRNNAHealth Unit CoordinatorAlso Read:HCA 459 Entire Course Discussion
Critically analyze some aspect of a personality theory
Module 1: The Keys to Persuasion
Assignment: Malingering and Addiction in the Treatment of Sleep Disorders
Discussion: Probability and Probability Distributions
Strategic Plan Recruiting and Supporting Teachers
Institutions rely heavily on strategic plans to adequately prepare and implement projects. Strategic plans can be used for organization-wide or department-wide decisions depending on the organizational needs. They have run vital activities such as budgeting, staffing, gathering resources, and organization expansion. Strategic plans are dynamic and change based on the needs and current circumstances requiring strategic plans. Staffing is one of the major activities in an organization because hiring the right staff determines the success of any institution, and support for new employees determines employees’ retention and integration into the institution. This paper develops a strategic plan to help a district school, Sunshine ISD in Houston, Texas, recruit and support new teachers.
Getting Ready for Success
Vigorous recruiting and supporting staff after recruitment improves their integration into the facility and eliminates error-making. The institution does not have a strong recruiting plan; thus, the recruiting and support process does not guarantee the best quality staff and staff support. Recruiting is a resource-intensive activity, but it is carried out once in a long time when the process is vigorous and the best staff are hired and retained (DeFeo & Tran, 2019).
The expected outcomes are creating a diversified and qualified staff team, ensuring staff is acquitted and comfortable in the facility, cultivating a moral school environment, and promoting the staff’s personal and professional growth and development. The objectives guiding the strategic plan are ensuring effective interventions in determining the specific staffing needs of the facility, regulatory requirements (maximum and minimum number of teachers and gender balance), and the quality of teachers required (years of experience and level of training).
It is important to lay out strategies to meet staffing requirements before the plan’s implementation. DeFoe and Tran (2019) note that change should be justified, meaning that data should be collected to validate the need for hiring and support the strategic plan. Other support interventions such as financial needs, directional strategies, leadership strength, and capacity for the new change should be evaluated. The school must have adequate resources for the strategic plan or a source of funds before preparing for the implementation. In the current world, institutions often hire other organizations and provide their details. These institutions then perform the recruitment on behalf of the facility, cutting costs and time it costs the school to hire staff (Tanjung, 2020).
Peer orientation programs are also widely implemented interventions where fellow teachers are appointed to help others get acquitted with the institution. The deputy school principal will lead the process change, and the dean of students, department heads, deputy principal, and board members will be on the strategic planning committee. The committee will solely make decisions, while the department heads will create the requirements for students in their various departments. The deputy principal will be responsible for drafting the strategic plan and communicating with the board members and other stakeholders, such as recruiting agencies. The deputy will also gather written feedback from all these stakeholders.
Stakeholder Engagement
Institutional The stakeholders of interest are the department heads, school leaders, recruiting agency, board of management, parents, and students. The stakeholders in the team will thus select and appoint a leader/chairperson to the recruitment board to ensure it is within the legal requirements of groups in schools. They will add roles to the members as they deem fit. The stakeholders selected are based on their roles in the strategic plan. According to Kujala et al. (2020), stakeholders’ selection is a crucial step that helps identify and engage personnel responsible for implementing and overseeing activities in any project. The stakeholders selected should all thus have an active role in the change and should be the best-fit professionals for the roles. Parents’ and students’ satisfaction with teachers and their conduct and performance will be integral to evaluating the strategic plan.
The department heads will majorly outline their departments’ requirements, such as staff adequacy, to influence the selection. They will regularly update the board because these needs keep changing. They will also select teachers to mentor and orient the new hire teachers into the organization and oversee the orientation activities. The board members and school leaders (principal and deputy principal) will protect the school’s interest by balancing the needs of the departments with the available organizational resources because they better understand the organization’s state.
They will oversee orientation programs for the new teachers by availing resources such as audits and checklists. Holmes et al. (2019) note that learning institutions should evaluate their staff and regularly evaluate their needs to ensure they meet them and prevent high turnover rates that affect school performance and continuity. The external stakeholders are the recruiting agencies. Most of these agencies are familiar with recruitment requirements of virtually all fields, including learning institutions and schools. The agency will execute the recruitment.
Articulating Mission, Vision, and Values
The third stage in the strategic planning process entails considering the organizational activities’ directional strategies, mission, vision, and values. These directional strategies have a bearing on virtually all organizational activities, including recruiting and staff support. For example, the school is built on Christian faith, and thus, in recruiting, the institution may be oriented to employ more Christian staff or those who believe and uphold the Christian worldview.
The school’s vision is to empower students to acquire, value, and articulate knowledge and skills to support their lifelong learning and contribute to the global community’s development. The mission is to provide high-quality education and safe child care based on the Christian faith in a respectful, inclusive, and supportive environment as a foundation for lifelong learning. The school’s values are respect, trustworthiness, commitment, honesty, humility, and tolerance. These directional strategies will guide the recruitment and support interventions.
The gap analysis shows that the institution lacks adequate teachers and support for these new teachers to meet the vision and mission. In most instances, the teachers are also not adequately supported to meet the needs outlined. The recruited teachers often do not display the school’s requirements to conduct, and there is a high turnover rate as most teachers are discontinued or quit, citing environmental pressure. The goal is to match the directional strategies with organizational needs. The target is to ensure that an adequate number of teachers are hired and that these teachers reflect the values required by the institution. Another target is to ensure that staff employed are supported and amalgamated into the organizational culture and portray the results that will support the achievement of the directional strategies.
Assessing the Environmental Needs
This last step entails conducting a SWOT/TOWS analysis to determine the environmental factors and how they can be leveraged or avoided to ensure quality outcomes. One major threat to the school is well-performing schools in the neighborhood. Parents are drawn to results and values, and institutions with better performance in the area will be preferred over the school. One of the major opportunities is the availability of many professional teachers and numerous recruiting agencies that can help match the school’s needs with the available labor force. The teachers are also educated, with masters and Ph.D. degrees in their respective areas. Another opportunity is that the school is Christian faith-based, encourages inclusion, and receives students from all cultures and faith. The school is thus revered due to the morality it upholds in its students.
One of the internal strengths of the school is its strong financial background. The school has access to resources that can help hire staff and oversee the orientation and support program. For a school, the orientation resources are few, including monetary remuneration for the mentors and record keeping, which can be easily managed using school resources. A major weakness of the school is its current average performance. The school is not at its peak performance, and strategies such as hiring new staff are required to address the weakness. Another weakness is the perceived lack of support from the leaders. See et al. (2020) note that a lack of organizational leadership support is one of the major problems leading to a high turnover in facilities. Other weaknesses include the lack of a strong leadership structure that can oversee staff recruitment and integration, necessitating a recruitment agency. The opportunities and strengths will help overcome the weaknesses and threats to contribute to the overall school growth.
Conclusion
Staff recruitment and support are integral processes in achieving institutional goals and objectives. This strategic plan focused on improving the hiring process and supporting new staff. Stakeholder selection is important to project success because it helps identify the best-fit professionals to perform the roles at hand. External stakeholders supplement organizational work and thus play vital roles in organizational success. The strategies outlined, such as utilizing an external agency, will help ensure the recruitment process is flawless and meets the organizational needs.
Benchmark – Staffing Matrix And Reflection References
DeFeo, D. J., & Tran, T. C. (2019). Recruiting, Hiring, and Training Alaska’s Rural Teachers: How Superintendents Practice Place-Conscious Leadership. Journal of Research in Rural Education, 35(2). https://doi.org/10.26209/jrre3502
Holmes, B., Parker, D., & Gibson, J. (2019). Rethinking teacher retention in hard-to-staff schools. Contemporary Issues in Education Research (CIER), 12(1), 29–34. https://doi.org/10.19030/cier.v12i1.10260
Kujala, J., Sachs, S., Leinonen, H., Heikkinen, A., & Laude, D. (2022). Stakeholder engagement: Past, present, and future. Business & Society, 61(5), 1136-1196. https://doi.org/10.1177/00076503211066595
See, B. H., Morris, R., Gorard, S., & El Soufi, N. (2020). What works in attracting and retaining teachers in challenging schools and areas? Oxford Review of Education, 46(6), 678-697. https://doi.org/10.1080/03054985.2020.1775566
Tanjung, B. N. (2020). Human resources (HR) in education management. Budapest International Research and Critics in Linguistics and Education (BirLE) Journal, 3(2), 1240-1249. https://doi.org/10.33258/birle.v3i2.1056
READ MORE >>
Benchmarking: Xerox Corporation PaperIntroductionIn the 70s and the early 80s, X ...
Benchmarking: Xerox Corporation Paper
Introduction
In the 70s and the early 80s, Xerox Corporation was one of the leading copier companies in the world. However, towards the 1990s, the company began to lose significant market share to Japanese and American copier firms. Numerous mistakes by the firm such as the managements’ failure to give direction and the firm’s failure to observe market trends cost it its position at the top. The biggest failure on the part of Xerox Corporation was to ignore new entrants that came in with more efficient models. These factors saw the company lose market share and profits to these new entrants. To bring back the company to its former glory, the management instituted sweeping changes through benchmarking.
Xerox Corporation Benchmarking
John T. Kearns became the CEO of Xerox Corporation in 1952. Kearns quickly discovered that his Japanese competitors effortlessly undercut Xerox’s prices because they produced copiers at 40-50% less than that of Xerox. Kearns decided to learn how he could bring back Xerox to profitability by using benchmarking. The CEO introduced a program called ‘Leadership through Quality’ as a strategy to revitalize the company.
Through benchmarking, the company’s CEO found that his company took twice as long to avail the company’s product to the market compared to his Japanese competitors. Other results that the CEO of Xerox found out through benchmarking are that the Japanese competitors could manufacture, ship, and sold units for the same amount that it cost Xerox on manufacturing only (Riva, & Pilotti, 2019). Secondly, Xerox products had more defects per part, about 30 times that of its competitors. Besides, the company had more engineers, about five times that of its competitors, yet the competitors’ were more efficient and profitable. With all these problems, it would take Xerox Corporation about five years to catch up with its competitors.
The course of Action and Current Status
Faced with the reality of the situation, Xerox Corporation began to collect critical data-based practices from the best-performing companies in its industry. The management analyzed and evaluated each practice to identify the improvement opportunities each presented. In particular, the company identified ten critical aspects on marketing alone that were further fine-tuned into 67 sub-categories that became targets for improvement (Intrisano et al., 2017). Besides marketing, Xerox also targeted other critical areas for improvement that included quality improvement, supplier relation and development, safety, efficiency, and lean operations.
Between the late 80s and the early 90s, Xerox Corporation began to reap from best practices it implemented from benchmarking. For example, by 1991, the company had reduced defects of its machines by an impressive score of 78 per 100 machines. Besides, sales units within the country improved from 152% to 328% indicating positive growth and profitability. By the late 1990s, Xerox Corporation became the only company in the world to win the three-most prestigious quality awards (Kozena, M., & Kocvarova, 2017). By the 2000s, Xerox Corporation became the leading copier firm that other firms worldwide looked up to for benchmarking. Leading companies like Toyota, Citicorp, IBM, Ford, and General Electric have joined hands with Xerox to the International Benchmarking Clearinghouse to promote benchmarking across the world.
Conclusion
Xerox Corporation turned around its losing streak in the 80s through benchmarking. The company identified several best practices from leading firms and incorporated them into its operations. Through benchmarking, Xerox Corporation rose to become one of the leading firms that successfully used benchmarking to turn failure into success.
References
- Intrisano, C., Micheli, A. P., Calce, A. M., & Di Nallo, L. (2017). Economic and Financial Benchmarking as a Strategic Planning Tool. International Journal of Economics and Financial Issues, 7(6), 175. http: www.econjournals.com
- Riva, A., & Pilotti, L. (2019). The strategy and the evolution of benchmarking methodology: the case of Rank Xerox-Fuji. Economia Aziendale Online-, 10(2), 273-291. https://doi.org/10.13132/2038-5498%2F10.2.1960
- Kozena, M., & Kocvarova, L. (2017). Evaluating Company Performance Through The Use Of Benchmarking. In 4th International Multidisciplinary Scientific Conference on Social Sciences and Arts Sgem 2017, 3(), 279-286. DOI: 10.5593/sgemsocial2017/13/S03.036
READ MORE >>
NHS-FPX6004 Benchmark Underperformance Dashboard Metrics ExampleBenchmark Underp ...
NHS-FPX6004 Benchmark Underperformance Dashboard Metrics Example
Benchmark Underperformance Dashboard Metrics Example
Benchmark Underperformance Dashboard Metrics Example
Benchmark Underperformance
Name
Institution
Benchmark Underperformance
Healthcare dashboards are crucial in determining the organization’s performance and indicators of quality. Dashboards and reports on performance provide critical information on how well the organization is performing on different fronts Benchmark Underperformance Dashboard Metrics Example. A digital dashboard such as Mercy Medical Center is sharable and can be used in outlining gaps in performance and implementing the necessary interventions to improve health care organization performance and quality of care.

Understanding benchmark underperformance as highlighted in local, state, and federal government policies and benchmarks will ensure effective quality improvement and improved outcomes in care Benchmark Underperformance Dashboard Metrics Example. This paper is an evaluation of Mercy Medical Center (Shakopee, MN) dashboard to outline areas of underperformance and suggest ethical action towards meeting set benchmarks.
Evaluation of Dashboard Metrics
After evaluation of the dashboard, several aspects have been noted with the patient records and trends in the organization. Two major areas of concern can be seen in this data; low HgbA1c tests and foot exam rates Benchmark Underperformance Dashboard Metrics Example. The highest number of foot exam rates indicated in the dashboard was 73 in 2019 Q1 and this declined to only 3 in Q4 of the same year (Vila Health, n.d.). HgbA1c test rates have also declined notably from 123 in 2019 Q1 to only 6 in Q4 (Vila Health, n.d.).
These tests are important in monitoring glycemic control as well as diabetes complications and hence the decline in testing rates presents a major health concern Benchmark Underperformance Dashboard Metrics Example. The tests are considered crucial in preventing diabetes complications and hence decline in the rates of tests shows poor outcomes.
