Our Previous Samples
Assignment: Formal vs Informal CounselingAssignment: Formal vs Informal Counseli ...
Assignment: Formal vs Informal Counseling
Assignment: Formal vs Informal Counseling
Difference between Formal vs Informal Counseling. A survey of mental health and includes diagnosis, counseling and effectiveness of counseling.
- Discuss differentiation of formal (professional) from informal (non-professional) counseling. Why is this differentiation essential?
© BrainMass Inc. brainmass.com March 21, 3:41 pm ad1c9bdddf
https://brainmass.com/psychology/abnormal-psychology/160570
Formal vs Informal Counseling Solution Preview
Hi,
This is an interesting topic! Let’s take a closer look.
Assignment: Formal vs Informal Counseling RESPONSE:
Formal vs. Informal Counseling. A survey of mental health and includes diagnosis, counseling and effectiveness of counseling. Discuss differentiation of formal (professional) from informal (non-professional) counseling. Why is this differentiation essential?
Counseling comes in two flavors: formal and informal, which are indeed very different, each having advantages and disadvantages based on the situation and person.

Assignment: Formal vs Informal Counseling INFORMAL COUNSELING
Informal counseling is defined in different ways. It consists of nothing more entering into conversation and listening to someone, such as being available or pulling someone aside for a quiet word about some problem they’re having. Assignment: Formal vs Informal Counseling. However, in a work situation, for example, as a supervisor might engage in informal counsel on the spur of the moment about something that happened only a second ago. In fact, this is probably the best use of this type of counseling, according to some.
The important thing to remember about informal counseling is to use the Golden Rule of Counseling – praise in public, reprimand in private. Assignment: Formal vs Informal Counseling. Don’t, for example, ever bite a big piece off of someone in front of everybody. All that does is embarrass the person unnecessarily and can destroy their self-esteem. It will also make you seem like a complete tyrant. No one wants to work for someone or be in relationship with someone who, if something goes wrong, will make her or him feel stupid in public.
READ MORE >>
Assignment Katherine Harris iHuman Case StudyNSG 6435 Week 4 Discussion: iHuman ...
Assignment Katherine Harris iHuman Case Study
NSG 6435 Week 4 Discussion: iHuman Case Study – HEENT and Respiratory Infections
This discussion assignment provides a forum for discussing relevant topics for this week based on the course competencies covered. For this assignment, make sure you post your initial response to the Discussion Area.
To support your work, use your course textbook readings and the South University Online Library. As in all assignments, cite your sources in your work and provide references for the citations in APA format.

Start reviewing and responding to the postings of your classmates as early in the week as possible. Respond to at least two of your classmates’ initial postings. Participate in the discussion by asking a question, providing a statement of clarification, providing a point of view with a rationale, challenging an aspect of the discussion, or indicating a relationship between two or more lines of reasoning in the discussion. Assignment Katherine Harris iHuman Case Study. Cite sources in your responses to other classmates. Complete your participation for this assignment.
For this assignment, you will complete an iHuman case study based on the course objectives and weekly content. iHuman cases emphasize core learning objectives for an evidence-based primary care curriculum. Assignment Katherine Harris iHuman Case Study.
Throughout your nurse practitioner program, you will use the iHuman case studies to promote the development of clinical reasoning through the use of ongoing assessments and diagnostic skills and to develop patient care plans that are grounded in the latest clinical guidelines and evidence-based practice.
The iHuman assignments are highly interactive and a dynamic way to enhance your learning. Material from the iHuman cases may be present in the quizzes, the midterm exam, and the final exam.
- Here you can view information on how to access and navigate iHuman.
- This week, complete the iHuman case titled “Katherine Harris.”
Apply information from the iHuman Case Study to answer the following questions:
- Do you recommend a limited or an involved use of antibiotics in treatment of these diseases and other unconfirmed bacterial illnesses and why? What are the standards regarding the use of antibiotics in pediatric population, and what assessment findings would warrant prescribing an antibiotic for Asthma symptoms?
- Using national guidelines and evidence-based literature, develop an Asthma Action Plan for this patient. Assignment Katherine Harris iHuman Case Study.
- Do the etiology, diagnosis, and management of a child who is wheezing vary according to the child’s age? Why or why not? Which objective of the clinical findings will guide your diagnosis? Why? When is a chest x-ray indicated in this case?
Week 7 Assignment 1: Discussion: iHuman Case Study-Gonorrhea
**Discuss the questions that would be important to include when interviewing a patient with this issue.
Why are you seeking help today? I have been having burning when I pee and vaginal discharge for a few days. I was worried that I had another bladder infection, but these symptoms are a little different.
When did your pain with urination start? About three days ago
What are the events surrounding the start of your pain with urination? Well, it came on pretty much with the discharge. It was hard to tell what’s what
Does anything make your pain with urination better or worse? Soaking in a warm bath helps
Do you have any other symptoms associated with painful urination? Well, yeah. The discharge I told you about.
Have you had problems with painful urination like before? Yes, with my bladder infection last year. But I’m wondering if this is really the same thing.
How often do you have pain with urination? Every time I pee.
What is the appearance, smell, texture and quantity of the vaginal discharge? Oh boy…I hate having to answer these questions. Yellow, kind of mucousy, kind of creamy. Not too smelly.
Is there vaginal discomfort or itching? No, nothing like a yeast infection.
Are you sexually active? Yes, I am.
How often are you having intercourse? Well, let’s just say I like men and they like me. I’ve been with a few different guys over the last 6 months. I haven’t done it with anyone since this started a few days ago. The last time was maybe a week ago?
Are you having or have you had unprotected sex? Yeah, I guess so. Sometimes I forget about condoms if I’ve been drinking. I’m on the pill, so I guess I’m protected that way.
Do you use precautions to prevent the transmission of sexual diseases? Nothing but the pill.
Do you have more than one sexual partner? Yes
Do you have new or multiple sexual partners with similar symptoms? Well, no one has told me he has any problem.
Have you had any sexually transmitted disease? Not that I know of.
Do you have sex with men, women, or both? I’m heterosexual.
Are you taking any prescription medications? No, other than the pill.
Are you taking any over the counter medications? Yeah, sometimes I take ibuprofen with my period. You know, like for cramps and headaches.
Do you have any pelvic pain? No
Do you have any blood in your urine? No
Do you have any genital sores or discharge? No sores, but I do have some vaginal discharge.
**Describe the clinical findings that may be present in a patient with this issue.
Symptoms are often nonspecific and may include increased vaginal discharge, dysuria, urinary frequency, and intermenstrual or postcoital bleeding. If the infection has been long-standing, symptoms can include low abdominal or low back pain (Dowell & Kirkcaldy, 2013)
**Are there any diagnostic studies that should be ordered on this patient? Why?
The Centers for Disease Control and Prevention (CDC) recommends testing on self- or clinician-collected endocervical and vaginal swab specimens, as well as on urine specimens. Nucleic acid amplification testing (NAAT) is the most sensitive and specific for gonorrheal and chlamydial infections, and it also allows for testing on the widest variety of specimen types (“Cervicitis Workup,” 2017).
**List the primary diagnosis and three differential diagnoses for this patient. Explain your reasoning for each.
Primary diagnosis – Cervicitis: Culture-proven, uncomplicated gonorrhea
Candida vaginitis is a vaginal yeast infection that is caused by the organism
Candida albican that is a naturally occurring microorganism in the vaginal area. Lactobacillus bacteria keeps its growth in check although if there’s an imbalance in your system, these bacteria won’t work effectively (Martin Lopez, 2015). This leads to an overgrowth of yeast, which causes the symptoms of vaginal yeast infections. Clinically a diagnosis is made by the presence of external dysuria and vulvar pruritus, pain, swelling, and redness. Signs also include vulvar edema, fissures, excoriations, and thick curdy vaginal discharge. This is not supported by clinical & physical assessment.
Pelvic inflammatory disease (PID) is an infection of the upper part of the female reproductive system namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis (Brunham, Gottlieb & Paavonen, 2015). Signs and symptoms, when present may include lower abdominal pain, vaginal discharge, fever, burning with urination, pain with sex, or irregular menstruation. Untreated PID can result in long term complications including infertility, ectopic pregnancy, chronic pelvic pain, and even cancer (Brunham et al, 2015). This is not supported by clinical & physical assessment.
Urinary Tract Infection is caused by a bacterium or virus infecting the kidneys. The infection may affect one or both upper urinary tracts which consist the ureter, renal pelvis, and kidney interstitium (Flores-Mireles, Walker, Caparon, & Hultgren, 2015). The infection is probably spread by ascending uropathic microorganisms?along the ureters, or can be carried through the bloodstream from other parts of the body.
Though many bacteria and viruses can cause pyelonephritis,?it is usually associated with Proteus, Pseudomonas though bacterium?Escherichia coli?is often the cause (Flores-Mireles et al., 2015). Symptoms are usually acute, with fever, chills, and flank or groin pain with most cases occurring in young adult women although older adults may have nonspecific symptoms, such as low-grade fever and malaise (Flores-Mireles et al., 2015). This is not supported by clinical & physical assessment.
**Discuss your management plan for this patient, including pharmacologic therapies, tests, patient education, referrals, and follow-ups.
Several factors should affect the decision to provide presumptive therapy for cervicitis or to await the results of diagnostic tests. Treatment with antibiotics for C. trachomatis should be provided for those women at increased risk for this common STD with a dose of Ceftriaxone 250 mg IM and Doxycycline 100 mg orally twice a day for 7 days can be used as an alternative in women who are not pregnant or breast feeding (Ebrahimy et al., 2015).
Patients must be educated that cervicitis is a preventable, sexually transmitted infection (STI) and that the most effective way to prevent the transmission of the infective agents is to avoid sexual intercourse without protection or infected partners. Partners should be notified and examined if chlamydia, gonorrhea, or trichomoniasis. Partners should then be treated for the STDs for which the index patient received treatment. Education on avoiding reinfection, patients and their sex partners should abstain from sexual intercourse until therapy is completed (Öztürk & Ulubay, 2016).
Follow-up should be conducted as recommended for the infections for which a woman is treated. If symptoms persist, women should be instructed to return for re-evaluation because women with documented chlamydial or gonococcal infections have a high rate of reinfection within 6 months after treatment. Therefore, repeat testing of all women with chlamydia or gonorrhea is recommended 3-6 months after treatment, regardless of whether their sex partners were treated (Ebrahimy et al., 2015).
References for Assignment Katherine Harris iHuman Case Study:
- Brunham, R. C., Gottlieb, S. L., & Paavonen, J. (2015). Pelvic inflammatory disease. The New England Journal of Medicine, 372(21), 2039.
- Cervicitis Workup. (2017). Retrieved from http://www.cdc.gov/std/treatment/2013/chlamydial-infections.htm
- Dowell, D., & Kirkcaldy, R. D. (2013). Effectiveness of gentamicin for gonorrhoea treatment: Systematic review and meta-analysis. Postgraduate Medical Journal, 89(1049), 142-147. doi:10.1136/postgradmedj-2012-050604rep
- Ebrahimy, F., Dolatian, M., Moatar, F., & Majd, H. A. (2015). Comparison of the therapeutic effects of garcin and fluconazole on candida vaginitis. Singapore Medical Journal, 56(10), 567-572. doi:10.11622/smedj.2015153
- Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nature Reviews. Microbiology, 13(5), 269. doi:10.1038/nrmicro3432
- Martin Lopez, J. E. (2015). Candidiasis (vulvovaginal). BMJ Clinical Evidence, 2015
- Öztürk, M., & Ulubay, M. (2016). Treatment of cervicitis; LEEP versus cryotherapy. Journal of the Turkish German Gynecological Association, 17, S7.
- Taylor, S. N. (2014). Cervicitis of unknown etiology. Current Infectious Disease Reports, 16(7), 1-5. doi:10.1007/s11908-014-0409-x
- Cervicitis Workup. (2017). Retrieved from http://www.cdc.gov/std/treatment/2013/chlamydial-infections.htm
READ MORE >>
Assignment: Malingering and Addiction in the Treatment of Sleep DisordersAccordi ...