When comparing these two areas of assessment with the state and national benchmarks, it is evident that they fail to meet the benchmark for both state and national outcomes. The numbers provided in the dashboard have not indicated percentages hence a major assumption made here is that the highest number is the total of diabetes patients. Assuming that the total number of patients is 123, only 6 (48.7%) received the HgbA1c tests in Q4 2019 compared to the national benchmark of 79.5%.
The state benchmark for Minnesota is 78.0% hence HgbA1c tests fall below both benchmarks (AHRQ, 2020). Similarly, in foot examinations, only 3 (24.4%) were examined in 2019 Q4 which falls below the national benchmark of 84.0% and Minnesota benchmark of 84.1% (AHRQ, 2020). Benchmark Underperformance Dashboard Metrics Example Therefore, when compared with the state and national rates, testing for diabetes-related complications at Mercy Medical fails to meet the required benchmarks.
The benchmarks against which this performance is compared are based on the National Healthcare Quality and Disparities Reports by the Agency for Healthcare Research and Quality (AHRQ). The agency derives the measures from top-performing states to compare achievable benchmarks with the performance of the rest of the country (AHRQ, 2020). These comparisons are used as part of the AHRQ agenda for continuous improvement and the Centers for Medicare and Medicaid Services (CMS) incentives to states and hospital organizations.
The data on Mercy Medical Center’s Dashboard also presents several areas of uncertainty where more information would help. For example, data on new diabetes patients is incomplete since the dashboard does not indicate the total new numbers in previous quarters. Similarly, the numbers of practitioners and facilities reported do not have comparators hence one cannot accurately tell whether the resources are adequate for the practice. More information on acuity and utilization level for the staff and facilities respectively would help in assessing the adequacy of resources in the organization. Benchmark Underperformance Dashboard Metrics Example
Challenge in Achieving Acceptable Performance
Several challenges may be experienced in achieving acceptable performance and for Mercy Medical Center, resources may be one of the biggest challenges Benchmark Underperformance Dashboard Metrics Example. The identified performance gaps include decline in testing and examination rates for patients with diabetes. Improvement in these performance areas would require more education and outreach to patients with diabetes.
Resources required for such an intervention include community education and facilitation resources as well as training finances required for the training processes. Benchmark Underperformance Dashboard Metrics Example
The high demands for resources and finances would thus present a challenge for the organization in improving current performance. Lack of resources means that the medical center does not provide enough education to the community and hence fewer people get tested and examined for diabetes complications Benchmark Underperformance Dashboard Metrics Example. The assumption made in this analysis is that the organization does not have a current diabetes education program in Shakopee, MN.
Specific Target for Improvement
The dashboard presents many areas of improvement which medical center can focus its efforts to produce better results and achieve the best overall improvement in quality outcomes. Areas of improvement can be chosen based on severity of the issue, number of affected patients, financial impact, and stakeholders involved in the process Benchmark Underperformance Dashboard Metrics Example. A crucial area of improvement is the testing and evaluation of diabetes and diabetes-related conditions.
According to the American Diabetes Association (2017), early detection of diabetes complications can aid in reducing the progress of the condition and hence significantly improving the quality of life for the patients Benchmark Underperformance Dashboard Metrics Example. Eye examination, foot evaluation, and HgbA1c tests are crucial areas of improvement since they enhance the quality of care for patients with diabetes and hence produce better health outcomes.
Another area of improvement that can be outlined in the medical center is the staffing levels. Although the dashboard does not clearly indicate gaps in staffing rates at Mercy Medical Center, staffing is one of the crucial areas of improvement that healthcare organizations in general should consider. This is because staffing levels and burnout rates are correlated with the quality of care and patient satisfaction (Gillet et al., 2018).
Staffing levels also affects a huge number of stakeholders starting with the patients, staff, and even the management. It is thus justifiable that the organization should focus on improving staffing levels hence enhancing care quality and outcomes Benchmark Underperformance Dashboard Metrics Example. The proposed improvement should thus focus on proactive diabetes care as well as staffing levels to improve care quality and reduce underperformance gap. Benchmark Underperformance: Dashboard Metrics Example
Suggested Actions for Performance Improvement
Based on the evaluation, it becomes evident that ethical action should be implemented to enhance the quality of care in Mercy Medical Center. The proposed ethical action is two-pronged. The first approach is to carry out patient education on diabetes care for reducing complications. This education program will target the community in general and also focus on diabetic patients specifically.
Community-targeted diabetes education reduces diabetes complications and adherence to treatment plan (Kwan et al., 2020). The education project could include community-based programs and in-clinic education approaches. The action is considered ethical because it increases patients’ health knowledge and will increase self-care and continuity in diabetes management. Benchmark Underperformance Dashboard Metrics Example
The second aspect of care improvement is assessing staffing needs and improving current staffing levels to support quality improvement. Staffing needs can be assessed through an overview of nurse acuity and provider: patient ratios in the organization. The staffing needs assessment will then be followed by a recruitment and training program to equip the organization with the relevant staff resources required to deliver high quality care.
The impact of this project will be positive quality-wise and will also benefit staff and patients. Better staffing levels will reduce burnout and increase job satisfaction while providing the relevant expertise and workforce for quality care and improvement Benchmark Underperformance Dashboard Metrics Example. Therefore, combining staffing improvements with diabetes education will significantly improve the quality of care and performance at Mercy Medical Center.
Benchmark Underperformance Dashboard Metrics Example Conclusion
The dashboard analysis is useful in determining areas of underperformance and pinpointing the need for improvement in the health care organization. This deliverable has shown that Mercy Medical Center could improve the quality of care by enhancing patient knowledge about diabetes-related examinations and tests. Also, improved staffing levels are useful in facilitating overall care quality improvement. The dashboard analysis provides a basis for care improvement and enhances quality outcomes by justifying interventions in the health care organization. Benchmark Underperformance Dashboard Metrics Example
Benchmark Underperformance Dashboard Metrics Example References
- Agency for Healthcare Research and Quality (AHRQ). (2020). Minnesota: Diabetes Quality Measures Compared to Achievable Benchmarks. National Healthcare Quality and Disparities Reports. https://nhqrnet.ahrq.gov/inhqrdr/Minnesota/benchmark/table/Diseases_and_Conditions/Diabetes
- American Diabetes Association. (2017). 10. Microvascular complications and foot care. Diabetes Care, 40(Supplement 1), S88-S98. https://doi.org/10.2337/dc17-S013
- Gillet, N., Fouquereau, E., Coillot, H., Cougot, B., Moret, L., Dupont, S., … & Colombat, P. (2018). The effects of work factors on nurses’ job satisfaction, quality of care and turnover intentions in oncology. Journal of Advanced Nursing, 74(5), 1208-1219. https://doi.org/10.1111/jan.13524
- Kwan, B. M., Dickinson, L. M., Glasgow, R. E., Sajatovic, M., Gritz, M., Holtrop, J. S., … & Waxmonsky, J. A. (2020). The Invested in Diabetes Study Protocol: a cluster randomized pragmatic trial comparing standardized and patient-driven diabetes shared medical appointments. Trials, 21(1), 65. https://doi.org/10.1186/s13063-019-3938-7
- Vila Health. (n.d.). Dashboard and Health Care Benchmark Evaluation. Capella University. https://media.capella.edu/CourseMedia/nhs6004element17010/wrapper.asp
Benchmark Underperformance: Dashboard Metrics Example Instructions
Choose one of the following two options for a performance dashboard to use as the basis for your evaluation:
Option 1: Dashboard Metrics Evaluation Simulation
Use the data presented in your Assessment 1 Dashboard and Health Care Benchmark Evaluation activity as the basis for your evaluation.
Note: The writing you do as part of the simulation could serve as a starting point to build upon for this assessment.
Option 2: Actual Dashboard
Use an actual dashboard from a professional practice setting for your evaluation. If you decide to use actual dashboard metrics, be sure to add a brief description of the organization and setting that includes:
- The size of the facility that the dashboard is reporting on.
- The specific type of care delivery.
- The population diversity and ethnicity demographics.
- The socioeconomic level of the population served by the organization.
- Benchmark Underperformance Dashboard Metrics Example
Note: Ensure your data are Health Insurance Portability and Accountability Act (HIPAA) compliant. Do not use any easily identifiable organization or patient information.
To complete this assessment:
- Review the performance dashboard metrics in your Assessment 1 Dashboard and Health Care Benchmark Evaluation activity, as well as relevant local, state, and federal laws and policies. Consider the metrics that are falling short of the prescribed benchmarks. Note: The writing you do as part of the simulation could serve as a starting point to build upon for this assessment.
- Write a report for a senior leader that communicates your evaluation of current organizational or interprofessional team performance, with respect to prescribed benchmarks set forth by government laws and policies at the local, state, and federal levels. In addition, advocate for ethical and sustainable action to address benchmark underperformance and explain the potential for improving the overall quality of care and performance, as reflected on the performance dashboard.
- Make sure your report meets the Report Requirements listed below. Structure it so that it will be easy for a colleague or supervisor to locate the information they need, and be sure to cite the relevant health care policies or laws when evaluating metric performance against established benchmarks.
- Benchmark Underperformance Dashboard Metrics Example
Report Requirements
The report requirements outlined below correspond to the scoring guide criteria, so be sure to address each main point. Read the performance-level descriptions for each criterion to see how your work will be assessed. In addition, be sure to note the requirements for document format and length and for supporting evidence.
- Evaluate dashboard metrics associated with benchmarks set forth by local, state, or federal health care laws or policies.
- Which metrics are not meeting the benchmark for the organization?
- What are the local, state, or federal health care policies or laws that establish these benchmarks?
- What conclusions can you draw from your evaluation?
- Are there any unknowns, missing information, unanswered questions, or areas of uncertainty where additional information could improve your evaluation?
- Analyze the consequence(s) of not meeting prescribed benchmarks and the impact this has on health care organizations or teams.
- Consider the following examples:
- Organizational mission and vision.
- Resources.
- Staffing.
- Financial: Operational and capital funding.
- Logistical considerations: Physical space.
- Support services (any ancillary department that gives support to a specific care unit in the organization, such as pharmacy, cleaning services, dietary, et cetera).
- Cultural diversity in the community.
- Staff skills.
- Procedures and processes.
- Address the following:
- What are the challenges that may potentially contribute to benchmark underperformance?
- What assumptions underlie your conclusions?
- Consider the following examples:
- Evaluate a benchmark underperformance in a heath care organization or interprofessional team that has the potential for greatly improving overall quality or performance.
- Focus on the benchmark you chose to target for improvement. Which metric is underperforming its benchmark by the greatest degree?
- State the benchmark underperformance that is the most widespread throughout the organization or interprofessional team.
- State the benchmark that affects the greatest number of patients.
- Include how this underperformance will affect the community that the organization serves.
- Include the greatest opportunity to improve the overall quality of care or performance of the organization or interpersonal team and, ultimately, to improve patient outcomes, as you think about the issue and the current poor benchmark outcomes.
- Advocate for ethical and sustainable action(s), directed toward an appropriate group of stakeholders, needed to address a benchmark underperformance.
- Who would be an appropriate group of stakeholders to act on improving your identified benchmark metric?
- Why should the stakeholder group take action?
- What are some ethical actions the stakeholder group could take that support improved benchmark performance?
- Organize content so ideas flow logically with smooth transitions.
- Proofread your report, before you submit it, to minimize errors that could distract readers and make it more difficult for them to focus on the substance of your evaluation and analysis.
- Support main points, assertions, arguments, conclusions, or recommendations with relevant and credible evidence.
- Be sure to apply correct APA formatting to source citations and references.
- Benchmark Underperformance Dashboard Metrics Example
Report Format and Length
Format your report using APA style.
- Use the APA Style Paper Tutorial [DOCX] to help you in writing and formatting your report. Be sure to include:
- A title and references page. An abstract is not required.
- Appropriate section headings.
- Your report should be 3–5 pages in length, not including the title page and references page.
Supporting Evidence
Cite 4–6 credible sources from peer-reviewed journals or professional industry publications to support your analysis of challenges, evaluation of potential for improvement, and your advocacy for ethical action.
Dashboard and Health Care Benchmark Evaluation
Dashboards and other reports can provide crucial information about how well an organization is meeting benchmarks set by local, state, and federal laws and policies. Healthcare organizations need to be able to use this information to determine the most effective strategies for quality and performance improvement. This activity asks you to review a diabetes dashboard and fact sheet used by Mercy Medical Center, a Vila Health affiliated hospital, and determine where the organization is falling short.
Scatterdesk
Public Health Dashboard – Diabetes
New Patients Last Quarter by Race
- African American – 17 (3 percent)
- American Indian – 73 (13 percent)
- Asian – 34 (6 percent)
- White – 355 (63 percent)
- Other – 11 (2 percent)
- Blank/Declined – 73 (13 percent)
New Patients Last Quarter by Gender
- Male – 214 (38 percent)
- Female – 347 (62 percent)
- Blank/Declined – 2
New Patients Last Quarter by Age
- 20 or younger – 118 (21 percent)
- 21-39 – 51 (9 percent)
- 40-64 – 214 (38 percent)
- 65+ – 180 (32 percent)
- Blank/Declined – 0
Fact Sheet
Mercy Medical Center (Shakopee, MN)
Mercy Medical Center is one of the region’s top choices for high quality health care. Don’t just take our word for it, though. Here are some of the accolades we’ve received:
- Highest Safe Surgery Rating by a consumer advocacy magazine.
- Healthgrades Outstanding Patient Experience Award.
- Shakopee Ledger Top 20 Workplaces 2020 and 2021.
- Women’s Choice Award for the Best Hospital for Patient Experience in Emergency Care.
Shakopee Demographics
FemaleMaleTotal Population18,23517,95736,192< 2021-4445-64> 6512,12614,7326,0992,371WhiteAsianHispanic – LatinoOtherAfrican AmericanTwo or more racesAmerican Indian28,537 (76 percent)3,822 (10 percent)2,890 (7 percent)1,661 (4 percent)1,601 (4 percent)1,016 (4 percent)433 (1 percent)Shakopee Ledger
Top 20 Workplaces 2020 & 2021
20102021Hospital Rooms (All Private)62 (70 licensed)85 (93 licensed)Medical/Surgical Rooms3356Special Care Unit88Family Birth Rooms1717Children’s Care Pediatric Rooms44Operating Rooms5 and 1 C – Section8 and 1 C – SectionEmergency Room Treatment Bays1621Endoscopy Rooms222021Physicians433Volunteers (15 — 94 years old)200Inpatient Admissions5,735Surgical Procedures4,627Births1,328Emergency Room Visits29,893Urgent Care Visits9,586Outpatient Encounters119,535Physical, Occupational, Speech/Language Therapy Visits28,636Pediatric Therapy Visits11,987Sleep Center Visits783Radiology Procedures59,335Cardiac Rehab Visits7,158Cardiopulmonary Visits19,676Cancer Center Visits7,781Now that you’ve reviewed the data answer the following questions:
What are the biggest areas of concern with regards to the information in Mercy Medical Center’s Public Health Dashboard – Diabetes?
Your response:
This question has not been answered yet.
While there are a few areas of concern present in the diabetes public health dashboard, the two biggest areas of concern are the declining HgbA1c exams and the low foot exam rate. Both of these tests are important tests to help identify potential diabetes related complications early. Benchmark Underperformance Dashboard Metrics Example
Some areas that are not concerns, or there is not enough data to say for sure are as follows
The number of eye exams has fluctuated over the last two years. It is about 6 times what it was in first quarter of 2018. and it is four to nine times more than the foot and HgbA1c exams. It could probably be better, but it is not one of the biggest areas of concern.
With regard to the data on new diabetes patients, this dashboard has no information on the total number of new patients in previous quarters. So the new patient numbers cannot definitively be called an issue based on the data available.
Looking at the statement regarding patients aged 20 or younger, similar to the new patient statement, there is not enough data within this dashboard to label it as one of the biggest areas of concern.
Select one of the underperforming metrics. Why and how would improving this metric contribute to the overall success of Mercy Medical Center? Benchmark Underperformance Dashboard Metrics Example
Your response:
This question has not been answered yet.
There is no one right answer for this question. When looking for areas to improve within a care setting it is important to consider factors such as:
- The severity of the issue.
- The number of patients affected.
- Any financial impacts.
- Stakeholders involved.
- Measureable outcomes.
- Benchmark Underperformance Dashboard Metrics Example
By building an objective, evidence-based case around these considerations, in addition to any legal or regulatory factors, it is possible to reach a good decision about improvement projects to pursue.
Benchmark Underperformance Dashboard Metrics Example Conclusion
In this activity, you had the opportunity to review various dashboards and other reports in order to evaluate Mercy Medical Center’s performance against local, state, and federal requirements. Use the information you acquired here as well as external research into appropriate standards to complete your course assignment. Benchmark Underperformance Dashboard Metrics Example
READ MORE >>
Juggling nursing school with a job proves challenging yet financially essential ...
Juggling nursing school with a job proves challenging yet financially essential for many students lacking external support. Attempting full-time employment on top of rigorous clinical rotations and didactic courseloads pushes limits for even the most dedicated learners. Finding optimal work arrangements that accommodate academic priorities becomes vital to prevent burnout.
Discover how structuring strategic shift schedules, upholding boundaries, and embracing time-saving techniques help learners balance intensive programs and career growth.
Can You Work While In Nursing School?
Yes, working stays possible in nursing school, but it requires supreme organization, self-care, and flexibility, maximizing earning hours without compromising grades or program completion. While no universal formulas guarantee success, proactive planning, priority management, and resource utilization help many nursing students work competitively.
Working During Nursing School
Most BSN students cannot afford to abandon income streams entirely while completing nursing programs. Many enroll as second-career students needing sustained incomes, health benefits, and family support through existing jobs. Other younger prospects find summertime savings inadequate, covering tuition, clinical supplies, testing fees, living costs, and technology needs across high-demand curriculums.
Letting financial instability sabotage education options makes little sense when reasonable working accommodations are integrated. But blindly overcommitting work hours risks poor academic performance too. Finding reasonable balances works best.
Best Work Schedule for Nursing School
Select scheduling allowing reliable income generation without missing critical nursing student obligations works optimally for learners managing both roles.
Fulltime Day Shift Work Schedule: 36 hours
Maintaining consistent, evenly distributed 36-hour day shift weeks allows for attending daily classes and local clinical rotations when available. Group project meetings also stay manageable depending on shift start/end times. This schedule allows some flexibility for changing school demands. However, long shifts require applying time and self-care strategies to protect sleep. You can also have a night shift schedule to align with your classes.
Part-time Day Shift Weekend Work Schedule: 24 hours
Clustering longer shift blocks exclusively on weekends creates ample free days and evenings for attending school and studying after work. The flip side means surrendering family and social time fully on weekends at work. Successfully separating contexts prevents school and work from overlapping. This schedule best suits dedicated students lacking kids or local social ties needing weekend attention.
The Challenges of Working a Full-Time Job While in Nursing School
Students working full hourly quotas while completing rigorous nursing curriculums encounter steep challenges, including:
Time Management
Packed class, clinical, work, and commute schedules mandate meticulous planning, balancing competing demands without sacrifices. This juggle proves difficult initially before establishing firm boundaries.
Physical and Emotional Fatigue
Long shifts on the feet coupled with mental healthcare strain before heading to school reliably trigger enormous cumulative fatigue over weeks. Managing energy levels and preventive self-care becomes essential.
Academic Pressure
Pre-licensure nursing programs load intensive foundational content spanning sciences, technical skills, and critical thinking, requiring copious studying. Working full-time easily distracts attention from academics.
Clinical Rotations and Shift Work
Rotating clinical shifts assigned at the last minute provides little control or predictability when managing hourly job schedules. Being perpetually available while rotating days and nights means no days “off.”
Maintaining a Social Life
Heavy work-life imbalance strains personal relationships needing attention. Isolation and burnout manifest quickly.
How to be Successful at Working Full-Time in Nursing School
Utilize the following reliable techniques to reconcile better working whole duty while attending rigorous nursing programs:
Effective Time Management
Block schedules meticulously plotting school, work, study sessions, self-care, errands, and family time using planners and phone alerts. Account for commute and preps within time budgeting.
Open Communication
Inform instructors, preceptors, managers, and family of student-employee status, prompting accommodations if feasible. Network for backup support coverage.
Self-Care
Prioritize proper sleep, nutrition, exercise, and mental health interventions to manage heightened stress levels proactively. Burnout prevention equals survival.
Utilize Support Systems
Access college academic advising departments for provided guidance like tutoring, counseling, or disability resources when applicable. Join student-worker forums too.
Set Realistic Expectations
Acknowledge specific career, financial, or social aspects that might need temporary downsizing to prevent feeling overwhelmed. Define what matters most right now and delay other goals.
5 Benefits Of Working Full-Time While In Nursing School
Despite genuine difficulties working full-force while learning care professions, tangible benefits beyond financial necessity arise as well, including:
Networking Opportunities
Campus jobs and healthcare settings offer invaluable foot-in-door networking, mentorships and hiring pipelines unavailable otherwise. Make professional connections!
No Stressing About Bills
Maintaining steady incomes prevents destabilizing moves home or dropping out. Bills keep getting paid!
Gain Experience
Early exposure to diverse healthcare settings and specialties builds impressive resumes through extended hands-on learning. This accelerates post-graduate hiring dramatically.
No Worry About Student Loans
Paying out-of-pocket program costs through work earnings reduces loan burdens or interest rates.
Steady Income
Reliable paychecks allow for better management of fixed budgets through predictable forecasting reliability. Saving for emergencies or lifestyle wants becomes more realistic than living only upon financial aid dispersals.
What Are The Most Convenient Full-Time Jobs For Nursing Students?
Factor program schedules and transportation access when selecting compatible nursing student jobs, allowing manageable sustainability:
Phlebotomist: Learn clinical skills working flexible hours on recall rosters, allowing class attendance. Gain healthcare exposure!
Ward Clerk: Coordinates unit communications and clerical functions on nursing floors with semi-flexible shifts possible around the school. Observe environments!
Hospital Transport: Campus hospitals gladly schedule full-timers around course times to transport patients and equipment without rigid hourly demands. Know facilities!
Certified Nursing Assistant: Find per-diem CNA aide roles that offer needed PRN pay without overly burdensome clinical rotations conflicting with clinicals. Master bedside care!
Tutor: Help other students grasp academic concepts, working personable shifts from campus libraries and labs. Review foundational knowledge!
Personal Care Attendant: Caring for clients on shifts individually set week-to-week works perfectly for changing school calendars. Bonus skills!
Call Center Representative: Remote health system phone positions allow for the reliable balance of school and earnings simultaneously from home bases.
Virtual Assistant: Find students online administrative gigs through freelancing platforms offering supreme shift control despite total workloads. Show technical talents!
Sales Associate: Major retailers staff ample weekend floor associate roles, ideal for weekday clinical attendees needing stable income. Learn customer service grace!
Social Media Manager: Digital marketers hire students to manage client accounts and campaigns from campus and remote spots week-to-week. It’s a great experience!
What Does A Typical Day Look Like For A Student Attending Nursing School And Working Full Time?
Fitting full-time nursing school schedules and full-time work into 24-hour mandates strictly organized efforts:
4:30 AM: Wake up to exercise and prep for morning clinical rotation
6:30 AM – 3:30 PM: Clinical hours
4:00 – 7:00 PM: Attend evening classes/study group
8:00 – 11:00 PM: Complete assigned reading and care plans after dinner
11:30 PM: Prepare uniforms and supplies for the next day
12:00 AM: Bedtime
Alternate school blocks with hourly shifts or double-up weekend shifts with online coursework. Pack meals, stay organized, alternate tasks with short breaks, and claim moments celebrating small accomplishments to maintain motivation. Some days will feel impossibly grueling and others surprisingly smooth – stay patient and consistently balance both worlds through self-compassion and planning.
Working full-time in Nursing School
Can students work full-time while they go to nursing school? Yes, but only through carefully constructed work-life integration techniques prioritizing school using hyper-organization, routine self-care, candid communication, and unrelenting time management.
By remaining determined, vulnerable, and responsive when aspects overwhelm them, learners working full-duty persist in earning those treasured nursing degrees and registered nurse licenses serving communities.
READ MORE >>
BHA FPX 4020 Assessment 1 Health Care Problem Analysis ProposalHealthcare Proble ...
BHA FPX 4020 Assessment 1 Health Care Problem Analysis Proposal
Healthcare Problem Analysis Proposal
Healthcare systems in the US bear the obligation to achieve a triad objective of improving the patient experience of care, including quality and satisfaction, improving public health services, and reducing the cost of care. Despite these considerations, Americans do not receive quality, timely, and affordable care due to the prevailing healthcare disparities.
According to the Agency for Healthcare Research and Quality (AHRQ) (2021), a healthcare disparity is a “difference between population groups in the way they access, experience, and receive healthcare” (p. 193). In this sense, the synergies between ethnic, social, economic, environmental, and geographical factors contribute to inequalities regarding access to care, experiences, and quality of life.
Although the country enacts policies that ensure affordability, accessibility, and equality, eliminating ethnic and socio-economic disparities poses a public health challenge. Therefore, this proposal elaborates on strategies for measuring and assessing healthcare disparities, quality benchmarks, and evidence-based strategies for addressing the problem.
Measurements and Assessment of the Problem
It is possible to measure and assess the problem of healthcare disparities by evaluating interactions between health and social determinants of health (SDOH), including age, education, neighborhood, employment, and population’s income levels. Also, it is essential to incorporate ethnic aspects because they influence access to quality care, experiences, and quality of life. The Agency for Healthcare Research and Quality (AHRQ) (2021) presents six profound domains for assessing disparities. These considerations are:
- Access to person-centered care
- Patient Safety
- Care coordination
- Care affordability
- Effective treatment
- Healthy living
Benchmarks for Healthcare Disparities
Often, it is possible to determine the prevailing health disparities by comparing the community’s performance against top-performing communities and state or national benchmarks. As noted earlier, it is vital to assess and measure health disparities by evaluating inequalities within the six domains, including access to patient-centered care, the level of care coordination, care affordability, the availability of effective treatment, and healthy living.
Gomez et al. (2021) argue that conditions in which people live, learn, work, and worship, alongside their age and growth patterns, influence well-being outcomes, quality of life, and access to timely, affordability, and quality care. Therefore, the social determinants of health (SDOH) are the causative and contributing factors for health disparities.
The Agency for Healthcare Research and Quality (AHRQ) collaborates with other agencies such as the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services (CMS) to document national and state benchmarks for the six domains. In this sense, it is possible to gauge communities’ performance regarding eliminating healthcare disparities by comparing their prevalence with states’ and national benchmarks.
One of the most profound benchmarks for healthcare disparities is the number of uninsured people of ethnic diversities. Carratala & Maxwell (2020) argue that about 10.6% of African Americans were uninsured compared with 5.9% of non-Hispanic Whites in 2017. Such statistics indicate ethnicity is a profound cause of disparities in care affordability and accessibility.
The stand unit for measuring health disparities entails often computing the total number of individuals with distinct characteristics against a predetermined population (1000, 100000, and so on). For example, healthcare professionals can calculate the total number of Black Americans with new cases of HIV by identifying the numbers of new cases per 100,000 people. Consequently, it is possible to compare the prevalence of disparities with achievable benchmarks.
Action Plan
Many scholarly and authoritative sources proposed evidence-based interventions for analyzing and addressing health disparities in patient safety, access to quality care, care affordability, quality of life, and care coordination. These interventions include:
- Identifying and addressing contextual issues contributing to healthcare disparities (Suarez-Balcazar et al., 2017). it is essential to understand the linkage between social determinants of health (SDOH) and access to care, affordability, care coordination, and quality of life.
- Initiating organizational, provider-focused, and systematic changes to reduce racial healthcare disparities (Gullost et al., 2018).