Assignment: Malingering and Addiction in the Treatment of Sleep Disorders
According to the National Sleep Foundation (2013), about 30–40% of the general population reports some level of insomnia during their lives, and 10–15% experience significant, chronic insomnia. For these individuals, medications to help induce and sustain sleep may be helpful. On the other hand, sleep aids pose potential concerns, namely abuse.
Some people exceed recommended doses, and some continue taking medications even after symptoms are no longer present. Others obtain medications under false pretenses, which is one form of malingering. Malingering occurs when clients make up or exaggerate symptoms for some personal gain.
Although mental health professionals may not be directly implicated in the client’s deceit, their unique position to receive more accurate and honest information than malingering other medical professionals presents ethical concerns.
What is the mental health professional’s role in these instances? In which instances would it be appropriate to break confidentiality due to a concern of malingering? How could the potentiality be planned for and avoided?
For this Assignment, conduct an Internet search or a Walden Library search for at least one peer-reviewed journal article that addresses a counseling issue related to malingering and addiction in treating sleep disorders.

BY DAY 7
In a 3- to 5-page, APA-formatted paper, include the following:
- A description and explanation of the major types of drugs prescribed for sleep disorders
- An explanation of the potential for addiction associated with these medicines
- An explanation of the issues related to malingering in the treatment of sleep disorders
- An explanation of the mental health professional’s role in mitigating the potentialities of malingering
Support your explanations with specific references to the Learning Resources and your peer-reviewed journal article
Assessing and Treating Patients with Sleep/Wake Disorders Example
Mental health disorders diagnosis and management are often symptomatic. Care providers use symptoms according to DSM 5 to diagnose and prescribe medications according to their effectiveness and FDA approval. Care providers observe patients’ responses and determine the management interventions depending on their response to the interventions. Psychiatric/mental health nurses play vital roles in assessing patients, and prescribing the correct medication interventions is integral. Insomnia is a mental health issue defined as trouble initiating or maintaining sleep and waking up early.
Insomnia accompanies most conditions, such as Alzheimer’s disease. It also arises from environmental stressors such as depression and medications such as alpha and beta blockers. Insomnia can negatively affect health and productivity and should be promptly addressed while paying attention to the adverse effects and their effects on life quality. This essay reviews management interventions for insomnia patients and explains the reasons behind the decisions.
Decision Point One
The patient presents with insomnia and clarifies that he has trouble falling asleep and maintaining sleep. The patient admitted to having less sleep at night and had an incidence of sleeping at work for not having enough night sleep, which is dangerous given the risky nature of his job. The patient also reports that his symptoms worsened after losing her fiancé. He used diphenhydramine for a while but stopped due to the side effects. The goals of the first decision are to ensure the patient has no problems initiating or maintaining sleep, does not sleep at work or, experiences daytime sleepiness, and reduces risky incidences at work.
The first decision is to initiate Zolpidem 10mg at bedtime. Zolpidem is a sedative-hypnotic in the class of imidazopyridines and a GABA A receptor agonist. It is an FDA-approved medication for short-term insomnia management (Xiang et al., 2020). According to Bouchette et al. (2022), the medication is helpful for patients with problems initiating sleep, improves sleep duration, and reduces night awakenings in transient insomnia. These functions match the requirements of patients who have trouble initiating and maintaining sleep. The approved dose in adults is 10mg and 5mg in the elderly.
Trazodone is an antidepressant medication often used in major depression, mood and anxiety disorders, and sleep disorders. Trazodone is a serotonin antagonist and reuptake inhibitor that is FDA-approved for depression (Stern et al., 2016). According to Madari et al. (2021), The medication is effective at doses between 20-100mg and reduces the risks for tolerance and daytime sleep. It can also be helpful for this patient who admits to being depressed after losing his partner. However, there is insufficient data on its effectiveness in insomnia; thus, the medication is not FDA-approved for insomnia but has off-label uses in managing insomnia. Thus, it is not the decision of choice.
Hydroxyzine is an antihistamine often used for allergic reactions. The medications’ drowsy effects take 4-6 hours, hence their limited use in managing sleep. The medication is FDA-approved for providing sedation (hence used as premedication in procedures), relieving anxiety symptoms, and relieving skin itchiness in atopic dermatitis (Krzystanek et al., 2020). The medication helps relieve insomnia resulting from anxiety. However, the medication is not approved for FDA-approved for insomnia. In addition, the patients admit to developing severe side effects that affect his uptake of antihistamines; thus, this medication is not the medication of choice. Therapy changes using drugs in the same class are done with caution due to the possibility of severe side effects.
It is also essential to consider the safety and effectiveness of the medication before medication. In addition, it is essential to consider the side effects of medications that could interfere with intake. For example, medications with low efficacy or late onset of action may not help manage acute symptoms. It is vital to avoid medication with a short maximum use period. Trazodone is licensed for use for a maximum of 2 weeks. Patient safety is essential, and for initiating therapy, the FDA recommends that healthcare providers prescribe FDA-approved medications and only use off-label mediations in rare occasions such as resistance, known greater efficacy, and unavailability of FDA-approved medications (Bouchette et al., 2021).
Decision Point #2
Once care providers make a medical management decision, they observe the patient’s reaction and make medical decisions depending on side effects and effectiveness in managing the symptoms. The patient had a night wakening, does not recall the incident, and says he sleeps well. He claims the medication knocked him out. The desired outcomes of this decision are the maintenance of effectiveness in sleep management and the reduction of complex sleep behaviors.
Harbout et al. (2020) note that zolpidem and other medications, such as zaleplon, have an FDA-black box warning indicating their risk for injury due to complex sleep behaviors that they do not remember later. The medication has led to symptom relief, but the side effects may warrant dose adjustment; reducing the doses when side effects arise is a recommended intervention by the FDA. Thus, reducing the drug dose to 5mg from 10mg is the intervention of choice.
Eszopiclone is an FDA-approved medication for insomnia. The symptoms of interest in this patient are complex sleep behaviors, such as waking up and doing roles that he has no memory of in the morning. Eszopiclone, zaleplon, and zolpidem are medications with increased risk for complex sleep behaviors and are thus not a drug of choice (Harbout et al., 2020). Its side effect profile also rules out its use in insomnia. Its typical side effects include daytime drowsiness, lightheadedness, and loss of coordination, which present symptoms similar to those the patient presented on the first visit, ruling out the decision.
Trazodone, as discussed earlier, is a non-FDA-approved medication. The dose is within the minimum and maximum licensed doses. However, the patient is already responding to the medication prescribed, and thus, there is no need for a therapy change. However, the drug can be considered if selected insomnia medications are ineffective or cause undesirable side effects (Maradani et al., 2021). The patient reports reduced sleep awakening and trouble initiating sleep and reports sleeping well. The side effects that arose do not require a therapy change but a dose reduction and subsequent observation. However, their persistence may warrant therapy changes.
In this decision, the principle of non-maleficence applies. The intention is to ensure that the decision made relays the least harm and maximum benefits to the patient. The medication given, zolpidem, is effective in managing insomnia symptoms but has led to undesirable effects. A reduction in the dose of the medication is the intervention of choice to help reduce the side effects while maintaining clinical effectiveness. The drug’s lowest licensed dose is 5mg before bedtime; thus, reducing the dose will maintain the drug’s efficacy and reduce the side effects.
Decision Point Three
The third decision depends on the current patient presentations. The patient returns to the hospital after reducing the dose to 5mg before bedtime. The symptoms have significantly reduced, and the patient likes the drug due to its ability to help him maintain sleep. However, the complex behaviors have not ceased and have persisted. This decision aims to eliminate the side effects while maintaining insomnia management. Despite Zolpidem FDA-approval, the medication has a horde of side effects preventing its first-line use (Mittal et al., 2021).
Choice decides to discontinue zolpidem and start the patient on trazodone 50mg. Mittal et al. (2021) note that the medication is highly effective in insomnia but is a double-edged sword due to its severe side effects, especially on complex sleep behaviors. These complex behaviors, such as waking up and preparing to go to work, can lead to activities that can cause harm, such as leaving the house at night. The medication should be stopped to prevent the patient from any harm.
Intermezzo is a brand for zolpidem, and these medications have similar structure and effectiveness and thus carry a high risk for recurrence or worsening of these symptoms. Thus, intermezzo 5mg sublingually before bedtime is not the decision of choice. Trazodone is a well-tolerated medication with fewer side effects compared to the medication (Madari et al.., 2021). The drug is administered in small doses, reducing the side effects severity.
Titrating the medication between 50 and 100 mg on the upper limit will allow the care providers to study the drug’s efficacy, tolerability, and side effects (Madari et al., 2021). The medication will help address the symptoms because studies show that trazodone is not associated with complex sleep behaviors and is, thus, a choice drug. Continuous patient observation and review of the medications will help with management and prevent complications.
The most critical ethical consideration is non-maleficence. Despite the effectiveness of the medication, the patient is experiencing marked complex sleep behaviors that potentially affect his life. Patients who perceive a medication as a threat can fear poor drug adherence affecting remission. Thus, changing the therapy to help manage the side effects is vital to maintaining the patient’s adherence and confidence in the mediation.
Conclusion
Insomnia can affect various aspects of life, and its management should be well-evaluated to ensure it does not affect other aspects. Zolpidem is an effective medication for insomnia but carries a significant risk for complex sleep behaviors, which could negatively impact patient safety. Thus, the medication is often avoided as the first-line treatment despite its FDA approval. Assessing the patient and collecting relevant data during every visit helps care providers determine patient needs and intervene accordingly.
Zolpidem achieves the therapeutic targets but leads to the development of undesirable side effects that do not cease with drug reduction. A change of therapy to trazodone, an effective off-label drug, is the intervention of choice due to its high efficacy and fewer side effects. Healthcare providers should assess therapeutic interventions regularly to ensure they produce the desired effects and their benefits outdo any harm they relay to the patients.
Assignment: Malingering and Addiction in the Treatment of Sleep Disorders References
Bouchette, D., Akhondi, H., & Quick, J. (2022). Zolpidem. In StatPearls [Internet]. StatPearls Publishing.
Harbourt, K., Nevo, O. N., Zhang, R., Chan, V., & Croteau, D. (2020). Association of eszopiclone, zaleplon, or zolpidem with complex sleep behaviors resulting in serious injuries, including death. Pharmacoepidemiology and drug safety, 29(6), 684–691. https://doi.org/10.1002/pds.5004
Krzystanek, M., Krysta, K., & Pa?asz, A. (2020). First generation antihistaminic drugs used in the treatment of insomnia–superstitions and evidence. Pharmacotherapy in Psychiatry and Neurology/Farmakoterapia w Psychiatrii i Neurologii, 36(1), 33-40.
Madari, S., Golebiowski, R., Mansukhani, M. P., & Kolla, B. P. (2021). Pharmacological management of insomnia. Neurotherapeutics, 18(1), 44-52. https://doi.org/10.1007/s13311-021-01010-z
Mittal, N., Mittal, R., & Gupta, M. C. (2021). Zolpidem for insomnia: a Double-edged Sword. a Systematic Literature Review on Zolpidem-induced Complex Sleep behaviors. Indian Journal of Psychological Medicine, 43(5), 373–381. https://doi.org/10.1177/0253717621992372
Stern, T. A., Favo, M., Wilens, T. E., & Rosenbaum, J. F. (2016). Massachusetts General Hospital psychopharmacology and neurotherapeutics. Elsevier
Xiang, T., Cai, Y., Hong, Z., & Pan, J. (2021). Efficacy and safety of zolpidem in the treatment of insomnia disorder for one month: a meta-analysis of a randomized controlled trial. Sleep Medicine, 87, 250-256. https://doi.org/10.1016/j.sleep.2021.09.005
REQUIRED READINGS for Assignment: Malingering and Addiction in the Treatment of Sleep Disorders
Lichtblau, L. (2011). Psychopharmacology demystified. Clifton Park, NY: Delmar, Cengage Learning.
- Chapter 6, “Anxiolytic-Sedative-Hypnotic Drug Pharmacotherapy” (previously read in Week 5)
Preston, J. D., O’Neal, J. H., & Talaga, M. C. (2017). Handbook of clinical psychopharmacology for therapists (8th ed.). Oakland, CA: New Harbinger.
- Chapter 15, “Other Miscellaneous Disorders” (pp. 161-174)
- Assignment: Malingering and Addiction in the Treatment of Sleep Disorders
Murdach, A. D. (2006). Social work and malingering. Health & Social Work, 31(2), 155-8.
National Institute of Neurological Disorders and Stroke. (2014). Brain basics: Understanding sleep. Retrieved from http://www.ninds.nih.gov/disorders/brain_basics/understanding_sleep.htm#sleep_disorders
As you review this website, consider the types of sleep disorders associated with mental health treatment.
Instructions for Assignment: Malingering and Addiction in the Treatment of Sleep Disorders
You must proofread your paper. But do not strictly rely on your computer’s spell-checker and grammar-checker; failure to do so indicates a lack of effort on your part, and you can expect your grade to suffer accordingly.
Papers with numerous misspelled words and grammatical mistakes will be penalized. Read over your paper – in silence and then aloud – before handing it in, and make corrections as necessary. Often it is advantageous to have a friend proofread your paper for obvious errors. Handwritten corrections are preferable to uncorrected mistakes.
Use a standard 10 to 12-point (10 to 12 characters per inch) typeface. Smaller or compressed type and papers with small margins or single-spacing are hard to read. It is better to let your essay run over the recommended number of pages than to try to compress it into fewer pages.
Likewise, large type, large margins, large indentations, triple-spacing, increased leading (space between lines), increased kerning (space between letters), and any other such attempts at “padding” to increase the length of a paper are unacceptable, wasteful of trees, and will not fool your professor.
The paper must be neatly formatted, double-spaced with a one-inch margin on the top, bottom, and sides of each page. When submitting a hard copy, be sure to use white paper and print it out using dark ink. If it is hard to read your essay, it will also be hard to follow your argument.
Also Read:
HCA 459 Entire Course Discussion
Critically analyze some aspect of a personality theory
Module 1: The Keys to Persuasion
Discussion: Probability and Probability Distributions
Benchmark – Staffing Matrix And Reflection
Insomnia Response Sample paper
Introduction
Hi Sara, as you have promptly identified, the patient is experiencing insomnia, which is the inability to obtain sufficient or good quality sleep. Often, insomnia is characterized by patient’s inability to sustain sleep, difficulty falling asleep, getting up too early and feeling fatigued, inability to concentrate, and irritability over the day. The causes of insomnia vary but are largely attributable to psychiatric conditions such as mood and anxiety disorders (Patel, Steinberg & Patel, 2018).
Your idea of using questions to develop the best treatment plan for the patient, through time evaluation of the period that insomnia has been experienced, we can be able to categorize insomnia as acute or chronic. It also promotes understating of the aggravating factors. One needs to evaluate the patient’s sleep habits and for how long the patient has been taking sertraline, an antidepressant that may have the side effect of insomnia.
I have also found your idea that a support system to the patient is of great importance as many people of this age depend on their children and caretakers to meet their needs. The support system provides answers to the patient’s change in mood and behavior or whether she is still recovering from the bereavement, as well as the likely continued abuse of illegal substances. She will need support if she is depressed since it is associated with an increased likelihood of comorbidity, physical illness, and suicide leading to premature death.
Further, your differential diagnoses that include complicated grief due to prolonged emotional responses to the loss of a husband is plausible. However, it is also important to assess for drug-induced insomnia such as sertraline and antidepressants as they “cause activation of serotonergic 5-HT2 receptors and increased noradrenergic and dopaminergic neurotransmission,” (Riemann et al., 2017). Diagnosis should be carried out using Hamilton Rating Scale for Depression, Beck Depression Inventory (BDI), and Geriatric Depression Scale (Riemann et al., 2017)
In my opinion use of Mirtazapine has great advantages to the patient in the improvement of patient insomnia episodes as it does not have anticholinergic or cardiovascular system side effects. The use of Trazadone in place of sertraline has also been effective since it reduces insomnia episodes. Provide the patient with a follow up 1-2 weeks to ensure compliance by the patient (Gandotra et al., 2018).
References
- Patel, D., Steinberg, J., & Patel, P. (2018). Insomnia in the Elderly: A Review. Journal Of Clinical Sleep Medicine, 14(06), 1017-1024. https://doi.org/10.5664/jcsm.7172
- Riemann, D., Baglioni, C., Bassetti, C., Bjorvatn, B., Dolenc Groselj, L., & Ellis, J. et al. (2017). European guideline for the diagnosis and treatment of insomnia. Journal Of Sleep Research, 26(6), 675-700. https://doi.org/10.1111/jsr.12594
- Gandotra, K., Chen, P., Jaskiw, G., Konicki, P., & Strohl, K. (2018). Effective Treatment of Insomnia With Mirtazapine Attenuates Concomitant Suicidal Ideation. Journal Of Clinical Sleep Medicine, 14(05), 901-902. https://doi.org/10.5664/jcsm.7142
Also Read: NURS 6650 Week 2 Family Assessment and Phases of Family Therapy
READ MORE >>
Assignment: Real-World Case 21.1Assignment: Real-World Case 21.1Kelly was a new ...
Assignment: Real-World Case 21.1
Assignment: Real-World Case 21.1
Kelly was a new coder who had never held an HIM job before. She had just graduated from college and passed her RHIT when she was hired by a local clinic and was so excited to start working. A few weeks later, her manager asked to meet with her. The manager closed the door and told Kelly that she wanted her to code charts for a particular procedure using two codes instead of one so the reimbursement would be higher.
The manager then proceeded to divulge information that the clinic was struggling financially so anything extra would help. Assignment: Real-World Case 21.1. Kelly got the impression that if she did not comply they would let her go; and she really needed this job. Also, since it was her boss asking, she felt obligated to do as she was told.

Assignment: Real-World Case 21.1 Question:
Read the Real-World Case 21.1 (at the end of Chapter 21). Summarize the case in a few words.
- What are the ethical issues associated with this case?
- Identify a few things the hospital can do to prevent the unethical behavior.
- Discuss Ms. Brown’s potential ethical cultural shock by learning who she was and meeting family and friends who she does not remember. Think in terms of religion and cultural bias or prejudices.
Assignment: Real-World Case 21.1 Expert Answer
This contextual analysis investigates a universe of misrepresentation and charm, revealing and clarifying the reasons for work environment issues and questionable works on lying behind the happy veneer of business neighborliness. Such an investigation…
Real-World Case 21.1
Kelly was a new coder who had never held an HIM job before. She had just graduated from college and passed her RHIT when she was hired by a local clinic and was so excited to start working. A few weeks later, her manager asked to meet with her. The manager closed the door and told Kelly that she wanted her to code charts for a particular procedure using two codes instead of one so the reimbursement would be higher.
The manager then proceeded to divulge information that the clinic was struggling financially, so anything extra would help. Kelly got the impression that if she did not comply, they would let her go, and she really needed this job. Assignment: Real-World Case 21.1. Also, since it was her boss asking, she felt obligated to do as she was told.
Assignment: Real-World Case 21.1 Question:
Read the Real-World Case 21.1 (at the end of Chapter 21). Summarize the case in a few words.
- What are the ethical issues associated with this case?
- Identify a few things the hospital can do to prevent unethical behavior.
- Discuss Ms. Brown’s potential ethical cultural shock by learning who she was and meeting family and friends who she does not remember. Think in terms of religion and cultural bias or prejudices.
Assignment: Real-World Case 21.1 Expert Answer:
This contextual analysis investigates a universe of misrepresentation and charm, revealing and clarifying the reasons for work environment issues and questionable works lying behind the happy veneer of business neighborliness.
READ MORE >>
and provide two scholarly resources in support of your policy or practice recom ...
READ MORE >>
NURS 6053 Discussion Review of Current Healthcare Issues Example Solution Includ ...
NURS 6053 Discussion Review of Current Healthcare Issues Example Solution Included
If you were to ask 10 people what they believe to be the most significant issue facing healthcare today, you might get 10 different answers. Escalating costs? Regulation? Technology disruption?
These and many other topics are worthy of discussion. Not surprisingly, much has been said in the research, within the profession, and in the news about these topics. Whether they are issues of finance, quality, workload, or outcomes, there is no shortage of changes to be addressed.
In this Discussion, you examine a national healthcare issue and consider how that issue may impact your work setting. You also analyze how your organization has responded to this issue.
To Prepare:
- Review the Resources and select one current national healthcare issue/stressor to focus on.
- Reflect on the current national healthcare issue/stressor you selected and think about how this issue/stressor may be addressed in your work setting.
BY DAY 3 OF WEEK 1
Post a description of the national healthcare issue/stressor you selected for analysis, and explain how the healthcare issue/stressor may impact your work setting. Then, describe how your health system work setting has responded to the healthcare issue/stressor, including a description of what changes may have been implemented. Be specific and provide examples.
By Day 6 of Week 1
Respond to at least two of your colleagues on two different days who chose a different national healthcare issue/stressor than you selected. Explain how their chosen national healthcare issue/stressor may also impact your work setting and what (if anything) is being done to address the national healthcare issue/stressor.
NURS 6053 Discussion Review of Current Healthcare Issues Example Approach
I currently work as regional manager for a large company that oversees doctors’ offices. One of the main issues that affect us greatly is the rising cost of medication and patient compliance. There are many reasons healthcare cost rise. One reason is “The way the system is structured now, it is a cure-driven system, not a prevention-driven system,” (Morabito 2022) This statement means that we focus on fixing a problem rather than preventing the problem.
My company has created a new position within the company to monitor patients and to ensure the follow up in office for preventative procedures. The position is care managers the care managers call patients routinely monitoring for any disease exacerbation, schedule them for follow up appointments after ER, or hospital stays, and routine visits. It is said that the benefits of preventive health care are narrowly defined in terms of reductions in future morbidity and mortality.
Thus it is normally assumed that it is the final health gains alone which bear utility (Salkeld). If patients are diligent about frequenting their physician offices to get routine test, labs and procedures as well as maintaining a balanced diet many health disparities will ne prevented. Getting preventive care reduces the risk for diseases, disabilities, and death — yet millions of people in the United States don’t get recommended preventive health care services (Borsky).
Borksy, A., et al. (2018). Few Americans Receive All High-Priority, Appropriate Clinical Preventive Services. Health Affairs, 37(6).
Charlotte Morabito February 28, 2022 “Why health-care costs are rising in the U.S. more than anywhere else” retrieved on November 28, 2022 from https://www.cnbc.com/2022/02/28/why-health-care-costs-are-rising-in-the-us-more-than-anywhere-else-.htmlLinks to an external site.
Salkeld G. (1998). What are the benefits of preventive health care?. Health care analysis : HCA : journal of health philosophy and policy, 6(2), 106–112. https://doi.org/10.1007/BF02678116
Kristine Joy Example 2
One of the main healthcare issues right now is nursing shortage. In my current workplace we are often understaffed. I work in a COVID unit and one reason nurses do not stay is staff burnout. Thus, our hospital is hiring travel nurses to fill up these positions and also partnering up with local universities and colleges that offers nursing programs to encourage new graduates to apply at the hospital in exchange of loan reimbursement. The same is offered with current staff that wants to pursue further education in exchange for a work contract.
First and foremost, hospitals and other health care facilities must immediately invest in retaining our current nursing workforce. Burnout associated with COVID-19 working conditions and post-traumatic stress disorder is leading to an exodus of nurses. Some nurses are choosing to retire; others are abandoning hometown hospitals for more lucrative traveler positions. Some nurses are leaving the profession altogether (Washington Nurse, 2021).
According to the American Nurses Association (ANA): “By 2022, there will be far more registered nurse jobs available than any other profession, at more than 100,000 per year. With more than 500,000 seasoned RNs anticipated to retire by 2022, the U.S. Bureau of Labor Statistics projects the need for 1.1 million new RNs for expansion and replacement of retirees, and to avoid a nursing shortage.”
In 2014, Thomas Bodenheimer, MD, and Christine Sinsky, MD, published an article reporting that staff burnout and dissatisfaction are associated with lower patient satisfaction, reduced health outcomes, and potentially increased costs. They recommended that organizations adopt the quadruple aim, citing that the fourth aim, improving the work life of health care clinicians and staff, is necessary to achieve the triple aim.