- Eliminating structural racism in healthcare organizations to promote fairness and equality at the institutional level (Lavizzo-Mourey et al., 2021)
- Ensuring equality when distributing socio-economic resources reduces disparities within the social determinants of health, such as housing, health literacy, work conditions, and employment status (Gomez et al., 2021).
- Implementing care transformative care delivery and financial arrangements to transform healthcare reimbursement strategies, including national insurance models to enhance accessibility and affordability (Garzon-Orjuela et al., 2020).
American College of Healthcare Executives (ACHE) Leadership Competencies
ACHE DomainACHE Competency SelectedHow This Competency Related to the Capstone Health Care Problem Analysis ProposalCommunication and Relationship ManagementCommunication Skills Communication competencies are prerequisites for effectively disseminating information and evidence regarding clinical problems as a healthcare professional. According to the American College of Healthcare Executives (ACHE) (2020), communication skills enhance an individual’s ability to communicate clearly and concisely with internal and external audiences, establish and maintain relationships, and facilitate constructive interactions with team members. This competency is consistent with the capstone project analysis because it entails developing interdisciplinary teams for change implementation.LeadershipManaging ChangeUndoubtedly, understanding the change process is essential for inspiring evidence-based interventions to address health disparities. ACHE (2020) contends that effective leadership entails inspiring individuals and organizational excellence by creating a shared vision and successfully managing change. Therefore, this competency complements the need to initiate, implement, and sustain approaches for addressing health disparities.ProfessionalismPersonal and Professional AccountabilityAs noted earlier, it is essential to eliminate structural discrimination in healthcare organizations to address health disparities such as access to quality care for disadvantaged patient populations, care coordination issues, and patient safety concerns (Lavizzo-Mourey et al., 2021).Personal and professional accountability is a prerequisite for ensuring equality at the institutional level because it aligns with ethical and professional standards. This competency relates to the capstone healthcare problem because it requires healthcare professionals to uphold ethical and professional practice standards, eliminating structural disparities such as discrimination.Knowledge of the Healthcare EnvironmentalHealthcare Systems and OrganizationsThe problem of health disparities prompts healthcare professionals and policymakers to understand the synergies between social determinants of health (SDOH) and domains of quality care, including accessible, affordable, and coordinated care.
Therefore, it is essential to understand external and internal organizational environments, including healthcare delivery systems like insurance and reimbursement models. Therefore, this competency aligns with the capstone healthcare problem because it emphasizes understanding care dynamics and their contribution to health disparities.Business Skills and KnowledgeQuality ImprovementQuality improvement is an essential concept in the current healthcare systems because it emphasizes interventions for bolstering care quality, accessibility, and affordability, alongside other dimensions of quality care.
Healthcare professionals should familiarize themselves with implementing evidence-based recommendations for clinical problems. This competency aligns with the capstone healthcare problem analysis because it entails understanding organizational capacity and aspects that improve dimensions of quality care.
BHA FPX 4020 Assessment 1 Health Care Problem Analysis Proposal References
Agency for Healthcare Research and Quality. (2021). National healthcare quality and disparities report (pp. 1-316). AHRQ. https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2021qdr.pdf
American College of Healthcare Executives. (2020). ACHE healthcare executive: 2020 competencies assessment tool. https://www.ache.org/-/media/ache/career-resource-center/competencies_booklet.pdf.
Carratala, S., & Maxwell, C. (2020). Health disparities by race and ethnicity. https://www.americanprogress.org/article/health-disparities-race-ethnicity/
Garzón-Orjuela, N., Samacá-Samacá, D., Luque Angulo, S., Mendes Abdala, C., Reveiz, L., & Eslava-Schmalbach, J. (2020). An overview of reviews on strategies to reduce health inequalities. International Journal for Equity in Health, 19(1), 1-11. https://doi.org/10.1186/s12939-020-01299-w
Gollust, S., Cunningham, B., Bokhour, B., Gordon, H., Pope, C., & Saha, S. et al. (2018). What causes racial health care disparities? A mixed-methods study reveals variability in how health care providers perceive causal attributions. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 55, 1-11. https://doi.org/10.1177/0046958018762840
Gómez, C., Kleinman, D., Pronk, N., Wrenn Gordon, G., Ochiai, E., & Blakey, C. et al. (2021). Addressing health equity and social determinants of health through healthy people 2030. Journal of Public Health Management and Practice, s249-s257. https://doi.org/10.1097/phh.0000000000001297
Lavizzo-Mourey, R., Besser, R., & Williams, D. (2021). Understanding and mitigating health inequities — past, current, and future directions. New England Journal of Medicine, 384(18), 1681-1684. https://doi.org/10.1056/nejmp2008628
Suarez-Balcazar, Y., Mirza, M., & Garcia-Ramirez, M. (2017). Health disparities: Understanding and promoting healthy communities. Journal of Prevention & Intervention in The Community, 46(1), 1-6. https://doi.org/10.1080/10852352.2018.1386761
Also Read:
BHA FPX 4020 Assessment 3 Data Collection and Analysis
FPX BHA 4020 Assessment 4 Paper
BHA FPX 4020 Assessment 5 Health Care Leadership
BHA FPX 4020 Assessment 1 Health Care Problem Analysis Proposal Instructions
Prepare a health care problem analysis proposal in outline format (3-10 pages) on a current, relevant health care problem. Include the rationale for selecting the problem, a description of the how the problem is assessed and measured for quality improvement purposes, a proposed industry measure of performance, action steps for completing the project, and a description of the applicable leadership competencies.
Effective health care leaders simultaneously maintain internal organizational and external industry environmental awareness. Leaders are challenged to focus on vision, mission, strategic direction, goals, and objectives while remaining mindful of emerging trends that may affect an organization’s viability.
Monitoring the external environment for issues that may represent major challenges to an organization requires ongoing diligence. Health care administrators must identify and prioritize issues affecting their organizations. Furthermore, leaders must select methods and tools with which to analyze data for identification of potential solutions.
In this first assessment in your capstone course, you will have an opportunity to select a health care problem that is relevant to your career interests and one that adds value to a current or future health care organization. By the end of the course, you will be drawing from current scholarly and/or authoritative sources to provide evidence-based recommendations to solve the problem.
Demonstration of Proficiency for BHA FPX 4020 Assessment 1 Health Care Problem Analysis Proposal
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
Competency 1: Evaluate problems in health care organizations, and apply tools to improve quality and outcomes.
Describe, using an authoritative source, how the selected health care problem is assessed and measured for quality improvement purposes. Describe how five American College of Healthcare Executives (ACHE) leadership competencies apply to the selected capstone project topic.
Competency 2: Analyze foundational elements of the U.S. health care system.
Identify a relevant problem along with the rationale for selecting the problem.
Competency 4: Analyze records and reports based on established benchmarks and organizational goals and performance.
Propose an industry measure of performance, such as a benchmark, which pertains to the type of organization selected for problem analysis.
Competency 5: Create comprehensive and useable data-driven actions plans, based on industry benchmarks. Provide a bulleted list of the preliminary action plan steps to review the problem and propose solutions.
Competency 6: Communicate effectively with diverse audiences, in an appropriate form and style, consistent with applicable organizational, professional, and scholarly standards.
Create a clear, well organized, professional, and generally error-free outline that describes a relevant health care problem.
Preparation for BHA FPX 4020 Assessment 1 Health Care Problem Analysis Proposal
To successfully complete this first assessment in your capstone course, you will need to conduct independent research on current, relevant problems facing the U.S. health care system. The problem you select needs to meet all of the following criteria:
- The selected health care problem is likely to affect your current or desired future workplace, such as a hospital, home health care agency, hospice, ambulatory clinic, et
- Authoritative and scholarly health care literature addresses the problem of
- Data is available for the selected
- The current state can be articulated by describing major factors and the way in which these factors are For example, the selected problem can be analyzed by examining such data as average length of stay (in days) and cost (dollars).
You may begin your research on current, relevant problems facing the health care industry by studying your suggested resources for this assessment. In addition, you may want to consult the Health Care Administration Undergraduate Library Research Guide to help you begin your search for scholarly and authoritative sources on significant, contemporary problems in the health care industry.
Please ensure that the problem is relevant and of sufficient interest to your career goals since all future course work is built upon the stated problem.
BHA FPX 4020 Assessment 1 Health Care Problem Analysis Proposal Instructions
For this assessment, you will construct a capstone health care problem analysis proposal on your selected topic. You may wish to envision your current or future workplace as the potential site for presentation of the proposal. After your proposal is constructed, you will receive feedback from your faculty member. Later in the course, in a separate assessment, you will receive feedback from a practicing professional about the proposed approach to analyze data relating to the problem.
The requirement for this assessment is to produce a proposal that has clear section headings and contains a flow of logic. You may opt to use an outline format. Please avoid lengthy narrative paragraphs, as the proposal is intended to be presented in an imaginary workplace. Busy executives will not have time to read paragraphs word for word. Instead, expect that your audience will read the document by scanning.
Your goal is to provide succinct yet substantive information with sufficient depth to cover your selected problem. Remember to include a cover page, table of contents, section headings, and reference list. The length of the proposal is based upon the breadth and depth of your selected topic.
The following general steps in construction of your proposal contain additional specific information requirements.
Step 1: Identify a relevant problem along with the associated rationale for the selection of the problem. Be sure to substantiate content with and authoritative source.
State the problem in a single sentence, tell why it is a problem, and add a citation from a current, authoritative source. For example: Condition X if not addressed may result in Consequence Y (source, year).
Step 2: Describe, using an authoritative source, how the selected health care problem is assessed and measured for quality improvement purposes. Include relevant factors and associated units of measurement.
Select six current authoritative sources that apply to your selected problem. You may consider your problem from an industry, organization, or specific professional level. Be sure to include any industry standards, legal, and ethical considerations that relate to your problem. Summarize each of the six sources in a succinct sentence or two. Explain how each source directly relates to the problem. Be sure to add an APA formatted citation for each.
Step 3: Propose an industry measure of performance, such as a benchmark, which pertains to the type of organization selected for problem analysis.
State the major factors or performance indicators that directly relate to your problem. Assign a unit of measurement to each factor (days, dollars, percentage, et cetera.)
Identify the authoritative source(s) used to determine the major factors you selected that relate to the problem. Identify which industry assessment tool or framework you will use to analyze the problem.
Step 4: Provide a bulleted list of the preliminary action plan steps to complete the capstone health care problem analysis project. Examples include:
conduct library search, formulate problem statement, identify factors and units of measure, and so on.
Step 5: Describe one competency from each of the five American College of Healthcare Executives’ (ACHE) domains that relate to your capstone health care problem analysis proposal.
Review the ACHE competency model:
Healthcare Leadership Alliance and the American College of Healthcare Executives. (2018). ACHE healthcare executive competencies assessment tool. Retrieved from https://www.ache.org/pdf/nonsecure/careers/competencies_booklet.pdf
Provide a short statement about how you practice one competency within each of the five ACHE domains. Consider including a table such as the following within your outline. Note: You have been provided with one example of how you might complete this for one competency within one domain. You will need to complete the entire table—one competency within each of the five domains.
ACHE Domain ACHE Competency Selected How This Competency Relates to the Capstone Health Care Problem Analysis Proposal Communication and Relationship Management Leadership Professionalism Knowledge of the Healthcare EnvironmentHealthcare Systems and OrganizationsI chose health care systems and organizations because the capstone project will require me to develop skills in identifying substantive problems that the health care industry needs to address. It will also require me to develop skills in working to resolve a substantive problem within a health care organization. Business Skills and KnowledgeReminder: You will condense and use the material from your outline in your final PowerPoint presentation in the fourth course assessment.
Additional Requirements for BHA FPX 4020 Assessment 1 Health Care Problem Analysis Proposal
Length: 3 to 10 double-spaced pages. Outline length will vary based on your selected topic.
Font: Use Times New Roman, 12 point font.
APA: Provide a minimum of six APA-formatted citations and references to current, scholarly and/or authoritative sources.
Problem selection criteria: Be sure your selected problem meets all four criteria listed under Preparation.
Writing: Create a clear, well-organized, professional, and generally error-free outline that describes a relevant health care problem
READ MORE >>
BHA FPX 4020 Assessment 3 Data Collection and AnalysisData Collection and Analys ...
BHA FPX 4020 Assessment 3 Data Collection and Analysis
Data Collection and Analysis
Health disparities in the US pose a challenge by compromising the ability to provide timely, affordable, and quality care. According to the Agency for Healthcare Research and Quality (AHRQ) (2021), healthcare disparities entail differences between population groups that determine how they access, experience, and receive healthcare services.
When elaborating on the problem of widening health inequalities, it is essential to incorporate the role of social determinants of health (SDOH) into the discussion. In this sense, synergies between ethnic, socioeconomic, environmental, and locational factors contribute to inequalities regarding access to care, care coordination, perceptions of patient safety, and care affordability.
As a country of demographic and socioeconomic diversities, the US needs to understand the interactions between health disparities. Therefore, data collection and analysis emerge as a profound strategy for enhancing knowledge and inspiring evidence-based practice for addressing health inequalities. As a result, this assessment presents data regarding various health inequalities while proposing evidence-based strategies for addressing health disparities.