The authors noted that the work environment has a significant impact on employee well-being, and employees with poor well-being were less engaged and more negative about the workplace (Jacobs et al., 2018). Even the most perfectly designed delivery system will become dysfunctional if the leaders of the team lack the energy or desire to effectively carry out their responsibilities. Each staff member should feel fully engaged in support of the healthcare organizational mission. This enhances continuity of care, adding to the momentum of patient engagement.
References
COVID-19 INTENSIFIES THE NATIONAL NURSING SHORTAGE: For years, national nursing leaders and health care experts warned of a looming nursing shortage… Add a global pandemic, and that shortage is here. (2021). Washington Nurse, 51(3), 22–23.
Epperson, W. J., Childs, S. F., & Wilhoit, G. (2021). Provider Burnout and Patient Engagement: The Quadruple and Quintuple Aims. Physician Leadership Journal, 8(2), 72–76.
Jacobs, B., McGovern, J. , Heinmiller, J. & Drenkard, K. (2018). Engaging Employees in Well-Being. Nursing Administration Quarterly, 42 (3), 231-245.
ANALYSIS OF A PERTINENT HEALTHCARE ISSUE
The Quadruple Aim provides broad categories of goals to pursue to maintain and improve healthcare. Within each goal are many issues that, if addressed successfully, may have a positive impact on outcomes. For example, healthcare leaders are being tasked to shift from an emphasis on disease management often provided in an acute care setting to health promotion and disease prevention delivered in primary care settings. Efforts in this area can have significant positive impacts by reducing the need for primary healthcare and by reducing the stress on the healthcare system.
Changes in the industry only serve to stress what has always been true; namely, that the healthcare field has always faced significant challenges, and that goals to improve healthcare will always involve multiple stakeholders. This should not seem surprising given the circumstances. Indeed, when a growing population needs care, there are factors involved such as the demands of providing that care and the rising costs associated with healthcare. Generally, it is not surprising that the field of healthcare is an industry facing multifaceted issues that evolve over time.
In this module’s Discussion, you reviewed some healthcare issues/stressors and selected one for further review. For this Assignment, you will consider in more detail the healthcare issue/stressor you selected. You will also review research that addresses the issue/stressor and write a white paper to your organization’s leadership that addresses the issue/stressor you selected.
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
WEEKLY RESOURCES
To Prepare:
- Review the national healthcare issues/stressors presented in the Resources and reflect on the national healthcare issue/stressor you selected for study.
- Reflect on the feedback you received from your colleagues on your Discussion post for the national healthcare issue/stressor you selected.
- Identify and review two additional scholarly resources (not included in the Resources for this module) that focus on change strategies implemented by healthcare organizations to address your selected national healthcare issue/stressor.
The Assignment (2-3 Pages):
Analysis of a Pertinent Healthcare Issue
Develop a 2 to 3 page paper, written to your organization’s leadership team, addressing your selected national healthcare issue/stressor and how it is impacting your work setting. Be sure to address the following:
- Describe the national healthcare issue/stressor you selected and its impact on your organization. Use organizational data to quantify the impact (if necessary, seek assistance from leadership or appropriate stakeholders in your organization).
- Provide a brief summary of the two articles you reviewed from outside resources on the national healthcare issue/stressor. Explain how the healthcare issue/stressor is being addressed in other organizations.
- Summarize the strategies used to address the organizational impact of national healthcare issues/stressors presented in the scholarly resources you selected. Explain how they may impact your organization both positively and negatively. Be specific and provide examples.
Looking Ahead
The paper you develop in Module 1 will be revisited and revised in Module 2. Review the Assignment instructions for Module 2 to prepare for your revised paper.
NURS_6053_Module01_Week02_Assignment_Rubric
NURS_6053_Module01_Week02_Assignment_Rubric
Criteria Ratings Pts
This criterion is linked to a Learning OutcomeDevelop a 2-3 page paper, written to your organization’s leadership team, addressing the selected national healthcare issue/stressor and how it is impacting your work setting. Be sure to address the following: · Describe the national healthcare issue/stressor you selected and its impact on your organization. · Use organizational data to quantify the impact (if necessary, seek assistance from leadership or appropriate stakeholders in your organization).
25 to >22.0 pts
Excellent
The response accurately and thoroughly describes the national healthcare issue/stressor selected and its impact on an organization. …The response includes accurate, clear, and detailed evidence/data to quantify the impact of the national healthcare issue/stressor selected.
22 to >19.0 pts
Good
The response describes the national healthcare issue/stressor selected and its impact on an organization. …The response includes accurate data to quantify the impact of the national healthcare issue/stressor selected.
19 to >17.0 pts
Fair
The response inaccurately or vaguely describes the national healthcare issue/stressor selected and its impact on an organization. …The response includes vague or inaccurate data to quantify the impact of the national healthcare issue/stressor selected.
17 to >0 pts
Poor
The response inaccurately and vaguely describes the national healthcare issue/stressor selected and its impact on an organization or is missing. …The response includes vague and inaccurate data to quantify the impact of the national healthcare issue/stressor selected or is missing.
25 pts
This criterion is linked to a Learning Outcome· Provide a summary of the two articles you reviewed from outside resources, on the national healthcare issue/stressor. · Explain how the healthcare issue/stressor is being addressed in other organizations.
30 to >26.0 pts
Excellent
Response includes a complete, detailed, and specific summary of two outside resources (articles) reviewed on the national healthcare issue/stressor selected. …The response accurately and thoroughly explains in detail how the healthcare issue/stressor is being addressed in other organizations.
26 to >23.0 pts
Good
Response includes an accurate summary of two outside resources (articles) reviewed on the national healthcare issue/stressor selected. …The response explains how the healthcare issue/stressor is being addressed in other organizations.
23 to >20.0 pts
Fair
Response includes a vague or inaccurate or incomplete summary of outside resources (articles) reviewed on the national healthcare issue/stressor selected. …The response vaguely or inaccurately explains how the healthcare issue/stressor is being addressed in other organizations.
20 to >0 pts
Poor
Response provides a vague and inaccurate summary of outside resources (articles) reviewed on the national healthcare issue/stressor selected or summary is missing. …The response vaguely and inaccurately explains how the healthcare issue/stressor is being addressed in other organizations or explanation is missing.
30 pts
This criterion is linked to a Learning Outcome· Summarize the strategies used to address the organizational impact of national healthcare issues/stressors presented in the scholarly resources you selected. · Explain how the strategies may impact your organization both positively and negatively. Be specific and provide examples.
25 to >22.0 pts
Excellent
Response includes a complete, detailed, and accurate summary of the strategies used to address the organizational impact of the national healthcare issue/stressor. …Response accurately and thoroughly explains how the strategies may impact an organization both positively and negatively, with specific and accurate examples for each.
22 to >19.0 pts
Good
Response includes an accurate summary of the strategies used to address the organizational impact of the national healthcare issue/stressor. …Response explains how the strategies may impact an organization both positively and negatively with at least one specific example for each.
19 to >17.0 pts
Fair
Response includes a vague or inaccurate summary of the strategies used to address the organizational impact of the national healthcare issue/stressor. …Response vaguely or inaccurately explains how the strategies may impact an organization both positively and negatively. …Response may include some vague or inaccurate examples.
17 to >0 pts
Poor
Response provides a vague and inaccurate summary of the strategies used to address the organizational impact of the national healthcare issue/stressor or summary is missing. …Response vaguely and inaccurately explains how the strategies may impact an organization both positively and negatively or explanation is missing. …Response does not include any examples.
25 pts
This criterion is linked to a Learning OutcomeResource Synthesis
5 to >4.0 pts
Excellent
Using proper in-text citations, the response fully integrates at least 2 outside resources and 2 or 3 course-specific resources.
4 to >3.0 pts
Good
Using proper in-text citations, the response fully integrates at least 2 outside resources and 1 course-specific resource.
3 to >2.0 pts
Fair
Using proper in-text citations, the response minimally integrates outside and course-specific resources.
2 to >0 pts
Poor
The response does not integrate outside and course-specific resources or no in-text citations are used.
5 pts
This criterion is linked to a Learning Outcome Written Expression and Formatting—Paragraph Development and Organization: Paragraphs make clear points that support well-developed ideas, flow logically, and demonstrate continuity of ideas. Sentences are carefully focused—neither long and rambling nor short and lacking substance. A clear and comprehensive purpose statement and introduction is provided, which delineates all required criteria.
5 to >4.0 pts
Excellent
Paragraphs and sentences follow writing standards for flow, continuity, and clarity. …A clear and comprehensive purpose statement, introduction, and conclusion are provided, which delineates all required criteria.
4 to >3.0 pts
Good
Paragraphs and sentences follow writing standards for flow, continuity, and clarity 80% of the time. …Purpose, introduction, and conclusion of the assignment are stated but are brief and not descriptive.
3 to >2.0 pts
Fair
Paragraphs and sentences follow writing standards for flow, continuity, and clarity 60–79% of the time. …Purpose, introduction, and conclusion of the assignment is vague or off topic.
2 to >0 pts
Poor
Paragraphs and sentences follow writing standards for flow, continuity, and clarity less than 60% of the time. …No purpose statement, introduction, or conclusion is provided.
5 pts
This criterion is linked to a Learning Outcome Written Expression and Formatting—English Writing Standards: Correct grammar, mechanics, and proper punctuation.
5 to >4.0 pts
Excellent
Uses correct grammar, spelling, and punctuation with no errors.
4 to >3.0 pts
Good
Contains a few (one or two) grammar, spelling, and punctuation errors.
3 to >2.0 pts
Fair
Contains several (three or four) grammar, spelling, and punctuation errors.
2 to >0 pts
Poor
Contains many (five or more) grammar, spelling, and punctuation errors that interfere with the reader’s understanding.
5 pts
This criterion is linked to a Learning Outcome Written Expression and Formatting: The paper follows correct APA format for title page, headings, font, spacing, margins, indentations, page numbers, running head, parenthetical/in-text citations, and reference list.
5 to >4.0 pts
Excellent
Uses correct APA format with no errors.
4 to >3.0 pts
Good
Contains a few (one or two) APA format errors.
3 to >2.0 pts
Fair
Contains several (three or four) APA format errors.
2 to >0 pts
Poor
Contains many (five or more) APA format errors.
5 pts
Total Points: 100
NURS 6053 MODULE 2 DISCUSSION – ORGANIZATIONAL POLICIES AND PRACTICES TO SUPPORT HEALTHCARE ISSUES
Quite often, nurse leaders are faced with ethical dilemmas, such as those associated with choices between competing needs and limited resources. Resources are finite, and competition for those resources occurs daily in all organizations.
For example, the use of 12-hour shifts has been a strategy to retain nurses. However, evidence suggests that as nurses work more hours in a shift, they commit more errors. How do effective leaders find a balance between the needs of the organization and the needs of ensuring quality, effective, and safe patient care?
In this Discussion, you will reflect on a national healthcare issue and examine how competing needs may impact the development of polices to address that issue.
To Prepare:
- Review the Resources and think about the national healthcare issue/stressor you previously selected for study in Module 1.
- Reflect on the competing needs in healthcare delivery as they pertain to the national healthcare issue/stressor you previously examined.
BY DAY 3 OF WEEK 3
Post an explanation of how competing needs, such as the needs of the workforce, resources, and patients, may impact the development of policy. Then, describe any specific competing needs that may impact the national healthcare issue/stressor you selected. What are the impacts, and how might policy address these competing needs? Be specific and provide examples.
BY DAY 6 OF WEEK 3
Respond to at least two of your colleagues on two different days by providing additional thoughts about competing needs that may impact your colleagues’ selected issues, or additional ideas for applying policy to address the impacts described.
LEARNING RESOURCES
Required Readings
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statementsLinks to an external site.. Silver Spring, MD: Author. Retrieved fromhttps://www.nursingworld.org/coe-view-onlyNote: Review all, with special attention to “Provision 6” (pp. 23–26).
- Kelly, P., & Porr, C. (2018). Ethical nursing care versus cost containment: Considerations to enhance RN practiceLinks to an external site.. OJIN: Online Journal of Issues in Nursing, 23(1), Manuscript 6. doi:10.3912/OJIN.Vol23No01Man06. Retrieved fromhttp://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-23-2018/No1-Jan-2018/Ethical-Nursing-Cost-Containment.html
- Milliken, A. (2018). Ethical awareness: What it is and why it mattersLinks to an external site.. OJIN: Online Journal of Issues in Nursing, 23(1), Manuscript 1. doi:10.3912/OJIN.Vol23No01Man01. Retrieved fromhttp://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-23-2018/No1-Jan-2018/Ethical-Awareness.html
Required Media
- Walden University, LLC. (Producer). (2012). Ethical, Moral, and Legal Leadership [Video file]. Baltimore, MD: Author.
https://waldenu.instructure.com/courses/21534/external_tools/retrieve?display=borderless&url=https%3A%2F%2Fwaldencanvasprod.kaf.kaltura.com%2Fbrowseandembed%2Findex%2Fmedia%2Fentryid%2F1_66j2ra6d%2FshowDescription%2Ffalse%2FshowTitle%2Ffalse%2FshowTags%2Ffalse%2FshowDuration%2Ffalse%2FshowOwner%2Ffalse%2FshowUploadDate%2Ffalse%2FplayerSize%2F766x431%2FplayerSkin%2F51364222%2F
- Walden University, LLC. (Producer). (2009b). Working with Individuals [Video file]. Baltimore, MD: Author.
https://waldenu.instructure.com/courses/21534/external_tools/retrieve?display=borderless&url=https%3A%2F%2Fwaldencanvasprod.kaf.kaltura.com%2Fbrowseandembed%2Findex%2Fmedia%2Fentryid%2F1_7u5n3hb6%2FshowDescription%2Ffalse%2FshowTitle%2Ffalse%2FshowTags%2Ffalse%2FshowDuration%2Ffalse%2FshowOwner%2Ffalse%2FshowUploadDate%2Ffalse%2FplayerSize%2F766x431%2FplayerSkin%2F51364222%2F
ORGANIZATIONAL POLICIES AND PRACTICES TO SUPPORT HEALTHCARE ISSUES SAMPLE SOLUTION 1 Chloe
When discussing the topic of patient advocacy, it is vital for nurses to know their role and responsibility to help achieve this significant aspect of healthcare. With national nursing shortages, nurses are being pulled in multiple directions throughout their shift and their ability to truly be present with their patient and form a trusting relationship has become compromised.
Despite how busy they are, nurses always have the duty to stand up for their patients and ensure that their concerns, wants, and needs are addressed. According to Milliken (2018), “Nurses must first recognize the potential ethical repercussions of their actions in order to effectively resolve problems and address patient needs” (para. 2). In other words, it is imperative for nurses to understand their ethical obligation to advocate for their patients.
A policy that is greatly impacting patient advocacy is nurse staffing. Clarke and Donaldson (2008) write, “Nursing is a critical factor in determining the quality of care in hospitals and the nature of patient outcomes. Nurse staffing is a crucial health policy issue on which there is a great deal of consensus on an abstract level (that nurses are an important component of the health care delivery system and that nurse staffing has impacts on safety” (para. 1).
Not only is the nursing shortage an issue for patient advocacy, it is an issue regarding patient safety as well. Griffiths et. al. (2018) analyzed the relationship between nurse staffing levels and patient outcomes and found that “omissions of nursing care (referred as missed care, care left undone or rationed care) have been proposed as a factor which may provide a more direct indicator of nurse staffing adequacy” (para. 2). This relates to patient advocacy because by omitting care, nurses are not fulfilling certain aspects of care that patients deserve to receive. One way to address the issue of failing patient advocacy is to first address the national nursing shortage.
References
Clarke SP, Donaldson NE. Nurse Staffing and Patient Care Quality and Safety. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 25. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2676/Links to an external site.
Griffiths P, Recio-Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, Smith GB, Ball J; Missed Care Study Group. The association between nurse staffing and omissions in nursing care: A systematic review. J Adv Nurs. 2018 Jul;74(7):1474-1487. doi: 10.1111/jan.13564. Epub 2018 Apr 23. PMID: 29517813; PMCID: PMC6033178.
Milliken, A. (2018). Ethical awareness: What it is and why it matters Links to an external site.Links to an external site.. OJIN: Online Journal of Issues in Nursing, 23(1), Manuscript 1. doi:10.3912/OJIN.Vol23No01Man01. Retrieved fromhttp://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-23-2018/No1-Jan-2018/Ethical-Awareness.htmlLinks to an external site.
ORGANIZATIONAL POLICIES AND PRACTICES TO SUPPORT HEALTHCARE ISSUES SAMPLE SOLUTION 2 – Elizabeth T
Competing needs in healthcare can include the needs of patients, the workforce, and resources that may impact policy development. The competing needs should work with the policy and not against it. The health of nurse work environments is the focus of my discussion. Work environment health has been shown to affect both patient and nurse outcomes.
A part of the quadruple aim is that nurses feel joy and find fulfillment in their work. This healthy workplace environment translates into job satisfaction, decreased burnout, and improved patient care outcomes. A healthy work environment enables nurses to provide the highest standards of compassionate patient care while being fulfilled at work (Ulrich et al., 2022).
As a result of the COVID-19 pandemic, early studies have found that nurses are fearful, distressed, and traumatized; many intend to leave the profession. In research by Zhao et al., nurses in China who provided direct patient care during the worst outbreak phase experienced significant psychological distress.
Still, their work environments could mitigate psychological distress. Less distressed nurses had managers with an inclusive leadership style. Inclusive leaders involved their staff in decisions, a form of empowerment that created workplace environments that were perceived to be mentally healthy.
Before the pandemic, the nursing workforce was already under strain. The challenge will be creating conditions to maintain and sustain a healthy nursing workforce. This challenge begins with nurse and healthcare leaders whose leadership and management styles create healthy, productive workplace environments for their staff and whose leadership values align with the models of nursing care that they are promoting (Gottlieb et al., 2021).
Nurses’ job satisfaction and psychological, emotional, and physical health are related to autonomy, agency, and empowerment. These factors are affected by nurse leadership, the culture in their units and their organization, and the opportunities created for staff. Nurse managers can facilitate empowering work conditions and promote collaborative inter-professional and intra-professional relationships (Gottlieb et al., 2021).
Policies must seek to empower their staff and provide autonomy and agency. Resources must be provided for education for both staff and managers. Resources can prove challenging. Encouraging managers and staff to collaborate and provide time for such may also seem daunting, but in the end, it will be worth the expense of a healthy, happy staff and improved patient outcomes.
Gottlieb, L. N., Gottlieb, B., & Bitzas, V. (2021). Creating Empowering Conditions for Nurses with Workplace Autonomy and Agency: How Healthcare Leaders Could Be Guided by Strengths-Based Nursing and Healthcare Leadership (SBNH-L). Journal of Healthcare Leadership, Volume 13, 169–181. https://doi.org/10.2147/jhl.s221141Links to an external site.
Ulrich, B., Cassidy, L., Barden, C., Varn-Davis, N., & Delgado, S. A. (2022). National Nurse Work Environments – October 2021: A Status Report. Critical Care Nurse, 42(5), 58–70. https://doi.org/10.4037/ccn2022798Links to an external site.
Zhao, F., Ahmed, F., & Faraz, N. A. (2020). Caring for the caregiver during COVID-19 outbreak: Does inclusive leadership improve psychological safety and curb psychological distress? A cross-sectional study. International journal of nursing studies, 110, 103725. https://doi.org/10.1016/j.ijnurstu.2020.103725
Module 2: ASSIGNMENT DEVELOPING ORGANIZATIONAL POLICIES AND PRACTICES
Competing needs arise within any organization as employees seek to meet their targets and leaders seek to meet company goals. As a leader, successful management of these goals requires establishing priorities and allocating resources accordingly.
Within a healthcare setting, the needs of the workforce, resources, and patients are often in conflict. Mandatory overtime, implementation of staffing ratios, use of unlicensed assisting personnel, and employer reductions of education benefits are examples of practices that might lead to conflicting needs in practice.
Leaders can contribute to both the problem and the solution through policies, action, and inaction. In this Assignment, you will further develop the white paper you began work on in Module 1 by addressing competing needs within your organization.
To Prepare:
- Review the national healthcare issue/stressor you examined in your Assignment for Module 1, and review the analysis of the healthcare issue/stressor you selected.
- Identify and review two evidence-based scholarly resources that focus on proposed policies/practices to apply to your selected healthcare issue/stressor.
- Reflect on the feedback you received from your colleagues on your Discussion post regarding competing needs.
The Assignment (1-2 pages):
Developing Organizational Policies and Practices
Add a section to the 2-3
READ MORE >>
SOC 445 Week 2 Assignment Topic 2: Ethics in Social Work WorksheetAssignment T ...
SOC 445 Week 2 Assignment Topic 2: Ethics in Social Work Worksheet
Assignment Topic 2: Ethics in Social Work Worksheet
Assignment Topic 2: Ethics in Social Work Worksheet Directions:
Complete the “Ethics in Social Work” worksheet using the NASW Code of Ethics to justify your responses. Be sure to cite the specific section(s) of the code utilized in each scenario.
Scenario 1:
A representative from “Canyon Smiles” dentist’s office comes to your agency to make a presentation about their services. You are surprised to see Bethanie; an old friend from high school is now working for “Canyon Smiles” and will be the one making the presentation Assignment Topic 2: Ethics in Social Work Worksheet.
During the presentation you learn the dentist’s office recently opened a new location that is really close to your house. This is important because you predominately work from home so this location would work best for you Assignment Topic 2: Ethics in Social Work Worksheet.
Everyone in the office very gets excited when Bethanie tells them: “Every case manager, who brings in a new client, will be entered into a drawing to win a brand new IPad! Don’t worry, she says, it is perfectly legal!” At the end of the meeting Bethanie pulls you aside and ask if you want to go lunch and catch up!
In 200-300 words, explain all the ethical situations that may arise out of the above scenario. Explain what you would do as case manager and why. Make sure to cite the NASW Code of Ethics in your explanation. Also, explain what else you could do to clarify ethical dilemmas in this situation that are not clear in the code of ethics.
ORDER COMPREHENSIVE SOLUTION PAPERS ON Assignment Topic 2: Ethics in Social Work Worksheet
Scenario 2(a):
You are shopping one Sunday afternoon at one of your favorite stores when you run into a current client of yours. After some simple chit-chat, about the store’s “special” that day, your client asks if you want to head on over to the food court to have lunch. You need to eat and was actually thinking about going over to the food court yourself, before your client mentioned it.
In 100-150 words, Explain what you would do as Case Manager and why? Make sure to cite the N.A.S.W Code of Ethics in your response Assignment Topic 2: Ethics in Social Work Worksheet.
Scenario 2(b):
You are shopping one Sunday afternoon at one of your favorite stores and you run into an old client of yours. After some simple chit-chat about the store’s “special” that day, and how well they are doing at their new job, the client asks if you want to head on over to the food court to have lunch. You need to eat and was actually thinking about going over to the food court yourself, before your client mentioned it.
In 100-150 words, Explain what you would do as case manager and why. Make sure to cite the NASW Code of Ethics in your response.
Scenario 3:
After graduating from college, you apply for and are offered a program manager position with a social service agency. Your primary responsibility is to develop a volunteer program that includes increasing donations & volunteerism for your clients and your program Assignment Topic 2: Ethics in Social Work Worksheet.
One week into your new job, you learn the program only has one volunteer group, that is part of a church, but they are on hiatus because of a bad experience between them, clients, and the agency. Wanting to repaper this damaged relationship you invite the members of the group into the office to discuss the situation and a plan for going forward. Assignment Topic 2: Ethics in Social Work Worksheet
During the meeting you learn that the leader of the group does not believe “everyone” in the group needs to poses a valid DPS Level One Fingerprint Clearance Card because he has one and he can vouch for everyone else in the group. The policy of the agency is that every volunteer, who interacts with clients more than one time, is required to possess a valid DPS Level One Fingerprint Clearance Card.
The leader of the group fears the card requirement will discourage volunteers from staying in/ joining the group because the cards cost $65 dollars each! The leader is unsure if he wants the group to continue because it is always hard to find volunteers willing to pay the $65 for the clearance card.
This group’s church donates $5,000 to your program every year. They sponsor your programs largest donation drive every year! In addition, the time they spend with your clients is given a monetary value and then matched by another donor source. In short, this group is the single largest private contributor to your program Assignment Topic 2: Ethics in Social Work Worksheet.