Data Presentation
Figure 1: People under age 65 with any period of uninsurance during the year, by race, 2017
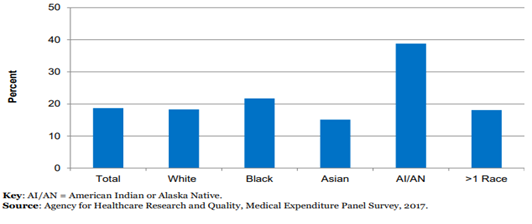
Figure 2: New HIV cases per 100,000 population aged 13 and over, 2008-2016
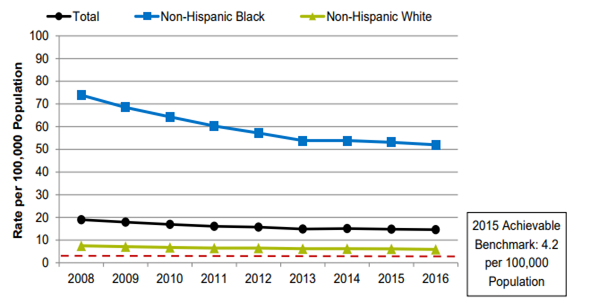
Source: Agency for Healthcare Research and Quality (AHRQ)
Figure 3: People unable to get or delayed in accessing medical care due to financial or insurance reasons, 2002-2017
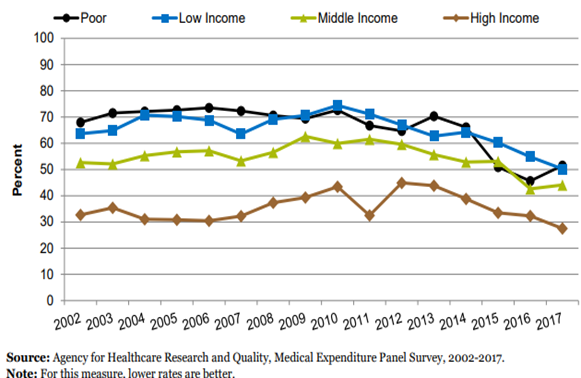
Figure 4: Effects of Medicaid Expansion on States’ Healthcare Expenditures
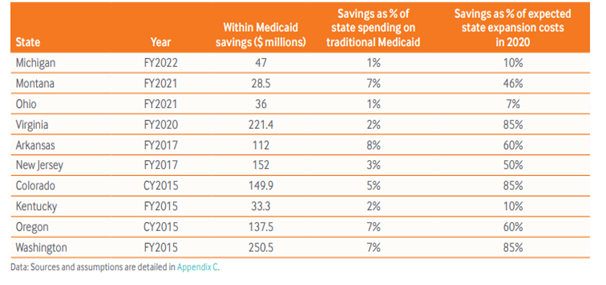
Source: The Commonwealth Fund
Quantitative and Qualitative Analysis of Data
As noted earlier, health disparities influence how people access, experience, and receive healthcare services. In the United States, health inequalities manifest via various domains, including access to person-centered care, patient safety, healthy living, effective treatment, care coordination, and care affordability (Agency for Healthcare Research and Quality, 2021).
In this sense, national and state health organizations set achievable benchmarks based on concepts from each domain. For example, organizations emphasize adverse drug events in patients with anticoagulants, urinary tract infections, and medication safety when establishing patient safety benchmarks. These sub-themes enable healthcare institutions to compare their performance with top-performing institutions.
Since health inequalities are diverse and beyond one measure of quality, it is essential to focus on areas that demonstrate widening gaps within the social determinants of health (SDOH). In this sense, analyzing quantitative and qualitative data from national healthcare organizations such as the Agency for Healthcare Research and Quality (AHRQ) is essential to identify priority areas that demonstrate significant inequalities.
The first graph represents quantitative data regarding the problem of uninsured people under the age of 65 years. The graph makes it possible to identify disparities in access to insurance coverage among people of different ethnic backgrounds, including White, Black Americans, Asian Americans, American Indians or Alaska Natives (AI/AN), and people of more than one race.
The graph indicates that in 2017, (AI/ANs) under age 65 were twice as likely to lack insurance as whites (38.8% compared with 18.3%). Also, Black Americans were more likely than Whites to have a period of uninsurance in 2017 (21.7% compared with 18.3%). While health disparities hamper access to insurance coverage for ethnic groups, this data from the Agency for Healthcare Research and Quality (AHRQ) can inform recommendations for addressing health inequalities within the national insurance models.
Another ideal measure of health disparities is the prevalence of new HIV cases among people aged 13 and above. In Figure 2, the Agency for Healthcare Research and Quality (AHRQ) (2021) indicates the inequalities regarding new HIV cases in 2016. The graph indicates that non-Hispanic Blacks reported 52.0 new HIV cases per 100000 population for people aged 13 and above compared with 5.9 per 100000 cases for non-Hispanic Whites.
Although these numbers did not match the 2015 national achievable benchmark of 4.2 cases per 100000 population, they signify underlying conditions that create imbalances in the quality of life across the two groups. Therefore, the data shed light on areas where the federal and state governments should improve to reduce health inequalities.
Apart from the prevalence of new HIV cases and the number of uninsured people across populations, income issues are essential determinants of health disparities. In Figure 3, it is evident that poor and low-income people grapple with the problem of delayed care compared to middle-and-high-income people.
The graph indicates that 51.5% of the poor faced the challenge of delayed care in 2017 due to financial or insurance reasons. Although the income disparities narrowed from 2002 to 2017, poor and low-income people endure delayed care due to financial or insurance reasons. Therefore, national and state governments can use such data to initiate programs to reduce income inequality.
Evidence-Based Recommendations
Healthcare organizations in the US operate to promote care quality, timeliness, equality, and affordability. However, the prevailing health disparities affect how people access, experience, and receive healthcare services. In the current healthcare systems, external evidence significantly influences organizations’ practices and informs clinical decisions. While health inequalities rely massively on discrepancies within the social determinants of health (SDOH), it is vital to implement recommendations from reputable sources to address these disparities. These recommendations include:
Medicaid Expansion
The United States lacks a universal insurance model for providing health coverage to vulnerable groups. The absence of universal public insurance coverage exacerbates the problem of uninsured people, leading to expensive insurance premiums and complex health reimbursement models.
According to Radley et al. (2021), nearly 30 million Americans are still uninsured and are disproportionately people of color. Although the Affordable Care Act (ACA) 2010 required states to expand Medicaid, the revised eligibility criteria exclude poor and low-income people. As a result, they are ineligible for Medicaid coverage, leading to multiple ramifications, including limited access to quality care, the problem of delayed care due to financial or insurance issues, and compromised quality of life.
Although Medicaid expansion is an ideal strategy for addressing income-related health disparities, it is essential to establish its cost-benefit analysis to ensure its economic plausibility. Since Medicaid is a federal insurance policy, its expansion can alter national healthcare expenditures. However, states are more likely to save the cost of healthcare outside Medicaid services.
Ward (2020) argues that Medicaid expansion reduces states’ spending in various areas, including mental health and substance abuse treatment, corrections, and uncompensated care. The qualitative data in Figure 4 present savings estimates from traditional Medicaid and Medicaid expansion for selected states in different fiscal years. It is vivid that expanding Medicaid addresses disparities in access to quality care, care affordability, coordination, and patient safety.
Developing Community-Based Programs and Policies for Ensuring Health Equality
Medicaid expansion cannot singlehandedly address the prevailing health inequalities. Instead, health organizations and governmental agencies should embrace interdisciplinary collaboration to support community-based initiatives tackling health inequalities. According to Gomez et al. (2020), these localized programs should focus on various social determinants of health, including education, housing, healthcare justice, and literacy.
Also, they should compromise sub-themes such as attending to root causes of health inequalities and disparities, addressing issues that affect susceptible groups, promoting equal opportunities for all people to guarantee improved quality of life, and fair distribution of socioeconomic resources to promote healthy living.
Eliminating Structural Racism in Healthcare Organizations
Organizational cultures are consistent with patient safety, coordination, and patient-centered care. According to Lavizzo-Mourey et al. (2021), racial and ethnic disparities in healthcare organizations exist and are disproportionate to minority groups such as Black Americans and Asian Americans.
Such inequalities result in adverse health effects by compromising the tenets of patient-centered care, patient safety, and positive medical outcomes. As a result, addressing the underlying organizational barriers to equal healthcare service delivery is a profound strategy for tackling health discrepancies at the organizational level.
Conclusion
Undoubtedly, health inequalities and disparities cut across various domains, including access to person-centered care, patient safety, coordination, affordability, and effective treatment. Since the US grapples with social determinants of health discrepancies, it is essential to incorporate evidence-based strategies from quantitative and qualitative data regarding measures of health inequalities.
Figures 1, 2, and 3 present insights on various health discrepancies prevailing among ethnic and socioeconomic groups. Therefore, national and state governments should use such data to formulate policies and programs addressing health disparities. Evidence-based recommendations are Medicaid expansion, implementing community-based interventions to ensure equality, and eliminating structural racism in healthcare settings.
References
Agency for Healthcare Research and Quality. (2021). National Healthcare Quality and Disparities Report (pp. 1-316). AHRQ. https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2021qdr.pdf
Gómez, C., Kleinman, D., Pronk, N., Wrenn Gordon, G., Ochiai, E., & Blakey, C. et al. (2021). Addressing health equity and social determinants of health through Healthy People 2030. Journal of Public Health Management and Practice, s249-s257. https://doi.org/10.1097/phh.0000000000001297
Lavizzo-Mourey, R., Besser, R., & Williams, D. (2021). Understanding and mitigating health inequities — past, current, and future directions. New England Journal of Medicine, 384(18), 1681-1684. https://doi.org/10.1056/nejmp2008628
Radley, D., Baumgartner, J., Collins, S., Zephyrin, L., & Schneider, E. (2021). Achieving racial and ethnic equity in US health care: A scorecard of state performance. Accessed 5th February 2022 from https://www.commonwealthfund.org/publications/scorecard/2021/nov/achieving-racial-ethnic-equity-us-health-care-state-performance.
Ward, B. (2020). The impact of Medicaid expansion on states’ budgets. Accessed 5th February 2022 from https://www.commonwealthfund.org/publications/issue-briefs/2020/may/impact-medicaid-expansion-states-budgets.
BHA FPX 4020 Assessment 3
Apply a selected tool to an identified health care problem, analyze the qualitative and quantitative results, and provide evidence-based recommendations to address the problem based on analyses performed. Include a minimum of two visual data displays (charts, graphs, et cetera).
Health care has become a data-driven industry that practices evidence-based decision making. Whether the issue is clinical or financial, health care leaders are expected to analyze problems using logic, established tools, and data. Effective leaders engage team members in the problem resolution process, encouraging a wide variety of perspectives. Once the problem is clearly defined, the health care leader is responsible for selecting an appropriate, established framework or tool with which to analyze the problem. Research, critical thinking, and team collaboration are important facets of problem solving.
Health care organizations have finite resources, so the solving of problems must take place within the confines of the organization’s available resources. In this assessment you will practice estimating the cost of one recommendation and determining whether implementing the recommendation is realistic for a specific health care organization. You will apply a simple cost benefit analysis and make a recommendation. Cost benefit analysis is another important skill for health care leaders, and this assessment provides an opportunity for you to demonstrate critical thinking skills.
This assessment also provides the opportunity to reflect upon the industry and organizational contexts before engaging in application of a tool for problem analysis. You will consider the organization’s setting with respect to level of care, mission, strategy, operations, and culture. Moreover, you will think critically about legal, regulatory, ethical, and risk management operational issues that relate to the selected problem. Let’s get started.
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate proficiency in the course competencies through the following assessment scoring guide criteria:
Competency 1: Evaluate problems in health care organizations, and apply tools to improve quality and outcomes.
Provide rationale for the selected problem analysis model or tool.
Competency 3: Construct evidence-based health care management recommendations in compliance with personal and professional values and legal, regulatory, and ethical considerations.
Construct evidence based recommendations which may include ethical, legal, regulatory, and organizational standards.
Competency 4: Analyze records and reports based on established benchmarks and organizational goals and performance.
Analyze date relative to internal and external benchmarks.
Preparation for BHA FPX 4020 Assessment 3
As you prepare to complete this third course assessment, consider the organizational context. How does analysis of the problem align with the organization’s vision, mission, strategy and financial viability? Using numbers and organizational considerations, you will explain why the organization should or should not proceed with the recommendation.
Assessment 3 Instructions
This assessment consists of three parts.
Data Presentation
In this part of the assessment, you will apply the selected tool to the problem and produce a minimum of two visual data displays (charts, graphs, et cetera). Examples of tools you might include are:
Cost Benefit Analysis: Excel spreadsheet, converted into 2–3 worksheet tabs, graphs, or other visual display format. Compliance Assessment: 3 major criteria converted into 3 separate pie charts or other graphic display format.
Lean Analysis: The percent of variance by major factor converted into 2–3 trend lines.
Note: At a minimum, provide a cost benefit analysis of the recommendation.
Quantitative and Qualitative Analysis of Data
In this part of the assessment you will analyze the collected data relative to benchmarks. Provide discussion as to whether the selected benchmarks are internal to the organization, external industry benchmarks, or a combination. Be sure to include a short summary of observations. Note: If the problem requires an additional tool, such as a compliance audit tool, you may include more than one discussion of the results.
Evidence-Based Recommendations
In this final part of the assessment, provide evidence-based recommendations that will help to address the identified problem. Be sure to support your recommendations with references to current, scholarly, and/or authoritative sources. Also include an explanation as to why the recommendations are feasible for this particular organization. For example, one recommendation might be to offer a new service line. Even though the new service may not generate an immediate profit, it might serve to draw additional patients into the network.
Additional Requirements
Length: The nature, breadth, and depth of the problem will drive the length of the recommendation and cost benefit analysis.
Font: Use Times New Roman, 12-point font.
APA: Follow APA formatting and style guidelines for citations and references
Related Assignments:
BHA-FPX 4020 Assessment 5 Instructions: Health Care Leadership Self-Assessment
READ MORE >>
BHA FPX 4020 Assessment 5 Health Care LeadershipComplete a self-assessment of 25 ...
BHA FPX 4020 Assessment 5 Health Care Leadership
Complete a self-assessment of 25 ACHE leadership competencies. Prepare a personal development plan that identifies specific action steps and due dates for improvement of five selected leadership competencies.
Throughout their careers, health care leaders must regularly assess their individual competencies and how those competencies align with organizational needs and priorities. Changing laws, regulations, technology, consumer preferences, medical treatment advances, and external environmental shifts can affect the skill sets needed for effective leadership. Accurate self-assessment is an important first step in identification of areas for future leadership development.
In this assessment, you will reflect upon your performance with respect to the industry-validated ACHE leadership competency model. After identifying areas of strength and areas for development, you can craft specific action steps to address any leadership development gaps.
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
Competency 4: Analyze records and reports based on established benchmarks and organizational goals and performance.
Identify five individual competencies within each of the five ACHE model domains practiced during the capstone project.
Estimate baseline competency performance ratings at the beginning of the BHA program on the 25 identified individual competencies. Assess current competency performance ratings for the capstone project on the 25 identified individual competencies.