In 200-300 words, explain all the ethical situations that may arise out of the above scenario. Explain what you would do as case manager and why. Make sure to cite the NASW Code of Ethics in your explanation. Also, explain what else you could do to clarify ethical dilemmas in this situation that are not clear in the code of ethics. Assignment Topic 2: Ethics in Social Work Worksheet
SOC-445 Case Management Sample Essay Paper
Brian is a male in his mid 30’s that has an addiction to heroin and was found by his son when he overdosed. The mother of his child, who is also his wife, had to use Narcan to revive him. The mother of his child claims that he is worthless and needs to man up as she states.
The child wants nothing to do with him because of what he saw the day his father overdosed, Brian claims that they would do everything together but now cannot look at him or even be in the same room. Brian feels useless and wants to do better but it seems he is suffering from depression and needs much attention to his mental health. Assignment Topic 2: Ethics in Social Work Worksheet
I would recommend outpatient treatment and family therapy. I would also recommend the child receive therapy as well due to the trauma he has experienced at home. The family would need much therapy and marriage counseling would be necessary to see where Brian and his wife can fix their marriage.
After Brian’s assessment I would consult with professionals such as my supervisor and other social workers to see if they believe that any other services should be given besides the ones I would be referring to.
I will be referring Brian to an outpatient program for substance abuse along with treatment for his depression. Brian will be removed from his home for the time of his treatment until completed. The reason for his removal is for the safety of his son which will be undergoing therapy for his emotional and mental state.
I will be contacting the wife with the permission of Brian to speak to his wife to get more insight of what she believes Brian can improve or get help in. When family is involved in treatment the chances of a client relapsing is less than someone that has no support Assignment Topic 2: Ethics in Social Work Worksheet.
Families receive agency support to remain involved with their family member whenever possible and receive the support they need to remain an intact family. Agencies that work to enable the identified client to live successfully in their community have found that individuals do much better if their families have not cut them off”.(Summer,2020)
Marty is a male in his 60’s and is a Vietnam Vet and suffers from depression and tries to suppress it by a large consumption of alcohol. Marty has no stable place to live so he stays with whoever will lend him a place to sleep for the night or sleeps outside Assignment Topic 2: Ethics in Social Work Worksheet.
Marty goes to VA hospital where he is provided money. When given that money he drinks with his two best friends which are two bottles of aholo everyday. Marty believes that his life is not worth living out of the guilt he feels for making it home while his friends died in war. He believes they are better off and says so to them when he has his nightmares at night which leads to the large consumption of alcohol the next day.
ORDER COMPREHENSIVE SOLUTION PAPERS
Marty will do much better in an inpatient program where there is around the clock care. The inpatient program will consist of five day treatment for alcoholics along with mental health treatment for his severe depression Assignment Topic 2: Ethics in Social Work Worksheet. The reason why I believe that inpatient will be the best fit is because Marty has no means of transportation to get to and from any programs given along the inpatient treatment facility will help Marty with housing upon completion of his programs while admitted into treatment. I will be making my referrals as soon as possible as Marty’s mental health has been left untreated for too long and is progressing along with his alcohol abuse.
The similarities that Marty and Brain have are they are two males that suffer from depression and feel like they are worthless. Marty and Brian both have relationship issues; one cannot keep a relationship because he feels unworthy of love and one feels worthless in his relationship because he cannot provide for his family. They both need programs to address their abuse of alcohol and drugs. Short term goals will be best for the both as they both will feel overwhelmed if too much pressure was put onto them at once.
The differences in Mrty and Brain is that one has the support of his family once he completes his treatment and is allowed in his home. Marty only has himself because his family doesn’t trust him ever since he came back from war. Assignment Topic 2: Ethics in Social Work Worksheet
Marty will be referred to inpatient and Brain into outpatient treatment programs. The way I will support Marty as a friend is by making sure his mental state is safe to be on his own. I will not leave Marty unless he will be going into his treatment program. As a social worker I will call men shelters to see if there is a bed available until his bed is secured in his inpatient program so he does not change his mind and he gets the help he needs Assignment Topic 2: Ethics in Social Work Worksheet.
The way I will help Brian as a friend is I will allow Brian to stay in my home so he can have a safe place to stay because the embarrassment might come on too heavy as too what happened around his son and wife. As a social worker I will have him contact family that he may stay with until he is cleared to go back into his home upon completion of his program.
The only challenges that I may face is the struggle that may come across with Marty and Brian will be out of embarrassment and the amount of the depression that they both face. They are both ready and willing to change and want the help that I can provide and the services that can be given upon request. Mental health is suffered by many people in today’s society.
The unfortunate situation is that not many come forward asking for the help and commit suidcide as their only way out. We need more support in the mental health community together we stand divided we fall. Assignment Topic 2: Ethics in Social Work Worksheet
Assignment Topic 2: Ethics in Social Work Worksheet Reference:
Summers, N. (2015). Fundamentals of case management practice (5th ed.). Boston, MA: Cengage Learning. ISBN-13: 9781305094765.
URL:
http://gcumedia.com/digital-resources/cengage/2015/fundamentals-of-case-management-practice_skills-for-the-human-services_ebook_5e.php
“Ethnic Differences in Mental Health Service Use Among Patients With Psychotic Disorders,” by Mohan et al., from Social Psychiatry and Psychiatric Epidemiology (2006).
URL:
https://lopes.idm.oclc.org/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=edswss&AN=000240913600002&site=eds-live&scope=site
READ MORE >>
you will study a recent nursing informatics-related healthcare policy ...
READ MORE >>
The Nurse Leader as Knowledge Worker NURS 6051 Example 1The Concept of a Knowled ...
The Nurse Leader as Knowledge Worker NURS 6051 Example 1
The Concept of a Knowledge Worker
- Employs intellect to analyze, create, and share valuable information.
- Utilizes expertise to solve complex problems and make informed decisions.
- Relies on continuous learning and innovation for professional growth.
- Leverages technology to access, organize, and disseminate knowledge effectively.
- Collaborates with multidisciplinary teams to improve patient outcomes and care.
- Drives evidence-based practices and fosters a culture of lifelong learning.
(Garcia-Dia, 2021)
Nursing Informatics – Definition and Explanation
- Integration of nursing science, computer science, and information science.
- Enhances healthcare through data management, knowledge dissemination, and technology.
- Improves patient care, safety, and outcomes through evidence-based practice.
- Utilizes technology to collect, analyze, and interpret healthcare data.
- Supports decision-making, research, and quality improvement in nursing practice.
- Optimizes information systems to streamline workflows and enhance communication
- (Kianto et al., 2019)
Nurse Leader as a Knowledge Worker
- Strategically integrates evidence-based practices into nursing leadership.
- Promotes continuous learning and professional development among the team.
- Facilitates knowledge sharing and collaboration across healthcare disciplines.
- Utilizes data and technology to drive informed decision-making and innovation.
- Advocates for a culture of lifelong learning and evidence-based care.
- Inspires and empowers the team to embrace knowledge-driven practices.
- (Strudwick et al., 2019)
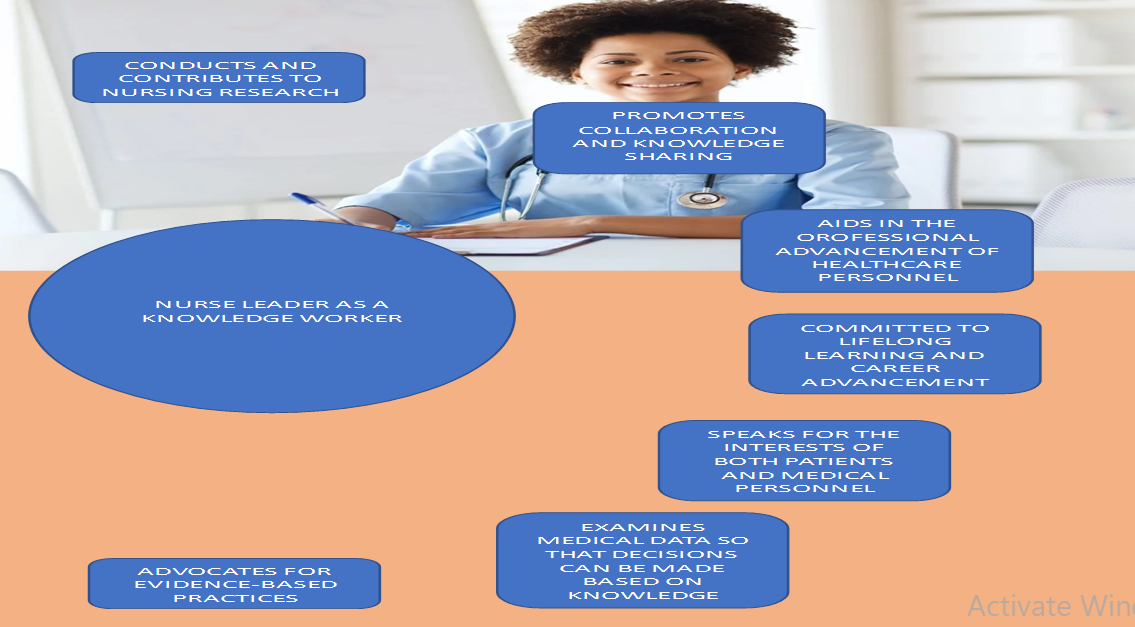
The Application of Data to Problem-Solving in Healthcare
- Examining data: Vital signs, glucose levels, physical activity, sleep patterns.
- Data collection: Wearable devices, sensors, secure transmission to a centralized database.
- Derived knowledge: Early identification, personalized treatment, proactive preventive care.
- Accessing data: Secure web portal, a mobile application for real-time monitoring.
- Clinical reasoning: Nurse leaders interpret data, consider patient context.
- Improving outcomes: Data-driven insights, evidence-based practice, process improvement.
The Nurse Leader as Knowledge Worker NURS 6051 References
Garcia-Dia, M. J. (2021). Nursing informatics: an evolving specialty. Nursing Management, 52(5), 56. https://journals.lww.com/nursingmanagement/fulltext/2021/05000/nursing_informatics__an_evolving_specialty.10.aspx
Kianto, A., Shujahat, M., Hussain, S., Nawaz, F., & Ali, M. (2019). The impact of knowledge management on knowledge worker productivity. Baltic Journal of Management, 14(2), 178-197. https://hub.hku.hk/bitstream/10722/278661/1/Content.pdf?accept=1
Strudwick, G., Nagle, L., Kassam, I., Pahwa, M., & Sequeira, L. (2019). Informatics Competencies for Nurse Leaders: A Scoping Review. The Journal of Nursing Administration, 49(6), 323–330. https://doi.org/10.1097/NNA.0000000000000760
Assignment: The Nurse Leader as Knowledge Worker NURS 6051 / NURS 5051 Instructions
Assignment: The Nurse Leader as Knowledge Worker
The term “knowledge worker” was first coined by management consultant and author Peter Drucker in his book, The Landmarks of Tomorrow (1959). Drucker defined knowledge workers as high-level workers who apply theoretical and analytical knowledge, acquired through formal training, to develop products and services. Does this sound familiar?
Nurses are very much knowledge workers. What has changed since Drucker’s time are the ways that knowledge can be acquired. The volume of data that can now be generated and the tools used to access this data have evolved significantly in recent years and helped healthcare professionals (among many others) to assume the role of knowledge worker in new and powerful ways.
In this Assignment, you will consider the evolving role of the nurse leader and how this evolution has led nurse leaders to assume the role of knowledge worker. You will prepare a PowerPoint presentation with an infographic (graphic that visually represents information, data, or knowledge. Infographics are intended to present information quickly and clearly.) to educate others on the role of nurse as knowledge worker.
Reference: Drucker, P. (1959). The landmarks of tomorrow. New York, NY: HarperCollins Publishers.
To Prepare for this The Nurse Leader as Knowledge Worker NURS 6051:
- Review the concepts of informatics as presented in the Resources.
- Reflect on the role of a nurse leader as a knowledge worker.
- Consider how knowledge may be informed by data that is collected/accessed.
The Assignment: The Nurse Leader as Knowledge Worker NURS 6051:
- Explain the concept of a knowledge worker.
- Define and explain nursing informatics and highlight the role of a nurse leader as a knowledge worker.