Competency 5: Create comprehensive and useable data-driven action plans, based on industry benchmarks.
Identify one competency within each of the five ACHE domains for further development.
Create one specific action step with a due date to strengthen competency performance for each of the five development areas identified.
Preparation
To successfully prepare to complete this final course assessment, you will need to review the ACHE competency model:
Healthcare Leadership Alliance and the American College of Healthcare Executives. (2018). ACHE healthcare executive competencies assessment tool. Retrieved from https://www.ache.org/pdf/nonsecure/careers/competencies_booklet.pdf
Remember that you already examined this tool in Assessment 1 and identified one competency from each domain that you would be practicing while completing the capstone project.
BHA FPX 4020 Assessment 5 Health Care Leadership Instructions
This assessment is in two parts:
Part 1: Leadership Self-Assessment.
You will assess the development of your leadership skills over the course of your BHA program.
Part 2: Personal Development Plan.
You will identify measurable action steps for future career development based on the results of your leadership skills assessment.
Part 1: Leadership Self-Assessment
To complete your leadership self-assessment:
Download the Leadership Self-Assessment Template [DOCX].
Select five competencies from each of the five ACHE leadership domains (25 total competencies) that you practiced during your capstone project and enter them into the appropriate space on the template (Column 2).
Estimate your performance at the beginning of your BHA program on each of the 25 competencies you selected. The rating scale is from 1 (novice) to 5 (expert).
Enter this information on Column 3 of the template.
Early careerists typically score in the novice to competent performance levels. Occasionally they may rate in the expert category. The faculty member will be emphasizing rating accuracy rather than how high the ratings are.
Assess your performance after completing your capstone project on each of the selected 25 competencies.
Enter this information in Column 4 on the template.
Summarize your insights about strengths and improvement areas in the space provided.
Part 2: Personal Development Plan
To complete the personal development plan part of this assessment:
Download the Personal Development Plan Template [DOCX].
Select from your leadership self-assessment five competencies (one from each of the five domains) for further development and cultivation of your health care leadership skills. Enter these competencies into Column 2 of the template.
Determine one specific, measurable action step for each of the five selected competencies that will promote skill development. Enter the actions steps in Column 3 of the template.
People learn the most from having the opportunity to practice and demonstrate their skills. Although courses and readings certainly have value for personal development, consider other ways to cultivate the selected competencies. For example, obtain a mentor, solicit feedback from a more experienced colleague, join a professional organization, or volunteer your services.
Assign due dates for completing each action step. Enter the due dates in Column 4 of the template.
Templates: Use the templates provided to complete your leadership self-assessment and your personal development plan.
Portfolio Prompt: You may choose to save this learning activity to your ePortfolio. Consult this resource for additional information about adding artifacts to your ePortfolio.
Leadership Self-Assessment Template Example
Refer to the ACHE Healthcare Executive Competencies Assessment Tool to select the applicable competencies.
ACHE DomainIdentified Competency (Choose 5 for each domain that you practiced during your capstone project)Rating at the beginning of BHA Program1 (novice) to 5 (expert)Rating during Capstone Project1 (novice) to 5 (expert)Communication and Relationship ManagementPrinciples of communication and their specific applications25 Communicating organizational mission, vision, objectives, and priorities14 Preparing and delivering business/organizational communication, including meeting agendas, presentations, reports, and project communication plans14 Providing and receiving constructive feedback25 Using factual data to produce and deliver credible and understandable reports13LeadershipChange Management and promotion14 Explore opportunities for growth and organizational development continuously14 Promote continuous organizational learning/improvement25 Anticipate and plan strategies for overcoming obstacles13 Develop effective medical staff relationships in support of the organization’s mission, vision, and strategic plan25ProfessionalismProfessional roles, responsibility, and accountability24 Understanding organizational business and personal ethics25 Balancing professional and personal pursuits13 Understanding cultural and spiritual diversity for patients and staff as they relate to healthcare needs24 Uphold and act upon ethical and professional standards25Knowledge of the Healthcare EnvironmentKnowledge of healthcare systems and organizations24 Healthcare and medical terminology15 Managed care models, structures, and environment14 Evidence-based management practice24 Healthcare economics13Business Skills and KnowledgeQuality Improvement25 Benchmarking techniques24 Quality improvement theories and frameworks24 National quality initiatives, including patient safety25 Data collection, measurement, and analysis13Summarize insights regarding strengths and areas for improvement as you continue your health care administration career:
Based on the leadership self-assessment template, it is valid to argue that the capstone project has bolstered various competencies across the five American College of Healthcare Executives (ACHE) domains. Under the communication and relationship management domain, the capstone project developed my communication skills by enhancing my understanding of communication principles and their specific applications, the ability to communicate institutional/team mission, vision, and objectives, and the ability to present agendas and reports, and project plans.
Also, it bolstered my capacity to provide and receive constructive feedback from colleagues regarding organizational objectives and priorities. However, I must improve on using factual data to produce and deliver credible and understandable reports.
Secondly, the capstone project has enhanced my competencies for promoting and managing change. In this sense, I am now aware of strategies for exploring organizational growth and development opportunities, anticipating and planning strategies for overcoming obstacles, and promoting continuous organizational learning or improvement.
Also, the project has transformed my ability to develop effective medical staff relationships in support of the organizational mission, vision, and strategic plans. However, it is essential to embrace strategies for personal development regarding the ability to anticipate and plan strategies for overcoming barriers to effective change implementation. In this sense, I need the implement action step for further development in areas such as change advocacy, analysis of the underlying impediments to quality improvement, and effective ways for championing change.
Thirdly, the capstone project bolstered various competencies under the professionalism domain. For instance, I have developed awareness of patient rights and responsibilities, corporate business and personal ethics, patients’ and staff’s cultural and spiritual diversity, and strategies for upholding and acting upon ethical and professional standards.
It is valid to argue that the capstone project has enabled me to understand thresholds for ethical and professional standards that guide nursing practices. However, I still face challenges when establishing approaches for balancing professional and personal pursuits. Often, I emphasize personal aspirations at the expense of professional roles. Therefore, I need to develop competencies to balance professional issues and personal aspirations and pursuits.
Fourthly, the capstone project has positively impacted my knowledge of healthcare systems and organizations. At the beginning of the Bachelor’s of Health Administration (BHA) program, I was a novice in various aspects, including healthcare and medical terminologies, managed care models, structures, and environment, evidence-based management practice, and healthcare economics. However, the program enhanced my competencies regarding these topics. Although knowledge of healthcare systems and organizations is one of my strengths, I need to embrace strategies for personal development regarding healthcare economics.
Finally, the BHA program has improved my business skills and knowledge. For instance, I am now aware of benchmarking techniques, national quality initiatives, clinical methodologies, quality improvement theories and frameworks, and data collection, measurement, and analysis tools/techniques. At the beginning of this program, I was a novice in various quality improvement techniques in different healthcare settings.
However, I had become competent by the time of completing my capstone project. Although I am competent in quality improvement, I should emphasize interventions for developing my data collection, measurement, and analysis competencies. In this sense, I am yet to become an expert in data collection, measurement, and analysis.
References
Healthcare Leadership Alliance and the American College of Healthcare Executives. (2018). ACHE healthcare executive competencies assessment tool. Retrieved from https://www.ache.org/pdf/nonsecure/careers/competencies_booklet.pdf
Personal Development Plan
From your Leadership Self-Assessment, identify five competencies (one from each domain) that you would like to develop further. Identify an appropriate action step with a due date for each competency.
ACHE DomainCompetency for Further Development (Choose 1 for each domain from your Leadership Self-AssessmentAction StepDue DateCommunication and Relationship ManagementUsing factual data and delivering credible and understandable reports· Develop a culture of inquiry to embrace evidence-based practice and improve skills for nursing research
· Obtain a mentor and solicit feedback from more experienced colleagues regarding effective selecting and appraising evidence sources.
· Volunteer to a professional organization specializing in nursing research methods and information dissemination.
By the end of 2022LeadershipAnticipate and plan strategies for overcoming obstacles to change management and promotion· Develop listening and communication skills to understand colleagues’ views and feedback regarding the change process.
· Leverage data to convince my colleagues to accept change and implement its provisions.
· Review and understand various change theories and frameworks
By June 2022ProfessionalismBalancing professional and personal pursuits· Developing time management skills by setting priorities and timely planning
· Proper scheduling
· Regularly reviewing workloads
· Encouraging social activities to facilitate recreation and reduce burnout
ContinuousKnowledge of the Healthcare EnvironmentHealthcare economics· Soliciting feedback from more experienced colleagues
· Enrolling in part-time learning programs regarding health economics
· Obtaining a mentor to offer guidance and insights into various aspects of healthcare economics
By December 2022Business Skills and KnowledgeData collection, measurement, and analysis· Use internet-based databases, books, and other evidence sources to learn about effective methods for data collection, measurement, and analysis
· Enroll in part-time learning programs for data collection, measurement, and analysis
· Obtain a mentor and engage more experienced colleagues to obtain insights into data collection, measurement, and analysis methods.
By mid-2023Related Assignments:
BHA-FPX4020 Assessment 1: Health Care Problem Analysis Proposal
BHA-FPX 4020 Assessment 3: Data Collection and Analysis
BHA-FPX 4020 Assessment 4: Interdisciplinary Presentation of Evidence-Based Recommendations
READ MORE >>
measurable action step for each of the five selected competencies that will pro ...
People learn the most from having the opportunity to practice and demonstrate their skills. Although courses and readings certainly have value for personal development
READ MORE >>
BHA FPX4020 Assessment Papers – Healthcare Problem Analysis Proposal Example ...
BHA FPX4020 Assessment Papers – Healthcare Problem Analysis Proposal Example Solution
Healthcare systems in the US bear the obligation to achieve a triad objective of improving the patient experience of care, including quality and satisfaction, improving public health services, and reducing the cost of care. Despite these considerations, Americans do not receive quality, timely, and affordable care due to the prevailing healthcare disparities. According to the Agency for Healthcare Research and Quality (AHRQ) (2021), a healthcare disparity is a “difference between population groups in the way they access, experience, and receive healthcare” (p. 193).
In this sense, the synergies between ethnic, social, economic, environmental, and geographical factors contribute to inequalities regarding access to care, experiences, and quality of life. Although the country enacts policies that ensure affordability, accessibility, and equality, eliminating ethnic and socio-economic disparities poses a public health challenge. Therefore, this proposal elaborates on strategies for measuring and assessing healthcare disparities, quality benchmarks, and evidence-based strategies for addressing the problem.
Measurements and Assessment of the Problem
It is possible to measure and assess the problem of healthcare disparities by evaluating interactions between health and social determinants of health (SDOH), including age, education, neighborhood, employment, and population’s income levels. Also, it is essential to incorporate ethnic aspects because they influence access to quality care, experiences, and quality of life. The Agency for Healthcare Research and Quality (AHRQ) (2021) presents six profound domains for assessing disparities. These considerations are:
- Access to person-centered care
- Patient Safety
- Care coordination
- Care affordability
- Effective treatment
- Healthy living
Benchmarks for Healthcare Disparities
Often, it is possible to determine the prevailing health disparities by comparing the community’s performance against top-performing communities and state or national benchmarks. As noted earlier, it is vital to assess and measure health disparities by evaluating inequalities within the six domains, including access to patient-centered care, the level of care coordination, care affordability, the availability of effective treatment, and healthy living.
Gomez et al. (2021) argue that conditions in which people live, learn, work, and worship, alongside their age and growth patterns, influence well-being outcomes, quality of life, and access to timely, affordability, and quality care. Therefore, the social determinants of health (SDOH) are the causative and contributing factors for health disparities.
The Agency for Healthcare Research and Quality (AHRQ) collaborates with other agencies, such as the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services (CMS), to document national and state benchmarks for the six domains. In this sense, it is possible to gauge communities’ performance regarding eliminating healthcare disparities by comparing their prevalence with states’ and national benchmarks.
One of the most profound benchmarks for healthcare disparities is the number of uninsured people of ethnic diversities. Carratala and Maxwell (2020) argue that about 10.6% of African Americans were uninsured compared with 5.9% of non-Hispanic Whites in 2017. Such statistics indicate ethnicity is a profound cause of disparities in care affordability and accessibility.
The stand unit for measuring health disparities entails often computing the total number of individuals with distinct characteristics against a predetermined population (1000, 100000, and so on). For example, healthcare professionals can calculate the total number of Black Americans with new cases of HIV by identifying the number of new cases per 100,000 people. Consequently, it is possible to compare the prevalence of disparities with achievable benchmarks.
Action Plan
Many scholarly and authoritative sources proposed evidence-based interventions for analyzing and addressing health disparities in patient safety, access to quality care, care affordability, quality of life, and care coordination. These interventions include:
- Identifying and addressing contextual issues contributing to healthcare disparities (Suarez-Balcazar et al., 2017). it is essential to understand the linkage between social determinants of health (SDOH) and access to care, affordability, care coordination, and quality of life.
- Initiating organizational, provider-focused, and systematic changes to reduce racial healthcare disparities (Gullost et al., 2018).
- Eliminating structural racism in healthcare organizations to promote fairness and equality at the institutional level (Lavizzo-Mourey et al., 2021)
- Ensuring equality when distributing socio-economic resources reduces disparities within the social determinants of health, such as housing, health literacy, work conditions, and employment status (Gomez et al., 2021).
- Implementing transformative care delivery and financial arrangements to transform healthcare reimbursement strategies, including national insurance models to enhance accessibility and affordability (Garzon-Orjuela et al., 2020).
American College of Healthcare Executives (ACHE) Leadership Competencies
ACHE DomainACHE Competency SelectedHow This Competency Related to the Capstone Health Care Problem Analysis ProposalCommunication and Relationship ManagementCommunication SkillsCommunication competencies are prerequisites for effectively disseminating information and evidence regarding clinical problems as a healthcare professional. According to the American College of Healthcare Executives (ACHE) (2020), communication skills enhance an individual’s ability to communicate clearly and concisely with internal and external audiences, establish and maintain relationships, and facilitate constructive interactions with team members. This competency is consistent with the capstone project analysis because it entails implementing interdisciplinary teams for change.LeadershipManaging ChangeUndoubtedly, understanding the change process is essential for inspiring evidence-based interventions to address health disparities. ACHE (2020) contends that effective leadership entails inspiring individuals and organizational excellence by creating a shared vision and successfully managing change. Therefore, this competency complements the need to initiate, implement, and sustain approaches for addressing health disparities.ProfessionalismPersonal and Professional AccountabilityAs noted earlier, it is essential to eliminate structural discrimination in healthcare organizations to address health disparities such as access to quality care for disadvantaged patient populations, care coordination issues, and patient safety concerns (Lavizzo-Mourey et al., 2021). Personal and professional accountability is a prerequisite for ensuring equality at the institutional level because it aligns with ethical and professional standards. This competency relates to the capstone healthcare problem because it requires healthcare professionals to uphold ethical and professional practice standards, eliminating structural disparities such as discrimination.Knowledge of the Healthcare EnvironmentalHealthcare Systems and OrganizationsThe problem of health disparities prompts healthcare professionals and policymakers to understand the synergies between social determinants of health (SDOH) and domains of quality care, including accessible, affordable, and coordinated care. Therefore, it is essential to understand external and internal organizational environments, including healthcare delivery systems like insurance and reimbursement models. Therefore, this competency aligns with the capstone healthcare problem because it emphasizes understanding care dynamics and their contribution to health disparities.Business Skills and KnowledgeQuality ImprovementQuality improvement is an essential concept in the current healthcare systems because it emphasizes interventions for bolstering care quality, accessibility, and affordability alongside other dimensions of quality care. Healthcare professionals should familiarize themselves with implementing evidence-based recommendations for clinical problems. This competency aligns with the capstone healthcare problem analysis because it entails understanding organizational capacity and aspects that improve dimensions of quality care.References
Agency for Healthcare Research and Quality. (2021). National healthcare quality and disparities report (pp. 1-316). AHRQ. https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2021qdr.pdf
American College of Healthcare Executives. (2020). ACHE healthcare executive: 2020 competencies assessment tool. https://www.ache.org/-/media/ache/career-resource-center/competencies_booklet.pdf.
Carratala, S., & Maxwell, C. (2020). Health disparities by race and ethnicity. https://www.americanprogress.org/article/health-disparities-race-ethnicity/
Garzón-Orjuela, N., Samacá-Samacá, D., Luque Angulo, S., Mendes Abdala, C., Reveiz, L., & Eslava-Schmalbach, J. (2020). An overview of reviews on strategies to reduce health inequalities. International Journal for Equity in Health, 19(1), 1-11. https://doi.org/10.1186/s12939-020-01299-w
Gollust, S., Cunningham, B., Bokhour, B., Gordon, H., Pope, C., & Saha, S. et al. (2018). What causes racial health care disparities? A mixed-methods study reveals variability in how healthcare providers perceive causal attributions. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 55, 1–11. https://doi.org/10.1177/0046958018762840
Gómez, C., Kleinman, D., Pronk, N., Wrenn Gordon, G., Ochiai, E., & Blakey, C. et al. (2021). Addressing health equity and social determinants of health through Healthy People 2030. Journal of Public Health Management and Practice, s249-s257. https://doi.org/10.1097/phh.0000000000001297
Lavizzo-Mourey, R., Besser, R., & Williams, D. (2021). Understanding and mitigating health inequities — past, current, and future directions. New England Journal of Medicine, 384(18), 1681-1684. https://doi.org/10.1056/nejmp2008628
Suarez-Balcazar, Y., Mirza, M., & Garcia-Ramirez, M. (2017). Health disparities: Understanding and promoting healthy communities. Journal of Prevention & Intervention in The Community, 46(1), 1-6. https://doi.org/10.1080/10852352.2018.1386761
BHA FPX4020 Assessment 1 Instructions : Health Care Problem Analysis Proposal
Prepare a health care problem analysis proposal in outline format (3-10 pages) on a current, relevant health care problem. Include the rationale for selecting the problem, a description of the how the problem is assessed and measured for quality improvement purposes, a proposed industry measure of performance, action steps for completing the project, and a description of the applicable leadership competencies.
Effective health care leaders simultaneously maintain internal organizational and external industry environmental awareness. Leaders are challenged to focus on vision, mission, strategic direction, goals, and objectives while remaining mindful of emerging trends that may affect an organization’s viability.
Monitoring the external environment for issues that may represent major challenges to an organization requires ongoing diligence. Health care administrators must identify and prioritize issues affecting their organizations. Furthermore, leaders must select methods and tools with which to analyze data for identification of potential solutions.
In this first assessment in your capstone course, you will have an opportunity to select a health care problem that is relevant to your career interests and one that adds value to a current or future health care organization. By the end of the course, you will be drawing from current scholarly and/or authoritative sources to provide evidence-based recommendations to solve the problem.
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
Competency 1: Evaluate problems in health care organizations, and apply tools to improve quality and outcomes.
Describe, using an authoritative source, how the selected health care problem is assessed and measured for quality improvement purposes. Describe how five American College of Healthcare Executives (ACHE) leadership competencies apply to the selected capstone project topic.
Competency 2: Analyze foundational elements of the U.S. health care system.
Identify a relevant problem along with the rationale for selecting the problem.
Competency 4: Analyze records and reports based on established benchmarks and organizational goals and performance.
Propose an industry measure of performance, such as a benchmark, which pertains to the type of organization selected for problem analysis.
Competency 5: Create comprehensive and useable data-driven actions plans, based on industry benchmarks. Provide a bulleted list of the preliminary action plan steps to review the problem and propose solutions.
Competency 6: Communicate effectively with diverse audiences, in an appropriate form and style, consistent with applicable organizational, professional, and scholarly standards.
Create a clear, well organized, professional, and generally error-free outline that describes a relevant health care problem.
Preparation
To successfully complete this first assessment in your capstone course, you will need to conduct independent research on current, relevant problems facing the U.S. health care system. The problem you select needs to meet all of the following criteria:
- The selected health care problem is likely to affect your current or desired future workplace, such as a hospital, home health care agency, hospice, ambulatory clinic, et
- Authoritative and scholarly health care literature addresses the problem of
- Data is available for the selected
- The current state can be articulated by describing major factors and the way in which these factors are For example, the selected problem can be analyzed by examining such data as average length of stay (in days) and cost (dollars).
BHA FPX 4020 Assessment 1 Instructions: Health Care Problem Analysis Proposal
You may begin your research on current, relevant problems facing the health care industry by studying your suggested resources for this assessment. In addition, you may want to consult the Health Care Administration Undergraduate Library Research Guide to help you begin your search for scholarly and authoritative sources on significant, contemporary problems in the health care industry.
Please ensure that the problem is relevant and of sufficient interest to your career goals since all future course work is built upon the stated problem.
Instructions
For this assessment, you will construct a capstone health care problem analysis proposal on your selected topic. You may wish to envision your current or future workplace as the potential site for presentation of the proposal. After your proposal is constructed, you will receive feedback from your faculty member. Later in the course, in a separate assessment, you will receive feedback from a practicing professional about the proposed approach to analyze data relating to the problem.
The requirement for this assessment is to produce a proposal that has clear section headings and contains a flow of logic. You may opt to use an outline format. Please avoid lengthy narrative paragraphs, as the proposal is intended to be presented in an imaginary workplace. Busy executives will not have time to read paragraphs word for word. Instead, expect that your audience will read the document by scanning. Your goal is to provide succinct yet substantive information with sufficient depth to cover your selected problem. Remember to include a cover page, table of contents, section headings, and reference list. The length of the proposal is based upon the breadth and depth of your selected topic.
The following general steps in construction of your proposal contain additional specific information requirements.
Step 1: Identify a relevant problem along with the associated rationale for the selection of the problem. Be sure to substantiate content with and authoritative source.
State the problem in a single sentence, tell why it is a problem, and add a citation from a current, authoritative source. For example: Condition X if not addressed may result in Consequence Y (source, year).
Step 2: Describe, using an authoritative source, how the selected health care problem is assessed and measured for quality improvement purposes. Include relevant factors and associated units of measurement.
Select six current authoritative sources that apply to your selected problem. You may consider your problem from an industry, organization, or
specific professional level. Be sure to include any industry standards, legal, and ethical considerations that relate to your problem. Summarize each of the six sources in a succinct sentence or two. Explain how each source directly relates to the problem. Be sure to add an APA formatted citation for each.
Step 3: Propose an industry measure of performance, such as a benchmark, which pertains to the type of organization selected for problem analysis.
State the major factors or performance indicators that directly relate to your problem. Assign a unit of measurement to each factor (days, dollars, percentage, et cetera.)
Identify the authoritative source(s) used to determine the major factors you selected that relate to the problem. Identify which industry assessment tool or framework you will use to analyze the problem.
Step 4: Provide a bulleted list of the preliminary action plan steps to complete the capstone health care problem analysis project. Examples include:
conduct library search, formulate problem statement, identify factors and units of measure, and so on.
Step 5: Describe one competency from each of the five American College of Healthcare Executives’ (ACHE) domains that relate to your capstone health care problem analysis proposal.
Review the ACHE competency model:
Healthcare Leadership Alliance and the American College of Healthcare Executives. (2018). ACHE healthcare executive competencies assessment tool. Retrieved from https://www.ache.org/pdf/nonsecure/careers/competencies_booklet.pdf
Provide a short statement about how you practice one competency within each of the five ACHE domains. Consider including a table such as the following within your outline. Note: You have been provided with one example of how you might complete this for one competency within one domain. You will need to complete the entire table—one competency within each of the five domains.
ACHE DomainACHE Competency SelectedHow This Competency Relates to the Capstone Health Care Problem Analysis ProposalCommunication and Relationship ManagementLeadershipProfessionalismKnowledge of the Healthcare EnvironmentHealthcare Systems and OrganizationsI chose health care systems and organizations because the capstone project will require me to develop skills in identifying substantive problems that the health care industry needs to address. It will also require me to develop skills in working to resolve a substantive problem within a health care organization.Business Skills and KnowledgeBHA FPX4020 Assessment 3 Instructions: Data Collection and Analysis
Apply a selected tool to an identified health care problem, analyze the qualitative and quantitative results, and provide evidence-based recommendations to address the problem based on analyses performed. Include a minimum of two visual data displays (charts, graphs, et cetera).
Health care has become a data-driven industry that practices evidence-based decision making. Whether the issue is clinical or financial, health care leaders are expected to analyze problems using logic, established tools, and data. Effective leaders engage team members in the problem resolution process, encouraging a wide variety of perspectives. Once the problem is clearly defined, the health care leader is responsible for selecting an appropriate, established framework or tool with which to analyze the problem. Research, critical thinking, and team collaboration are important facets of problem solving.
Health care organizations have finite resources, so the solving of problems must take place within the confines of the organization’s available resources. In this assessment you will practice estimating the cost of one recommendation and determining whether implementing the recommendation is realistic for a specific health care organization. You will apply a simple cost benefit analysis and make a recommendation. Cost benefit analysis is another important skill for health care leaders, and this assessment provides an opportunity for you to demonstrate critical thinking skills.
This assessment also provides the opportunity to reflect upon the industry and organizational contexts before engaging in application of a tool for problem analysis. You will consider the organization’s setting with respect to level of care, mission, strategy, operations, and culture. Moreover, you will think critically about legal, regulatory, ethical, and risk management operational issues that relate to the selected problem. Let’s get started.
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate proficiency in the course competencies through the following assessment scoring guide criteria:
Competency 1: Evaluate problems in health care organizations, and apply tools to improve quality and outcomes.
Provide rationale for the selected problem analysis model or tool.
Competency 3: Construct evidence-based health care management recommendations in compliance with personal and professional values and legal, regulatory, and ethical considerations.
Construct evidence based recommendations which may include ethical, legal, regulatory, and organizational standards.
Competency 4: Analyze records and reports based on established benchmarks and organizational goals and performance.
Analyze date relative to internal and external benchmarks.
Preparation
As you prepare to complete this third course assessment, consider the organizational context. How does analysis of the problem align with the organization’s vision, mission, strategy and financial viability? Using numbers and organizational considerations, you will explain why the organization should or should not proceed with the recommendation.
Instructions
This assessment consists of three parts.
Data Presentation
In this part of the assessment, you will apply the selected tool to the problem and produce a minimum of two visual data displays (charts, graphs, et cetera). Examples of tools you might include are:
Cost Benefit Analysis: Excel spreadsheet, converted into 2–3 worksheet tabs, graphs, or other visual display format. Compliance Assessment: 3 major criteria converted into 3 separate pie charts or other graphic display format.
Lean Analysis: The percent of variance by major factor converted into 2–3 trend lines.
Note: At a minimum, provide a cost benefit analysis of the recommendation.
Quantitative and Qualitative Analysis of Data
In this part of the assessment you will analyze the collected data relative to benchmarks. Provide discussion as to whether the selected benchmarks are internal to the organization, external industry benchmarks, or a combination. Be sure to include a short summary of observations. Note: If the problem requires an additional tool, such as a compliance audit tool, you may include more than one discussion of the results.
Evidence-Based Recommendations
In this final part of the assessment, provide evidence-based recommendations that will help to address the identified problem. Be sure to support your recommendations with references to current, scholarly, and/or authoritative sources. Also include an explanation as to why the recommendations are feasible for this particular organization. For example, one recommendation might be to offer a new service line. Even though the new service may not generate an immediate profit, it might serve to draw additional patients into the network.
BHA FPX4020 Assessment 4 Instructions: Interdisciplinary Presentation of Evidence-Based Recommendation
Create and deliver a slide presentation (8-12 slides; 3-5 minutes maximum presentation) on the analysis of a selected health care problem that includes evidence-based recommendations. Your submission needs to include a narrated webcam recording, using your PowerPoint slides and speaker notes, which serve as a transcript.
Health care leaders scan for emerging and existing issues, prioritize problems, collect and analyze data, propose evidence-based solutions, and engage diverse teams in the process. Once a problem has been sufficiently analyzed, the health care leader must identify stakeholders who will participate in the final decision making for a proposed evidence-based solution.