- Include one slide that visually represents the role of a nurse leader as knowledge worker.
- Your PowerPoint should Include the hypothetical scenario you originally shared in the Discussion Forum. Include your examination of the data that you could use, how the data might be accessed/collected, and what knowledge might be derived from that data. Be sure to incorporate feedback received from your colleagues’ responses.
By Day 7 of Week 2
Submit your completed Presentation.
Assignment: The Nurse Leader as Knowledge Worker NURS 6051 Example 2 Presentation
The Knowledge Worker
- Knowledge workers are people who use their theoretical knowledge and acquired skills through formal training to deliver productive work (Druker, 1995).
- Knowledge workers use their knowledge and skills to solve complex problems, make decisions, and provide new services.
- Knowledge workers access and synthesize information and use analytic reasoning and relevant judgments in addressing issues and new situations.
- Good communication skills and adequate motivation help knowledge workers deliver quality service.
- A professional board always governs knowledge workers
- Knowledge workers receive higher compensation due to the complex nature of their work
Nursing Informatics
- Nursing informatics combines nursing science, information science, and computer science (McGonigle & Mastrian, 2015.)
- This combination helps identify, define, manage, and communicate information, wisdom, and data in nursing practice to improve patient care.
- Nursing informatics includes bed management systems that help manage patient census and an electronic portal that allows patients to access their medical records quickly.
- Radio frequency identification is another example of nursing informatics that aids in tracking patient and caregiver activities.
- Nursing informatics is essential in increasing patient safety and promoting quality healthcare in hospital settings.
- Nursing informatics plays a vital role in training nursing staff on the use of technology, answering questions, and monitoring results.
Nursing informatics improve patient care by:
- Designing different process of treatment approaches, reviewing clinical workflow, diagnostic and treatment plans
- Measuring and analyzing different parts of organizational roles and making specific changes that help in improving patient care.
- Analyzing several data information to identify prevalent issues in healthcare organizations and provide the best solutions
- Selecting and testing new medical devices used in improving patient care.
- Providing training to other nursing staff by providing educational programs.
- Implementing information systems provides better access to evidence affecting patient safety and supports evidence-based nursing.
Role of a Nurse as a Knowledge Worker
- Nurse leaders play a crucial work in developing new treatment plans, collecting and evaluating treatment plans
- Using their autonomy and nursing experience, nursing leaders aid in broadening healthcare fields and promoting health
- Nurse leaders apply their knowledge and skills to address the needs of their patients and level up the general patient care criteria.
- Nurse leaders use their acquired integrated knowledge to solve upcoming and existing practice problems in healthcare settings.
- Nurse leaders are equipped with informatics skills that aid in developing new research on different nursing practices that help in improving outcomes of patient needs.
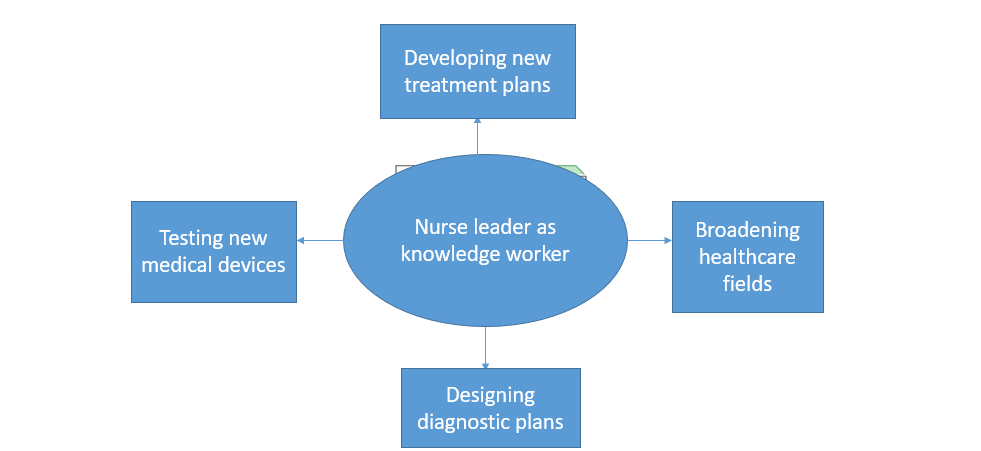
The Nurse Leader as Knowledge Worker NURS 6051 Presentation References
- Drucker, P. (1959). Landmarks of Tomorrow: A Report on the New” Post-Modern. World.
- McGonigle, D., & Mastrian, K. G. (Eds.). (2015). Nursing informatics and the foundation of knowledge. Jones & Bartlett Publishers
NURS 6051 Week 3 Discussion: Interaction Between Nurse Informaticists and Other Specialists
Nature offers many examples of specialization and collaboration. Ant colonies and bee hives are but two examples of nature’s sophisticated organizations. Each thrives because their members specialize by tasks, divide labor, and collaborate to ensure food, safety, and general well-being of the colony or hive.
Of course, humans don’t fare too badly in this regard either. And healthcare is a great example. As specialists in the collection, access, and application of data, nurse informaticists collaborate with specialists on a regular basis to ensure that appropriate data is available to make decisions and take actions to ensure the general well-being of patients.
In this Discussion, you will reflect on your own observations of and/or experiences with informaticist collaboration. You will also propose strategies for how these collaborative experiences might be improved.
To Prepare:
- Review the Resources and reflect on the evolution of nursing informatics from a science to a nursing specialty.
- Consider your experiences with nurse Informaticists or technology specialists within your healthcare organization.
By Day 3 of Week 3
Post a description of experiences or observations about how nurse informaticists and/or data or technology specialists interact with other professionals within your healthcare organization. Suggest at least one strategy on how these interactions might be improved. Be specific and provide examples. Then, explain the impact you believe the continued evolution of nursing informatics as a specialty and/or the continued emergence of new technologies might have on professional interactions.
By Day 6 of Week 3
Respond to at least two of your colleagues* on two different days, offering one or more additional interaction strategies in support of the examples/observations shared or by offering further insight to the thoughts shared about the future of these interactions.
*Note: Throughout this program, your fellow students are referred to as colleagues.
NURS 6051 Week 3 Assignment: The Impact of Nursing Informatics on Patient Outcomes and Patient Care Efficiencies
In the Discussion for this module, you considered the interaction of nurse informaticists with other specialists to ensure successful care. How is that success determined?
Patient outcomes and the fulfillment of care goals is one of the major ways that healthcare success is measured. Measuring patient outcomes results in the generation of data that can be used to improve results. Nursing informatics can have a significant part in this process and can help to improve outcomes by improving processes, identifying at-risk patients, and enhancing efficiency.
To Prepare:
- Review the concepts of technology application as presented in the Resources.
- Reflect on how emerging technologies such as artificial intelligence may help fortify nursing informatics as a specialty by leading to increased impact on patient outcomes or patient care efficiencies.
The Assignment: (4-5 pages not including the title and reference page)
In a 4- to 5-page project proposal written to the leadership of your healthcare organization, propose a nursing informatics project for your organization that you advocate to improve patient outcomes or patient-care efficiency. Your project proposal should include the following:
- Describe the project you propose.
- Identify the stakeholders impacted by this project.
- Explain the patient outcome(s) or patient-care efficiencies this project is aimed at improving and explain how this improvement would occur. Be specific and provide examples.
- Identify the technologies required to implement this project and explain why.
- Identify the project team (by roles) and explain how you would incorporate the nurse informaticist in the project team.
- Use APA format and include a title page and reference page.
- Use the Safe Assign Drafts to check your match percentage before submitting your work.
By Day 7 of Week 4
Submit your completed Project Proposal.
NURS 6051 Week 5 Discussion: Big Data Risks and Rewards
When you wake in the morning, you may reach for your cell phone to reply to a few text or email messages that you missed overnight. On your drive to work, you may stop to refuel your car. Upon your arrival, you might swipe a key card at the door to gain entrance to the facility. And before finally reaching your workstation, you may stop by the cafeteria to purchase a coffee.
From the moment you wake, you are in fact a data-generation machine. Each use of your phone, every transaction you make using a debit or credit card, even your entrance to your place of work, creates data. It begs the question: How much data do you generate each day? Many studies have been conducted on this, and the numbers are staggering: Estimates suggest that nearly 1 million bytes of data are generated every second for every person on earth.
As the volume of data increases, information professionals have looked for ways to use big data—large, complex sets of data that require specialized approaches to use effectively. Big data has the potential for significant rewards—and significant risks—to healthcare. In this Discussion, you will consider these risks and rewards.
To Prepare:
- Review the Resources and reflect on the web article Big Data Means Big Potential, Challenges for Nurse Execs.
- Reflect on your own experience with complex health information access and management and consider potential challenges and risks you may have experienced or observed.
By Day 3 of Week 5
Post a description of at least one potential benefit of using big data as part of a clinical system and explain why. Then, describe at least one potential challenge or risk of using big data as part of a clinical system and explain why. Propose at least one strategy you have experienced, observed, or researched that may effectively mitigate the challenges or risks of using big data you described. Be specific and provide examples.
By Day 6 of Week 5
Respond to at least two of your colleagues* on two different days, by offering one or more additional mitigation strategies or further insight into your colleagues’ assessment of big data opportunities and risks.
*Note: Throughout this program, your fellow students are referred to as colleagues.
Submission and Grading Information
Week 6 Discussion: Healthcare Information Technology Trends
Throughout history, technological advancements have appeared for one purpose before finding applications elsewhere that lead to spikes in its usage and development. The internet, for example, was originally developed to share research before becoming a staple of work and entertainment. But technology—new and repurposed—will undoubtedly continue to be a driver of healthcare information. Informaticists often stay tuned to trends to monitor what the next new technology will be or how the next new idea for applying existing technology can benefit outcomes.
In this Discussion, you will reflect on your healthcare organization’s use of technology and offer a technology trend you observe in your environment.
To Prepare:
- Reflect on the Resources related to digital information tools and technologies.
- Consider your healthcare organization’s use of healthcare technologies to manage and distribute information.
- Reflect on current and potential future trends, such as use of social media and mobile applications/telehealth, Internet of Things (IoT)-enabled asset tracking, or expert systems/artificial intelligence, and how they may impact nursing practice and healthcare delivery.
By Day 3 of Week 6
Post a brief description of general healthcare technology trends, particularly related to data/information you have observed in use in your healthcare organization or nursing practice. Describe any potential challenges or risks that may be inherent in the technologies associated with these trends you described. Then, describe at least one potential benefit and one potential risk associated with data safety, legislation, and patient care for the technologies you described. Next, explain which healthcare technology trends you believe are most promising for impacting healthcare technology in nursing practice and explain why. Describe whether this promise will contribute to improvements in patient care outcomes, efficiencies, or data management. Be specific and provide examples.
By Day 6 of Week 6
Respond to at least two of your colleagues* on two different days, offering additional/alternative ideas regarding opportunities and risks related to the observations shared.
*Note: Throughout this program, your fellow students are referred to as colleagues.
Week 6 Assignment: Literature Review: The Use of Clinical Systems to Improve Outcomes and Efficiencies
New technology—and the application of existing technology—only appears in healthcare settings after careful and significant research. The stakes are high, and new clinical systems need to offer evidence of positive impact on outcomes or efficiencies.
Nurse informaticists and healthcare leaders formulate clinical system strategies. As these strategies are often based on technology trends, informaticists and others have then benefited from consulting existing research to inform their thinking.
In this Assignment, you will review existing research focused on the application of clinical systems. After reviewing, you will summarize your findings.
To Prepare:
- Review the Resources and reflect on the impact of clinical systems on outcomes and efficiencies within the context of nursing practice and healthcare delivery.
- Conduct a search for recent (within the last 5 years) research focused on the application of clinical systems. The research should provide evidence to support the use of one type of clinical system to improve outcomes and/or efficiencies, such as “the use of personal health records or portals to support patients newly diagnosed with diabetes.”
- Identify and select 4 peer-reviewed research articles from your research.
- For information about annotated bibliographies, visit https://academicguides.waldenu.edu/writingcenter/assignments/annotatedbibliographies
The Assignment: (4-5 pages not including the title and reference page)
In a 4- to 5-page paper, synthesize the peer-reviewed research you reviewed. Format your Assignment as an Annotated Bibliography. Be sure to address the following:
- Identify the 4 peer-reviewed research articles you reviewed, citing each in APA format.