Most importantly, the health care leader must craft a message that is aligned with organizational mission and strategy, based upon sound analysis and data, and includes of a wide variety of diverse stakeholders. The message needs to be communicated in a clear, concise, culturally competent, balanced, and professional manner.
In this assessment, you will have an opportunity to practice a wide variety of executive level skills by conducting a PowerPoint presentation on the selected health care problem. You will demonstrate a flow of logic and analysis by following a slide presentation outline template. In the presentation you will carry forward the work already completed in Assessment 3. Specifically you will cover the following in your presentation:
State the problem.
Identify clearly the relevant factors or performance indicators and associated units of measurement. Describe the application of an appropriate analysis tool to the problem.
Offer insights and evidence-based recommendations.
As you prepare for this webcam presentation, keep the imaginary audience in mind. It is comprised of a diverse senior leadership team at the selected organization. The team represents a variety of ages, cultures, and perspectives. You will communicate your presentation in a concise, professional, and culturally competent manner. The goal is to persuade the senior leadership team to implement the evidence-based recommendations presented. Consider that two senior leadership team members may be evaluating you as a high potential candidate for a promotion. Good luck! It is time to construct your presentation.
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
Competency 3: Construct evidence-based health care management recommendations in compliance with personal and professional values and legal, regulatory, and ethical considerations.
Analyze evidence-based recommendations with respect to organizational context. Provide rationale for the execution of evidence-based recommendations.
Competency 5: Create comprehensive and useable data-driven action plans, based on industry benchmarks.
Construct a data-driven action plan based upon industry benchmarks to solve the selected health care problem.
Competency 6: Communicate effectively with diverse audiences, in an appropriate form and style, consistent with applicable organizational, professional, and scholarly standards.
Create a succinct PowerPoint presentation on the selected problem and recommendations that is designed for interdepartmental senior leadership team viewing.
Preparation
Complete these tasks to successfully prepare for this presentation.
Slides
Review Guidelines for Effective PowerPoint Presentations [PPTX] for a refresher on how to create compelling, visually appealing slides that capture the audience’s attention.
Download and study the Final PowerPoint Template [PPTX] for a suggested structure for the slides. Using the slide template will help to keep your presentation within the maximum 3 to 5 minute presentation time frame.
Practice Video Recording the Presentation
After developing slides and preparing your speaker notes, practice delivering the presentation multiple times via screen and webcam recording before making the final webcam recording for submission. Practicing your presentation multiple times will make the presentation more polished and professional. Likewise, multiple dry runs will also help you adhere to the 3 to 5 minute maximum presentation length. Before submitting the presentation, make sure the recording is audible, the slides are visible, and that you are included in a video capture.
Consult the Using Kaltura [PDF] for additional guidance on how to record the presentation.
Instructions
Use the Final PowerPoint [PPTX] template to create a 3–5 minute recorded PowerPoint presentation of 8–12 preformatted slides. The template provides the outline of what you need to cover in the presentation. The goal of this assessment is to communicate essential elements of your analysis in a succinct manner. A 3- to 5-minute presentation may not seem long, but it is the reality in today’s health care workplace. Busy executives will not be able to spare more time than this. The presentation is for interdepartmental senior leadership team viewing.
Be sure to include visual summaries of your data, such as a pie chart or graph. The summarized data visual display should be in a readable format in a Word document or spreadsheet. It is important to include specific titles for the data summaries that identify the subject matter and measurement units.
BHA FPX4020 Assessment 5 Instructions: Health Care Leadership
Complete a self-assessment of 25 ACHE leadership competencies. Prepare a personal development plan that identifies specific action steps and due dates for improvement of five selected leadership competencies.
Throughout their careers, health care leaders must regularly assess their individual competencies and how those competencies align with organizational needs and priorities. Changing laws, regulations, technology, consumer preferences, medical treatment advances, and external environmental shifts can affect the skill sets needed for effective leadership. Accurate self-assessment is an important first step in identification of areas for future leadership development.
In this assessment, you will reflect upon your performance with respect to the industry-validated ACHE leadership competency model. After identifying areas of strength and a
READ MORE >>
BHA FPX 4108 Assessment 4 Instructions: Community Health Action PlanUse the prov ...
BHA FPX 4108 Assessment 4 Instructions: Community Health Action Plan
Use the provided template to create an action plan to address a chosen health problem.
Introduction
Information technology, specifically electronic health records (EHR) and patient portals, are helping to empower patients to take a more active role with their health care (Nash, Fabius, Skoufalos, & Clarke, 2016). Information technology is also supporting collaborative efforts among multiple health care stakeholders, including providers, insurers, community health agencies, and policy makers (Nash, Fabius, Skoufalos, & Clarke, 2016).
The use of decision support systems facilitates the mining of large amounts of data in population health, including data measurement and analysis. Three purposes of measurement include improvement, accountability, and research (Nash, Fabius, Skoufalos, & Clarke, 2016). Decision support systems can also be used for predictive modeling to improve performance and predict potential outcomes (Nash, Fabius, Skoufalos, & Clarke, 2016). As information technology and decision support systems become more sophisticated, and larger amounts of data are captured, the potential to further the IHI Triple Aim initiatives discussed previously in the course increases.
Population health continues to evolve, and the Affordable Care Act (ACA) introduced several new regulations and models. The IHI Triple Aim initiative will be an ongoing area of focus, and information technology offers new ways to engage patients in their own health. Smart phones, health and wellness apps, and smart watches will give patients new ways to monitor their behaviors.
As providers educate themselves on behavioral change models and economics, they can help patients change unhealthy behaviors. Nash, Fabius, Skoufalos, and Clarke (2016) predict that the next few years will likely result in an updated health risk assessment that includes additional determinants of health and performance, including stress and anxiety, and increased recognition of the importance of thriving and health. Beyond five years, we will likely see shared values among employers, employees, and the community.
Taking measurements, regulations, current and evolving technology, and models of care into account is critical to help ensure sound design of population and community health plans. Without a well-thought-out design, a well-thought-out and implementable action plan will prove difficult to impossible. So, these are critical considerations as you approach the Community Health Action Plan assessment.
Reference
Nash, D. B., Fabius, R. J., Skoufalos, A., & Clarke, J. L. (2016). Population health: Creating a culture of wellness (2nd ed.). Burlington, MA: Jones & Bartlett Learning.
Demonstration of Proficiency
Competency 1: Integrate principles of epidemiology, population health, and community engagement to plan interventions.
Evaluate an organization best suited to implement a community-health intervention.
Competency 2: Differentiate and evaluate evidence-based treatment models and prevention models designed to promote wellness and disease management for population health.
Formulate criteria for evaluation of task completion.
Competency 3: Create an action plan to promote wellness and disease management in a diverse population.
Define a goal for an action plan.
Identify roles, tasks, and timeframes required to implement a plan.
Identify human, capital, and material resources needed to complete tasks in a plan.
Competency 4: Communicate in a manner that is scholarly, professional, and respectful of the diversity, dignity, and integrity of others and is consistent with expectations for health care professionals.
Write clearly and logically, with correct use of spelling, grammar, punctuation, and mechanics. Write following APA style for in-text citation, quotes, and references.
Note: It is recommended that you complete the assessments in this course in the order they are presented.
Preparation
This assessment brings together aspects of the other three assessments in the course. The goal is to create an implementable action plan to achieve a SMART goal addressing the community-health need you have been exploring throughout the course.
To prepare to successfully create your Community Health Action Plan, it is recommended you complete the following:
Familiarize yourself with the Action Plan Template you will be completing as your assessment artifact.
Consult your previous assessments, and the feedback you received on them, to focus on what areas you should focus on when completing the template.
It may be helpful to complete the Community Health Programs formative activity.
BHA FPX 4108 Assessment 4 Instructions: Community Health Action Plan Instructions
For this assessment, create a detailed action plan to promote wellness and disease management by addressing your chosen health problem you have been working on throughout this course. Based on feedback received on your previous assessments, design a plan you could implement in a health care organization (such as a hospital, physician practice, or federally qualified health center) to address a specific SMART goal.
Make sure you download and complete the Action Plan Template. Only submit the completed template for your assessment. Do not submit a paper for this assessment. Papers will not be graded.
Consult the scoring guide to ensure that you are addressing all criteria at the level to which you desire. When completing the template, be sure you address the following:
Define a goal for an action plan.
You may want to review either (or both) of the media pieces related to SMART goals to help in addressing this criterion: SMART Goals | Transcript.
Evidence-Based Strategies and SMART Goals | Transcript.
Evaluate an organization best suited to implement a community-health intervention.
Identify a specific organization best suited to address the problem and implement the potential solution you have selected based on your work in the other assessments in the course.
Why is the organization best suited to address your chosen health problem? Why is the organization best suited to implement your potential solution?
How is the organization best suited to engage and help the affected populations in the community?
Identify roles, tasks, and time frames required to implement a plan.
This criterion is related to the first two columns in the template.
Be sure to detail the specific tasks that must be completed based on the research you have conducted in the first column.
Identify the roles of all stakeholders needed to implement your plan. Explain why they are needed.
For each task, be sure to identify an appropriate and realistic timeframe to complete the task in the second column.
Formulate criteria for evaluation of task completion.
This criterion is related to the third column of the template.
Make specific connections between these criteria and evidence-based strategies to promote wellness and disease management for a population.
Identify human, capital, and material resources needed to complete tasks in a plan.
This criterion is related to the fourth column of the template, as well as the Key Stakeholders section.
For the stakeholders:
Which stakeholders are required to complete each task? What are the roles of the stakeholders?
In other words, why are the specific stakeholders needed?
Additionally, make sure you identify any other people, capital, materials, and so on, needed to complete a task.
Write clearly, with correct spelling, grammar, and syntax, and good organization. Apply proper APA formatting and style.
Additional Requirements
Written communication: Ensure content is free of errors that detract from the overall message.
APA: Use current-edition APA style and formatting guidelines, including citations and a reference page in the second tab of the Action Plan Template
Action Plan Template
Goal or Objective: Organization: Key Stakeholders: Tasks (High level overview of each step to achieve the stated goal or objective)Time Frame and Due Date (Duration of task and final due date)Success Criteria (How will you know the task has been completed?)Resources (Stakeholders, materials, property, et cetera that will be neededAction Plan Template Example
Goal or Objective:To reduce the COVID-19 infection rates to the level of evidence-based safe infection rate of sustained decline of cases over 14 daysOrganization:Missouri Department of Health and Senior ServicesKey Stakeholders:communicable disease reporting and surveillance agency, state public health laboratory, community health workers, all hospitals and healthcare organizations Tasks (High level overview of each step to achieve the stated goal or objective)Time Frame and Due Date (Duration of task and final due date)Success Criteria (How will you know the task has been completed?)Resources (Stakeholders, materials, property, et cetera that will be neededThe two meter social distance, which encourages people to stay at least six feet from each other especially in a public area.Time frame is not clearly defined because the virus is still on the spread and other variants of the virus are still emerging.Success shall have been achieved if the infection rate decreases within 14 days. However, this prevention measure should be maintained until a cure for the virus is developedCommunity members/citizens (to maintain social distancing), the government (federal, local, state). There are however, no extra resources need.regularly disinfecting frequently held surfaces such as shopping carts, door knobs, counter top surfaces and seats.Time frame is not clearly defined because the virus is still on the spread and other variants of the virus are still emerging.Success shall have been achieved if the infection rate decreases within 14 days. However, this prevention measure should be maintained until a cure for the virus is developedCommunity members/citizens (to maintain social distancing) and the government (federal, local, state). There needs to be disinfectant materials provided by health authoritiesPracticing safe sneezing or coughing by covering nose to limit the spread of potentially infected droplets.Time frame is not clearly defined because the virus is still on the spread and other variants of the virus are still emerging.Success shall have been achieved if the infection rate decreases within 14 days. However, this prevention measure should be maintained until a cure for the virus is developedCommunity members/citizens (to maintain social distancing), the government (federal, local, state). Additional testing kits from the government would be necessaryEnsuring that individuals who show symptoms of infection are immediately tested so that those who test positive are immediately quarantined and treated (Bruns, 2020).Time frame is not clearly defined because the virus is still on the spread and other variants of the virus are still emerging.Success shall have been achieved if the infection rate decreases within 14 days. However, this prevention measure should be maintained until a cure for the virus is developedCommunity members/citizens (to maintain social distancing), the government (federal, local, state). Both business and individuals would need handwashing soaps and disinfectants from the governmentConsistently adhering to basic hygiene protocols such as hand washing after touching surfaces or after visiting a public place (Gonzales et al. 2020).Time frame is not clearly defined because the virus is still on the spread and other variants of the virus are still emerging.Success shall have been achieved if the infection rate decreases within 14 days. However, this prevention measure should be maintained until a cure for the virus is developedCommunity members/citizens (to maintain social distancing), the government (federal, local, state). No additional materials are neededAvoiding crowded places especially those who have weakened immune system because otherwise they are vulnerable to COVID-19 (Zanettini et al, 2020).Time frame is not clearly defined because the virus is still on the spread and other variants of the virus are still emerging.Success shall have been achieved if the infection rate decreases. However, this prevention measure should be maintained until a cure for the virus is developedCommunity members/citizens, the government (federal, local, state). There are no materials neededUsing facemask to cover both nose and mouth. This helps to break the chain of infection by preventing potentially infected droplets from transferring to or from other people.Time frame is not clearly defined because the virus is still on the spread and other variants of the virus are still emerging.Success shall have been achieved if the infection rate decreases within 14 days. However, this prevention measure should be maintained until a cure for the virus is developedCommunity members/citizens, the government (federal, local, state). Individuals will need to purchase facemasksAvoiding physical contacts such as hugs and handshakes as part of avoiding close contact with others (Bruns, 2020).Time frame is not clearly defined because the virus is still on the spread and other variants of the virus are still emerging.Success shall have been achieved if the infection rate decreases within 14 days. However, this prevention measure should be maintained until a cure for the virus is developedCommunity members/citizens, the government (federal, local, state). There are no materials neededREAD MORE >>