- Include an introduction explaining the purpose of the paper.
- Summarize each study, explaining the improvement to outcomes, efficiencies, and lessons learned from the application of the clinical system each peer-reviewed article described. Be specific and provide examples.
- In your conclusion, synthesize the findings from the 4 peer-reviewed research articles.
- Use APA format and include a title page.
- Use the Safe Assign Drafts to check your match percentage before submitting your work.
By Day 7 of Week 8
Submit your completed Assignment.
NURS 6051 Week 9 Discussion: The Inclusion of Nurses in the Systems Development Life Cycle
In the media introduction to this module, it was suggested that you as a nurse have an important role in the Systems Development Life Cycle (SDLC). With a focus on patient care and outcomes, nurses may not always see themselves as contributors to the development of new systems. However, as you may have observed in your own experience, exclusion of nurse contributions when implementing systems can have dire consequences.
In this Discussion, you will consider the role you might play in systems development and the ramifications of not being an active participant in systems development.
To Prepare:
- Review the steps of the Systems Development Life Cycle (SDLC) as presented in the Resources.
- Reflect on your own healthcare organization and consider any steps your healthcare organization goes through when purchasing and implementing a new health information technology system.
- Consider what a nurse might contribute to decisions made at each stage of the SDLC when planning for new health information technology.
By Day 3 of Week 9
Post a description of what you believe to be the consequences of a healthcare organization not involving nurses in each stage of the SDLC when purchasing and implementing a new health information technology system. Provide specific examples of potential issues at each stage of the SDLC and explain how the inclusion of nurses may help address these issues. Then, explain whether you had any input in the selection and planning of new health information technology systems in your nursing practice or healthcare organization and explain potential impacts of being included or not in the decision-making process. Be specific and provide examples.
By Day 6 of Week 9
Respond to at least two of your colleagues* on two different days, by offering additional thoughts regarding the examples shared, SDLC-related issues, and ideas on how the inclusion of nurses might have impacted the example described by your colleagues.
*Note: Throughout this program, your fellow students are referred to as colleagues.
Example Essay On The Inclusion of Nurses in the Systems Development Life Cycle
The healthcare sector continues to face several unique challenges. There has been an increased demand for enhanced and secure data management methods. There have been many significant advancements in computer technology in the modern world. The use of computers has become ubiquitous across many if not all, sectors. In the healthcare industry, computer technology has revolutionized many practices, increasing efficiency, patient outcomes, communication, and the overall satisfaction levels of healthcare providers and their clients or patients (Mcgonigle & Mastrian, 2022). Nurses form the majority of healthcare providers.
Furthermore, nurses have the most contact and communication with patients. Risling and Risling (2020) assert that nurses play vital roles in decision-making regarding the use of information systems in the healthcare industry and the Systems Development Life Cycle (SDLC). The SDLC is a cycle involving planning, analyzing, designing, implementing, and maintaining healthcare information systems and nursing informatics (Wang et al., 2019). This paper analyzes the potential repercussions and consequences for organizations that fail to involve nurses in each stage of the SDLC when implementing or purchasing new health information systems.
Planning Phase
The planning phase is an integral part of any project. Effective planning ensures that the subsequent steps run smoothly and ensures the achievement of top-notch results despite the complexity or difficulty of a project. Organizations must conduct a feasibility analysis before implementing or purchasing a new information system. Failing to include nurses in this vital step could lead to developing an ineffective system that does not address all the healthcare organizations. Nurses form most of the healthcare team and spend the most time with patients.
Analysis Phase
The analysis phase entails evaluating a technology to see what works and what does not. In this phase, the project designers examine the requirements and workflows of the new system. Nurses manage patients and also collaborate with other healthcare professionals. Therefore, they understand all healthcare providers’ responsibilities and workflow in patient care. Failing to involve nurses in the analysis phase could lead to developing systems deficient in positive workflows and failing to address all the healthcare needs.
Design Phase
This stage has various processes, including the essentiality of data and program visualization. It also includes how combining different aspects of a system can lead to productive and successful outcomes. Nurses are involved at every point of patient care and know the most essential and non-essential patient data at every interaction phase. Failing to involve nurses in the design phase could lead to a system that is inefficient to use, time-consuming, and fails to collect all essential patient information at different stages.
Implementation and Evaluation Phase
The system developers collaborate with nurses and other healthcare members to bring the new system to life. Failing to involve nurses in this stage can lead to an unhelpful and unfamiliar system that nurses perceive as non-essential to patient care. Hosein et al. (2019) note that nurses dramatically improve healthcare services when they adopt new health information systems. Failing to involve nurses in evaluating the effectiveness of a system can lead to gathering unreliable data that does not identify possible gaps.
The maintenance phase involves continuous user support, which may involve system changes. Failing to involve nurses can lead to long delays in implementing system changes, delaying essential patient care.
I have not yet been involved in developing or selecting a health information technology system. However, there might be some upcoming projects soon. I am positive that I will be involved in the projects. This paper has shed light on the essence of involving nurses in the different phases of the SDLC.
References
Hosein, B., Luo, J., & Karami, M. (2019). Adoption of Hospital Information System Among Nurses: A Technology Acceptance Model Approach. Acta Informatica Medica, 27(5), 305. https://doi.org/10.5455/aim.2019.27.305-310
Mcgonigle, D., & Mastrian, K. G. (2022). Nursing informatics and the foundation of knowledge (5th ed.). Jones & Bartlett Learning.
Risling, T. L., & Risling, D. E. (2020). Advancing nursing participation in user-centered design. Journal of Research in Nursing, 25(3), 226–238. https://doi.org/10.1177/1744987120913590
Wang, J., Gephart, S. M., Mallow, J., & Bakken, S. (2019). Models of collaboration and dissemination for nursing informatics innovations in the 21st century. Nursing Outlook, 67(4), 419–432. https://doi.org/10.1016/j.outlook.2019.02.003
NURS 6051 Week 10 Portfolio Assignment: The Role of the Nurse Informaticist in Systems Development and Implementation
Assume you are a nurse manager on a unit where a new nursing documentation system is to be implemented. You want to ensure that the system will be usable and acceptable for the nurses impacted. You realize a nurse leader must be on the implementation team.
To Prepare:
- Review the steps of the Systems Development Life Cycle (SDLC) and reflect on the scenario presented.
- Consider the benefits and challenges associated with involving a nurse leader on an implementation team for health information technology.
The Assignment: (2-3 pages not including the title and reference page)
In preparation of filling this role, develop a 2- to 3-page role description for a graduate-level nurse to guide his/her participation on the implementation team. The role description should be based on the SDLC stages and tasks and should clearly define how this individual will participate in and impact each of the following steps:
- Planning and requirements definition
- Analysis
- Design of the new system
- Implementation
- Post-implementation support
- Use APA format and include a title page and reference page.
- Use the Safe Assign Drafts to check your match percentage before submitting your work.
By Day 7 of Week 10
Submit your completed Role Description.
NURS 6051 Week 11 Assignment: Policy/Regulation Fact Sheet
As a professional nurse, you are expected to apply your expertise to patient care. On occasion, you will also be expected to share that expertis
READ MORE >>
Assignment: Select a healthcare facility or serviceAssignment: Select a healthca ...
Assignment: Select a healthcare facility or service
Assignment: Select a healthcare facility or service
- Select a healthcare facility or service (e.g., hospital, physician practice, long-term care facility, ambulance service, pharmacy, or skilled nursing facility).
- Identify and read one recently proposed or enacted state or federal legislation that impacts your selected healthcare facility or service.
- Write an 800-word policy brief on the legislation’s effects on your selected facility or service and the state’s population.
Use the following structure when putting together your policy brief:
- Title
- Executive Summary (225 words)
- Recommendations
- Introduction
- State recommendation again
- Body
- Overview of problem
- Review of relevant research
- Application of research results
- Policy Implications
- Conclusion
Cite 3 reputable references to support your assignment (e.g., trade or industry publications, government or agency websites, scholarly works, or other sources of similar quality).
ORDER THROUGH BOUTESSAY
Assignment: Select a healthcare facility or service Instructions
Read over your paper – in silence and then aloud – before handing it in and make corrections as necessary. Often it is advantageous to have a friend proofread your paper for obvious errors. Handwritten corrections are preferable to uncorrected mistakes.
Use a standard 10 to 12 point (10 to 12 characters per inch) typeface. Smaller or compressed type and papers with small margins or single-spacing are hard to read. It is better to let your essay run over the recommended number of pages than to try to compress it into fewer pages.
Likewise, large type, large margins, large indentations, triple-spacing, increased leading (space between lines), increased kerning (space between letters), and any other such attempts at “padding” to increase the length of a paper are unacceptable, wasteful of trees, and will not fool your professor.
The paper must be neatly formatted, double-spaced with a one-inch margin on the top, bottom, and sides of each page. When submitting hard copy, be sure to use white paper and print out using dark ink. If it is hard to read your essay, it will also be hard to follow your argument.
ADDITIONAL INSTRUCTIONS FOR THE CLASS
Discussion Questions (DQ)
- Initial responses to the DQ should address all components of the questions asked, include a minimum of one scholarly source, and be at least 250 words.
- Successful responses are substantive (i.e., add something new to the discussion, engage others in the discussion, well-developed idea) and include at least one scholarly source.
- One or two sentence responses, simple statements of agreement or “good post,” and responses that are off-topic will not count as substantive. Substantive responses should be at least 150 words.
- I encourage you to incorporate the readings from the week (as applicable) into your responses.
Weekly Participation
- Your initial responses to the mandatory DQ do not count toward participation and are graded separately.
- In addition to the DQ responses, you must post at least one reply to peers (or me) on three separate days, for a total of three replies.
- Participation posts do not require a scholarly source/citation (unless you cite someone else’s work).
- Part of your weekly participation includes viewing the weekly announcement and attesting to watching it in the comments. These announcements are made to ensure you understand everything that is due during the week.
APA Format and Writing Quality
- Familiarize yourself with APA format and practice using it correctly. It is used for most writing assignments for your degree. Visit the Writing Center in the Student Success Center, under the
- Resources tab in LoudCloud for APA paper templates, citation examples, tips, etc. Points will be deducted for poor use of APA format or absence of APA format (if required).
- Cite all sources of information! When in doubt, cite the source. Paraphrasing also requires a citation.
- I highly recommend using the APA Publication Manual, 6th edition.
Use of Direct Quotes
- I discourage overutilization of direct quotes in DQs and assignments at the Masters’ level and deduct points accordingly.
- As Masters’ level students, it is important that you be able to critically analyze and interpret information from journal articles and other resources. Simply restating someone else’s words does not demonstrate an understanding of the content or critical analysis of the content.
- It is best to paraphrase content and cite your source.
LopesWrite Policy
- For assignments that need to be submitted to LopesWrite, please be sure you have received your report and Similarity Index (SI) percentage BEFORE you do a “final submit” to me.
- Once you have received your report, please review it. This report will show you grammatical, punctuation, and spelling errors that can easily be fixed. Take the extra few minutes to review instead of getting counted off for these mistakes.
- Review your similarities. Did you forget to cite something? Did you not paraphrase well enough? Is your paper made up of someone else’s thoughts more than your own?
- Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for tips on improving your paper and SI score.
Late Policy
- The university’s policy on late assignments is 10% penalty PER DAY LATE. This also applies to late DQ replies.
- Please communicate with me if you anticipate having to submit an assignment late. I am happy to be flexible, with advance notice. We may be able to work out an extension based on extenuating circumstances.
- If you do not communicate with me before submitting an assignment late, the GCU late policy will be in effect.
- I do not accept assignments that are two or more weeks late unless we have worked out an extension.
- As per policy, no assignments are accepted after the last day of class. Any assignment submitted after midnight on the last day of class will not be accepted for grading.
Communication
Communication is so very important. There are multiple ways to communicate with me:
- Questions to Instructor Forum: This is a great place to ask course content or assignment questions. If you have a question, there is a good chance one of your peers does as well. This is a public forum for the class.
- Individual Forum: This is a private forum to ask me questions or send me messages. This will be checked at least once every 24 hours.
READ MORE >>
